Abstract
The purpose of the present study is to evaluate the vital prognoses of elderly people in their mid-eighties living in a group home (GH) compared to age- and sex-matched outpatient clinic (OPC) in an observational study conducted over 6 years. We investigated the association between mortality and general, cardiac, and nutritional parameters, including eicosapentaenoic acid (EPA) in 54 GH residents (83 ± 8 years old) and 57 OPC attendees (83 ± 5 years old). Kaplan–Meier curves and Cox proportional hazard ratio analyses were used to assess the association between EPA drug administration and mortality in the GH residents and OPC attendees, respectively. The 54 GH residents had higher mortality and poorer nutritional states, as indicated by lower EPA/arachidonic acid values (median 0.20 vs 0.55, p < 0.001), and BMI under the condition without EPA drug administration (1800 mg daily) than did the OPC group. The significant factors that differed between survivors and deceased in the GH residents and OPC attendees were nutritional and cardiac factors. Cox proportional hazard ratio analysis confirmed that a possible determinant of the prognosis was a lower incidence of EPA drug administration and lower hemoglobin in GH. Kaplan–Meier curves and Cox proportional hazard ratio analyses revealed that EPA drug administration significantly reduced the relative mortality by 82 % in the GH residents (p < 0.001) but not in the OPC attendees. The vital prognosis in individuals from GHs was potentially improved by EPA drug administration, which was not the case in the OPC group; however, further prospective studies are needed.
Similar content being viewed by others
Introduction
Japan will soon become a very old society, thus providing an opportunity to develop a model care system for the elderly. We are interested in achieving better vital prognoses in the elderly. Several epidemiological cohort studies have reported useful clinical indicators of survival, including functional abilities such as gait speed [1–3]. Group homes (GH) in Japan are care services where five to nine residents live together as though they were in their own home. In these facilities, elderly individuals with poor activities of daily living (ADL) or impaired cognitive function live together, and medical, nursing and nutritional care is collaboratively provided [4, 5].
However, vital prognoses and clinical aspects in GH residents have not been sufficiently reported. Recently, we reported the cause of eicosapentaenoic acid (EPA) deficiency in GHs and an improvement in the severity of supraventricular arrhythmias and changes in lipids in response to EPA therapy [6].
To elucidate the possible determinants of vital prognosis in GH residents, we investigated the association between mortality and general, nutritional, and cardiac parameters, including the polyunsaturated fatty acid levels, between GH residents and outpatient clinic (OPC) attendees.
Methods
Subjects
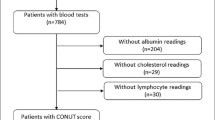
We recruited 54 elderly subjects (83 ± 8, 63–97 years old) in GHs and 57 elderly patients (83 ± 8, 75–95 years old) who regularly visited the Department of Cardiology OPC at the city hospital (Tokyo, Japan) between January 2010 and December 2015. The entry criteria for this study were as follows. For GH residents, the inclusion criteria were all residents who stayed in a GH in the period described above, except for 4 patients who moved from a GH to another care facility. For OPC attendees, the entry criteria were all patients over 75 years of age (83 ± 8, 75–95 years old) who visited the Department of Cardiology at the city hospital and saw the corresponding author for more than 4 months in the period described above; their general parameters are shown in Table 1, and electrocardiograms were performed. The same physician (the corresponding author) treated all 111 enrolled patients from both the OPC and GH groups.
Protocol
In 54 GH residents and 57 OPC patients in their mid-eighties, we examined the general, nutritional, and cardiac parameters listed below (see measurement variables). To determine the possible determinants of clinical characteristics for elderly individuals in their mid-eighties in GHs, we compared the clinical findings of the 54 GH residents to those of 57 control OPC attendees using a non-parametric test. We also compared the clinical variables between 27 survivors and 27 deceased participants of the 54 GH residents and between 43 survivors and 14 deceased participants of the 57 OPC attendees using a non-parametric test. At nearly the mid-point of the observation period (2013), the physician extended EPA drug therapy (1800 mg daily) using a criterion of EPA/AA < 0.465 [7]. The effects of EPA drug administration on vital prognosis were evaluated by Kaplan–Meier curves and Cox proportional hazard ratios between the subjects with and without EPA drug treatment in the GH residents and OPC attendees, respectively.
