Abstract
Objectives
Study formal and informal care of community-living older people in the Swedish National study of Aging and Care (SNAC).
Design
Cross-sectional, population based cohort.
Setting
Three areas in Sweden: Municipality of Nordanstig, Stockholm and Skåne County.
Participants
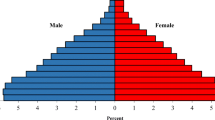
3,338 persons ≥72 years.
Measurements
Patterns and amounts of informal and formal care by cognition and area of residence.
Results
73% received no care; 14% formal care; and 17% informal care (7% received both). In the whole study population, including those who used no care, individuals in small municipalities received 9.6 hours of informal care/month; in mid-size municipalities, 6.6; and in urban areas, 5.6. Users of informal care received 33.1 hours of informal care/month in small municipalities, 54.6 in mid-size municipalities and 36.1 in urban areas. Individuals with cognitive impairment received 14.1 hours of informal care/month, 2.7 times more than people with no/slight impairment. In the whole study population, individuals in small municipalities received an average of 3.2 hours of formal care/month; in mid-size municipalities 1.4; and in urban areas, 2.6. Corresponding figures for formal care users were 29.4 hours in small municipalities, 13.6 in mid-size municipalities and 16.7 in urban areas. Formal care users received 7.1 hours, and informal care users, 5.9 hours for each hour/month received by people in the study population as a whole.
Conclusions
More informal than formal care was provided. Informal care is more frequent in small municipalities than urban areas and for those with than without cognitive impairment. The relationship between data on the whole population and the data on users or care indicates that population-based data are needed to avoid overestimates of care.





Similar content being viewed by others
References
Nordberg G. Formal and informal care in an urban and rural elderly population. Who? When? What? Stockholm: Karolinska Institutet; 2007.
McDaid D. Estimating the costs of informal care for people with Alzheimer’s disease: methodological and practical challenges. Int J Geriatr Psychiatry. 2001 Apr;16(4):400–5.
Nordberg G, von Strauss E, Kareholt I, Johansson L, Wimo A. The amount of informal and formal care among non-demented and demented elderly personsresults from a Swedish population-based study. Int J Geriatr Psychiatry. 2005 Aug 22;20(9):862–71.
SBU. Dementia. A systematic review. Stockholm: Staten beredning för medicinsk utvärdering (SBU) (The Swedish Council on Technology Assessment in Health Care) 2008. Report No.: 172E/1-3.
Wimo A, Sjolund B, Skoldunger A, Johansson L, Nordberg G, von Strauss E. Incremental patterns in the amount of informal and formal care among non-demented and demented elderly persons results from a 3-year follow-up population-based study. Int J Geriatr Psychiatry. 2011 Jul 26;26(Jan):56–64.
Mittelman MS, Haley WE, Clay OJ, Roth DL. Improving caregiver well-being delays nursing home placement of patients with Alzheimer disease. Neurology. 2006 Nov 14;67(9):1592–9.
Andren S, Elmstahl S. Effective psychosocial intervention for family caregivers lengthens time elapsed before nursing home placement of individuals with dementia: a five-year follow-up study. Int Psychogeriatr. 2008 Dec;20(6):1177–92.
Lagergren M, Fratiglioni L, Hallberg IR, Berglund J, Elmstahl S, Hagberg B, et al. A longitudinal study integrating population, care and social services data. The Swedish National study on Aging and Care (SNAC). Aging Clin Exp Res. 2004 Apr;16(2):158–68.
SKL. Kommungruppsindelning 1999-2004. Stockholm: Sveriges Kommuner och Landsting(SKL) in English: Swedish Association of Local Authorities and Regions (SALAR); 2009 [updated 2009; cited 2013 2013-06-11]; Available from: http://www.skl.se/kommuner_och_landsting/fakta_om_kommuner/kommungruppsindelning/aldre_indelning.
Folstein MF, Folstein SE, McHugh PR. «Mini-mental state». A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975 Nov;12(3):189–98.
Fratiglioni L, Viitanen M, Backman L, Sandman PO, Winblad B. Occurrence of dementia in advanced age: the study design of the Kungsholmen Project. Neuroepidemiology. 1992;11 Suppl 1:29–36.
Wimo A, Wetterholm AL, Mastey V, Winblad B. Evaluation of the resource utilization and caregiver time in Anti-dementia drug trials-a quantitative battery. In: Wimo A, Jonsson B, Karlsson G, Winblad B, editors. The Health Economis of dementia. London: John Wiley & Sons; 1998. p. 465–99.
Wimo A, Nordberg G. Validity and reliability of assessments of time Comparisons of direct observations and estimates of time by the use of the resource utilization in dementia (RUD)-instrument. Arch Gerontol Geriatr. 2006 Jun 12;44:71–81.
