Abstract
Background
Characterization of the main features of pre-frailty may contribute to better understanding the mechanisms involved in the development of frailty.
Objective
To characterize the pre-frail population consulting in primary care centres in Mataró (Catalonia, Spain), to describe the Fried’s frailty criteria for this population and to identify the main associated factors.
Design
Cross-sectional study.
Setting
Three primary care centres in Catalonia.
Participants
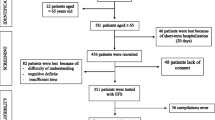
Pre-frail subjects recruited from among persons aged 70 years and older consulting primary care centres and screened for frailty according to Fried’s criteria.
Measurements
Clinical, nutritional and functional data.
Results
Frailty prevalence of 31.0% and pre-frailty prevalence of 49.0% were observed. Comorbidity was not especially frequent among elderly individuals classified as pre-frail (except for diabetes with 35.8% prevalence). Functional status and nutritional status were both reasonably satisfactory in pre-frail subjects with mean Barthel score of 98 points and 91% classified as well nourished. Among pre-frail subjects, 35% were obese (body mass index>30); 75% reported pain; 12% had an accidental fall in the previous three months; and the mean number of medications ingested was 6.2. Weakness was the most prevalent frailty criterion (70%), followed by slowness (30%). Weakness was associated with age in men and with pain in women. Poor physical activity was associated with pain.
Conclusions
Pre-frailty is very common among elderly subjects consulting primary care centres. Weakness, slowness, diabetes, pain and polypharmacy should alert healthcare professionals to the onset of a frailty process.



Similar content being viewed by others
References
Morley J, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, et al. Frailty consensus: a call to action. Journal of the American Medical Directors Association 2013; 14: 392–7.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. Journals of Gerontology Series A: Biological Sciences and Medical Sciences 2001; 56 (3): M146–M156.
Vellas B, Cestac P, Morley JE. Implementing frailty into clinical practice: we cannot wait. J Nutr Health Ageing 2012; 16 (7): 599–600.
Rockwood K, Song X, MacKnight C et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005; 173: 489–95.
Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging 2012; 16: 601–8.
Steverink N, Slaets JPJ, Schuurmans H, Lis van M. Measuring frailty: development and testing of the Groningen frailty indicator(GFI). Gerontologist 2001; 41: 236–7.
Searle S, Mitnitski A, Gahbauer E, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatr2008; 8: 24.
Gill TM, Gahbauer EA, Allore HG, Han L. Transitions between frailty states among community-living older persons. Arch Intern Med 2006; 166: 418–23.
Walston JD. Frailty–and its dangerous effects-might be preventable. Ann In Med 2004; 141: 489–92.
Clegg A, Young J, Ilife S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet 2013; 381: 752–62.
Fernandez-Garrido J, Ruiz-Ros V, Buigues C, Navarro-Martínez R, Cauli O. Clinical features of pre-frail older individuals and emerging peripheral biomarkers: A systematic review. Arch GerontolGeriat 2014. http://dx.doi.org/10.1016/j. archger.2014.02.008
Smit E, Winter-Stone KM, Loprinzi PD, Tang AM, Crespo CJ. Lower nutritional status and higher food insufficiency in frail older US adults. British Journal of Nutrition 2013; 110: 172–8.
Shardell M, D’Adamo C, Alley DE, Miller RR, Hicks GE, Milaneschi Y et al. Serum 25-hydroxivitamin D, transitions between frailty states, and mortality in older adults: The invecchiare in Chianti study. Journal of the American Geriatrics Society 2012; 60 (2): 256–64.
Santos-Egimann B, Cuenoud P, Spagnoli J, Junod J. Prevalence of frailty in middleaged and older community dwelling Europeans living in 10 countries. Journals of Gerontology Series A: Biologica Sciences and Medical Sciences 2009; 64A (6): 675–81.
Foster A, et al. Rehabilitation for older people in long term care. Cochrane database of systematic reviews. 2009, 1 (CD004294).
Puig-Domingo M, Serra-Prat M, Merino MJ, Pubill M, Burdoy E, Papiol M, et al. Muscle strength in the Mataró Ageing study participants and its relationship to successful ageing. Ageing ClinExp Res 2008; 20: 439–46.
Kalyani RR, Saudek CD, Brancati FL, Selvin E. Association of diabetes, comorbidities, and A1C with functional disability in older adults: results from the National Health and Nutrition Examination Survey (NHNES), 1999-206. Diabetes Care 2010; 33: 1055–60.
Park SW, Goodpaster BH, Lee JS, and the Health, Ageing, and Body composition study. Excessive loss of skeletal muscle mass in older adults with type 2 diabetes. Diabetes Care 2009; 32: 1993–7.
Park SW, Goodpaster BH, Strotmeyer ES and the Health, Ageing, and Body composition study. Accelerated loss of skeletal muscle strength in older adults with type 2 diabetes: the health, ageing, and body composition study. Diabetes Care 2007; 30: 1507–12.
Barzilay JI, Cotsonis GA, Walston J, and the Health ABC study. Insuline resistance is associated with decreased quadriceps muscle strength in non diabetic adults aged ≥70 years. Diabetes care 2009; 32: 736–8.
Kelley DE, He J, Menshikova EV, Ritov VB. Dysfunction of mitochondria in human skeletal muscle in type 2 diabetes. Diabetes 2002; 51: 2944–50.
Kalyani RR, Corriere M, Ferrucci L. Age-related and disease-related muscle loss: the effect of diabetes, obesity, and other diseases. Lancet Diabetes Endocrinol 2014; 2 (10): 819–29.
Franchi C, Tettamanti M, Pasina L, Djignefa CD, Fortino I, Bortolotti A, et al. Changes in drug prescribing to italian community-dwelling elderly people: the EPIFARM-Elderly project 2000-2010. Eur J ClinPharmacol 2014; 70 (4): 437–43.
Richardson K, Bennett K, Kenny RA. Polypharmacy including falls risk-increasing medications and subsequent falls in community-dwelling middle-aged and older adults. Age Ageing 2014 pii: afu141
Beers MH. Explicit criteria for determining potentially inappropriate medication use by the elderly. An update. Arch Intern Med 1997;157:1531–6.
Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J ClinPharmacolTher. 2008 Feb;46(2):72–83.
Naugler CT, Brymer C, Stolee P, Arcese ZA. Development and validation of an improving prescribing in the elderly tool. Can J ClinPharmacol. 2000 Summer;7(2):103–7
Wenger NS, Shekelle PG. Assessing care of vulnerable elders: ACOVE Project overview. Ann Intern Med. 2001 Oct 16;135(8 Pt 2):642–6.
Danon Hersch N, Rodondi N, Spagnoli J, Santos-Eggimann B. Prefrailty and chronic morbidity in the youngest old: an insight from the Lausanne cohort Lc65. Journal American Geriatrics Society 2012; 60 (9): 1687–94.
Xue Q, Bandeen-Roche K, Varadhan R, Zhou J, Fried LP. Initial manifestations of frailty criteria and the development of frailty phenotype in the Women’s Health and Ageing Study II. Journalñs of Gerontology Series A: Biological Sciences and Medical Sciences 2008; 63 (9): 984–90.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Serra-Prat, M., Sist, X., Saiz, A. et al. Clinical and functional characterization of pre-frailty among elderly patients consulting primary care centres. J Nutr Health Aging 20, 653–658 (2016). https://doi.org/10.1007/s12603-016-0684-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-016-0684-3