The Institutional Review Board for Clinical Research of Tokai University (Hospital) approved this study.
Measurement of variables
General parameters, blood chemistry data and cardiac parameters
The general parameters included the body mass index (BMI), systolic blood pressure (SBP), diastolic blood pressure (DBP), and cognitive function, as evaluated using the Mini-Mental State Examination (MMSE), which was divided into 3 levels (MMSE 24–30:1, MMSE 10–23:2, and MMSE 0–9:3). ADL and medications (including dosing information), such as the EPA drug (EPADEL, MOCHIDA PHARMACEUTICAL CO., LTD. Tokyo, Japan), antithrombotic agents, antihypertensive agents, diuretics or inotropic drugs, antianginal drugs, anti-dementia agents, hypoglycemic agents, dyslipidemia medications and antiarrhythmic agents, were recorded. Blood chemistry data included the serum levels of total protein (TP); albumin (Alb); hemoglobin (Hb); unsaturated fatty acid, EPA, docosahexaenoic acid (DHA), and arachidonic acid (AA); lipid [low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and triglycerides]; glycosylated hemoglobin (HbA1c) values; and serum and other blood sample data, including renal function parameters [blood urea nitrogen (BUN) and serum creatinine (Cre)], liver function parameters [serum aspartate aminotransferase (AST) and alanine aminotransferase (ALT)], and serum level of N-terminal pro-brain natriuretic peptide (NT-proBNP). Cardiac parameters included the cardiothoracic ratio (CTR) on a chest-X ray, severity of supraventricular and ventricular arrhythmias (SVA and PVC) and 12-lead electrocardiogram (ECG) findings, such as left ventricular hypertrophy, left atrial overload, left axis deviation, right axis deviation, atrial fibrillation, and left and right bundle branch blocks.
The blood chemistry data, including the TP, Alb, Hb, fatty acids, lipids, HbA1c, and both renal and liver function, and NT-proBNP, were analyzed using a previously described method [23]. The severity of SVA and PVC was examined on a Holter electrocardiogram. We defined the SVA severity based on the following 6 categories: 1, no arrhythmia; 2, supraventricular extrasystole (a single or couplet); 3, 3–29 supraventricular tachycardia (SVT); 4, ≥ 30 SVT; 5, paroxysmal atrial fibrillation (Af); and 6, sustained Af. The PVC severity was classified as follows: 1, no arrhythmia; 2, a single arrhythmia; 3, ≥ couplet ventricular premature contraction (PVC); 4, 3–29 PVC; 5, ≥ 30 PVC, and 6, ventricular fibrillation.
Statistical analyses
We used the SPSS software (version 23, IBM, Armonk, New York, USA) for all statistical analyses. The chi-squared test was used to compare the categorical values. The Mann–Whitney U test was used to compare continuous variables.
To determine the EPA drug therapy for predicting the long-term prognosis in GH residents, the Kaplan–Meier curves and Cox proportional hazard ratio were applied in the GH and OPC groups, respectively.
Results
Comparison between the GH residents and OPC attendees
As shown in Tables 1, 2 and 3, comparing the 54 GH residents and 57 OPC attendees, the elderly in the GH group exhibited increased mortality (p < 0.01) as well as poor nutritional states, as indicated by EPA/AA (p < 0.01), lower BMI (p < 0.01), and HbA1c (p < 0.01), under the condition without EPA drug administration. In addition to these parameters, lower SBP (p < 0.01), impaired cognitive function (p < 0.01), and reduced ADL scores (p < 0.01) were noted in GH residents compared with OPC attendees.