Wimo A, Jonsson L, Zbrozek A. The Resource Utilization in Dementia (RUD) instrument is valid for assessing informal care time in community-living patients with dementia. J Nutr Health Aging. 2010 Aug;14(8):685–90.
Mesterton J, Wimo A, By A, Langworth S, Winblad B, Jonsson L. Cross Sectional Observational Study on the Societal Costs of Alzheimer’s Disease. Curr Alzheimer Res. 2010 Nov 26;7:358–67.
Socialstyrelsen. Vård och omsorg om äldre 2002 (tabellbilaga) (Current developments in care of the elderly in Sweden in 2002) (in Swedish with English summary)). Stockholm; 2003. Report No.: 2003-131-1 Contract No.: Document Number.
van den Berg B, Spauwen P. Measurement of informal care: an empirical study into the valid measurement of time spent on informal caregiving. Health Econ. 2006 May;15(5):447–60.
Zhu CW, Scarmeas N, Torgan R, Albert M, Brandt J, Blacker D, et al. Clinical features associated with costs in early AD: baseline data from the Predictors Study. Neurology. 2006 Apr 11;66(7):1021–8.
Cavallo MC, Fattore G. The economic and social burden of Alzheimer disease on families in the Lombardy region of Italy. Alzheimer Dis Assoc Disord. 1997;11(4):184–90.
Feldman H, Gauthier S, Hecker J, Vellas B, Emir B, Mastey V, et al. Efficacy of donepezil on maintenance of activities of daily living in patients with moderate to severe Alzheimer’s disease and the effect on caregiver burden. J Am Geriatr Soc. 2003 Jun;51(6):737–44.
Gustavsson A, Jonsson L, Rapp T, Reynish E, Ousset PJ, Andrieu S, et al. Differences in resource use and costs of dementia care between European countries: baseline data from the ICTUS study. J Nutr Health Aging. 2010 Aug;14(8):648–54.
Van Houtven CH, Oddone EZ, Weinberger M. Informal and formal care infrastructure and perceived need for caregiver training for frail US veterans referred to home and community-based services. Chronic Illn. 2010 Mar;6(1):57–66.
Daatland SO. Ageing, families and welfare systems: comparative perspectives. Z Gerontol Geriatr. 2001 Feb;34(1):16–20.
Moore MJ, Zhu CW, Clipp EC. Informal costs of dementia care: estimates from the National Longitudinal Caregiver Study. J Gerontol B Psychol Sci Soc Sci. 2001 Jul;56(4):S219–28.
Moise P, Schwarzinger M, Um M-Y, al. e. Dementia care in 9 OECD countries. A comparative analysis. Paris: OECD; 2004. Report: OECD Health Working Papers No 13.
Campbell P, Wright J, Oyebode J, Job D, Crome P, Bentham P, et al. Determinants of burden in those who care for someone with dementia. Int J Geriatr Psychiatry. 2008 Oct;23(10):1078–85.
Coduras A, Rabasa I, Frank A, Bermejo-Pareja F, Lopez-Pousa S, Lopez-Arrieta JM, et al. Prospective one-year cost-of-illness study in a cohort of patients with dementia of Alzheimer’s disease type in Spain: the ECO study. J Alzheimers Dis. Jan;19(2):601-15.
Kumamoto K, Arai Y, Zarit SH. Use of home care services effectively reduces feelings of burden among family caregivers of disabled elderly in Japan: preliminary results. Int J Geriatr Psychiatry. 2006 Feb;21(2):163–70.
Kang IO, Lee SY, Kim SY, Park CY. Economic cost of dementia patients according to the limitation of the activities of daily living in Korea. Int J Geriatr Psychiatry. 2007 Jul;22(7):675–81.
ADI. World Alzheimer Report 2009. London: ADI; 2009.
Lien WC, Chang JH, Guo NW, Lin YC, Hsieh PC, Kuan TS (2015) Determinants of Perceived Physical Environment Barriers among Community-Dwelling Elderly in Taiwan. J Nutr Health Aging 19, 575–82.
Wham CA, Teh R, Moyes S, Dyall L, Kepa M, Hayman K, Kerse N (2015) Health and Social Factors Associated with Nutrition Risk: Results from Life and Living in Advanced Age: A Cohort Study in New Zealand (LiLACS NZ). J Nutr Health Aging 19, 637–45.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wimo, A., Elmståhl, S., Fratiglioni, L. et al. Formal and informal care of community-living older people: A population-based study from the Swedish National study on Aging and Care. J Nutr Health Aging 21, 17–24 (2017). https://doi.org/10.1007/s12603-016-0747-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-016-0747-5