Comparison of the clinical findings between those who survived and deceased subjects in the GH residents and OPC attendees
The significant factors between survivors and deceased in the GH residents and OPC attendees were nutritional and cardiac factors (Tables 4, 5, 6). Mann–Whitney analysis showed that NT-proBNP was significantly increased in deceased OPC and GH patients. Lower BMI, left axis deviation and an increased incidence of atrial fibrillation were noted in the deceased OPC patients. Reduced TP, reduced Alb, increased HbA1c, reduced Hb, an increased incidence of left atrial overload and minimal changes in DBP were noted in the deceased GH patients who did not receive EPA drug administration (Tables 4, 5, 6). Cox proportional hazard ratio analysis revealed that in addition to EPA drug treatment, the predictive factors for vital prognosis were Hb in the GH residents and a lower BMI and higher incidence of atrial fibrillation in the OPC attendees (Table 7). The EPA levels under the condition without EPA drug administration were not significantly different between the survivors and deceased in both the GH residents and OPC attendees.
Effects of EPA drug administration on vital prognosis in the GH residents and OPC attendees
As shown in Fig. 1, the physician extended EPA drug administration in the GH group in 2013 (from 17 to 88 % of GH residents as a cumulative administration percentage) using the criterion of EPA/AA < 0.465 reported by Ikeya et al. [7]. As shown in Fig. 2a, Kaplan–Meier curves in the GH residents showed that mortality was significantly lower in the residents given EPA than in those without EPA (18 vs 100 %, p < 0.001), indicating a relative reduction of 82 %. In contrast, Kaplan–Meier curves in OPC attendees revealed no significant differences in the attendees with and without EPA (24 vs 25 %, p = 0.658). There was no difference in the plasma EPA levels at baseline between the subjects with and without EPA drug administration in both groups (p = 0.734 in GH residents and p = 0.259 in OPC attendees, respectively; data not shown). Again, Cox proportional hazard ratio analysis confirmed that EPA drug administration was a significant predictive factor of long-term prognosis in GH residents (Table 7).
Discussion
This study showed that GH residents had higher mortality and poorer nutritional states, as indicated by the lower EPA/AA and BMI compared to the OPC attendees. Cox proportional hazard ratio analysis confirmed that the significant factors between survivors and deceased in GH residents and OPC attendees were essentially nutritional and cardiac factors. Additionally, EPA drug administration drastically reduced the relative mortality in GH residents but not in OPC attendees.
The 54 GH residents exhibited increased mortality (p < 0.01) and poorer nutritional states, as indicated by the EPA/AA, lower BMI and HbA1c, with no EPA drug administration (Tables 1, 2, 3). The Cox proportional hazard ratio analysis followed by the Mann–Whitney U test between survivors and deceased subjects in the GH residents and OPC attendees revealed that a lack of EPA drug administration and a lower Hb level were possible determinants of poor vital prognosis in the GH residents. Lower BMI and higher incidence of atrial fibrillation were observed in the OPC attendees (Tables 4, 5, 6, 7). Kaplan–Meier curves showed that EPA drug administration could reduce the mortality in GH residents (Fig. 2a) but not in the OPC attendees (Fig. 2b). All 21 of the patients who did not receive EPA died within the 72-month observation period. Cox proportional hazard ratio analysis, followed by Kaplan–Meier curve analysis, confirmed that EPA drug administration was a significant predictive factor of long-term prognosis in GH residents (Fig. 2a; Table 7).
Fried et al. reported the overall 5-year mortality in the elderly > 65 years of age was 12 % (annual mortality of 2.4 %) [8]. The annual mortalities increased with age as follows: 3.48 % for 75- to 79-year-olds, 5.45 % for 80- to 84-year-olds and 9.66 % for > 85-year-olds. In Japan, the annual mortalities of the elderly groups in 2014 were 2.51 % for those who were 75–79 years of age, 4.55 % for those 80–84 years of age, and 8.18 % for those > 85 years of age [9]. The mortality rates of home-care residents and community residents were 21.5 and 3.9 %, respectively [10].
A lower BMI, Hb, and Alb; hospitalization; and living in a nursing home have been reported as possible risk factors for high mortality in the elderly [7, 11, 12]. Various cardiac abnormalities increased mortality of the elderly [8], who often died from multifactorial diagnoses [13]. We defined acute death as sudden deterioration in life quality within several days in the present study. Fifty-nine percent of the deaths (24 of 41) were attributed to acute deaths. The nine acute deaths in the OPC patients included 2 dissecting aortic aneurysms, 3 strokes, 1 pulmonary embolism and 1 acute myocardial infarction. The remaining 2 patients died suddenly. Five chronic deaths in the OPC patients included 4 chronic congestive heart failure cases and 1 liver disease case. Fifteen acute deaths in GH residents included 2 pneumonias, 2 acute congestive heart failures, and 11 sudden deaths. Twelve chronic deaths in the GH residents included 4 chronic congestive heart failures, 2 pneumonias, and 2 senile decay cases with 4 unknown causes of death. Four of 41 people who died had had various cancers; however, their cancers were not the primary cause of their death.
EPA drug treatment reduced the major coronary events for patients with a history of coronary artery disease [14] and stroke recurrence [15]. All-cause mortality reduction by EPA [16, 17] or EPA and DHA [18] has been reported in a few prospective studies. N-3 fatty acids exerted a preventive effect on arrhythmia and sudden cardiac death [19, 20]. A randomized study reported that n-3 fatty acids reduced the heart rate variability, which is related to sudden death [21, 22].
One hypothesis generated from our results and the previous reports is that the association between cardiac overload and poor nutritional state, including possibly EPA deficiency, might induce sudden cardiac deterioration in the elderly. EPA deficiency in the vascular endothelium and platelets might enhance thrombogenesis [23, 24]. Furthermore, a lack of unsaturated fatty acids in the lipid bi-layers of the atrial and ventricular endocardia might cause arrhythmogeneicity [23]. Transient tachyarrhythmias in patients with hypertensive heart disease or ischemic heart disease can induce a transient reduction in the cardiac output, which possibly causes acute circulatory deterioration. We recently reported that plasma EPA was low in other types of elderly facilities, which was probably due to the low incidence of raw fish consumption and EPA supplementation ameliorated SVAs [6]. Low EPA levels in the elderly subjects among the GH residents probably enhanced the risk of acute cardiovascular events, as described above. There was no difference in EPA/AA between survivors and non-survivors in the group home patients at baseline. Therefore, EPA drug administration reduced the risk of such acute cardiovascular events. In contrast, OPC patients with higher EPA/AA levels at baseline had a lower risk of acute cardiovascular events than did the GH residents.
Our study has several limitations. First, it was a cross-sectional study with a small sample size. Second, there was a time lag in the observation period between EPA treatment, which primarily occurred in the later 3 years in the treatment group and in the earlier 3 years in the non-treatment group. Third, we did not perform autopsies to determine the causes of death.
Conclusion
The vital prognoses of elderly GH residents in their mid-eighties was potentially improved by EPA drug administration. Further prospective studies are required to confirm the role of EPA in vital prognosis.
References
Lubitz J, Cai L, Kramarow E, Lentzner H (2003) Health, life expectancy, and health care spending among the elderly. N Engl J Med 349:1048–1055
Studenski S, Perera S, Patel K et al (2011) Gait speed and survival in older adults. JAMA 305:50–58
Cesari M, Kritchevsky SB, Newman AB et al (2009) Health, aging and body composition study. Added value of physical performance measures in predicting adverse health-related events: results from the health, aging and body composition study. J Am Geriatr Soc 57:251–259
Kobayashi S, Yamamoto-Mitani N, Nagata S, Murashima S (2008) End-of-life care for older adults with dementia living in group homes in Japan. Jpn J Nurs Sci 5:31–40
Yamaguchi T (2005) An empirical study of group home care for the elderly with dementia [in Japanese]. Jpn J Soc Welf 46:100–101
Todoroki K, Ikeya Y, Fukui S et al (2016) Nutrition-dependent eicosapentaenoic acid deficiency in care house residents. Nutrition 32:806–810
Ikeya Y, Fukuyama N, Kitajima W, Ogushi Y, Mori H (2013) Comparison of eicosapentaenoic acid concentrations in plasma between patients with ischemic stroke and control subjects. Nutrition 29:127–131
Fried LP, Kronmal RA, Newman AB et al (1998) Risk factors for 5-year mortality in older adults: the cardiovascular health study. JAMA 279:585–592
Vital statistics. The Ministry of Health, Labour and Welfare (online). http://www.e-stat.go.jp/SG1/estat/NewList.do?tid=000001028897. Accessed 15 Sept 2015
Shah SM, Carey IM, Harris T, DeWilde S, Cook DG (2013) Mortality in older care home residents in England and Wales. Age Ageing 42:209–215
Nelson CL, Elkassabany NM, Kamath AF, Liu J (2015) Low albumin levels, more than morbid obesity, are associated with complications after TKA. Clin Orthop Relat Res 473:3163–3172
van Dijk PT, Mehr DR, Ooms ME et al (2005) Comorbidity and 1-year mortality risks in nursing home residents. J Am Geriatr Soc 53:660–665
Kohn RR (1982) Cause of death in very old people. JAMA 247:2793–2797
Yokoyama M, Origasa H, Matsuzaki M et al (2007) Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis. Lancet 369:1090–1098
Tanaka K, Ishikawa Y, Yokoyama M et al (2008) Reduction in the recurrence of stroke by eicosapentaenoic acid for hypercholesterolemic patients: subanalysis of the JELIS trial. Stroke 39:2052–2058
Lee SH, Shin MJ, Kim JS et al (2009) Blood eicosapentaenoic acid and docosahexaenoic acid as predictors of all-cause mortality in patients with acute myocardial infarction—data from infarction prognosis study (IPS) Registry. Circ J 73:2250–2257
Lindberg M, Saltvedt I, Sletvold O, Bjerve KS (2008) Long-chain n-3 fatty acids and mortality in elderly patients. Am J Clin Nutr 88:722–729
Pottala JV, Garg S, Cohen BE, Whooley MA, Harris WS (2010) Blood eicosapentaenoic and docosahexaenoic acids predict all-cause mortality in patients with stable coronary heart disease: the heart and soul study. Circ Cardiovasc Qual Outcomes 3:406–412
Calò L, Bianconi L, Colivicchi F et al (2005) N-3 fatty acids for the prevention of atrial fibrillation after coronary artery bypass surgery: a randomized, controlled trial. J Am Coll Cardiol 45:1723–1728
Leaf A, Kang J, Xiao Y, Billman GE (2003) Clinical prevention of sudden cardiac death by n-3 polyunsaturated fatty acids and mechanism of prevention of arrhythmias by n-3 fish oils. Circulation 107:2646–2652
Romieu I, Téllez-Rojo MM, Lazo M et al (2005) Omega-3 fatty acid prevents heart rate variability reductions associated with particulate matter. Am J Respir Crit Care Med 172:1534–1540
Holguin F, Téllez-Rojo MM, Lazo M et al (2005) Cardiac autonomic changes associated with fish oil vs soy oil supplementation in the elderly. Chest 127:1102–1107
Calder PC (2012) The role of marine omega-3 (n-3) fatty acids in inflammatory processes, atherosclerosis and plaque stability. Mol Nutr Food Res 56:1073–1080
Adkins Y, Kelley DS (2010) Mechanisms underlying the cardioprotective effects of omega-3 polyunsaturated fatty acids. J Nutr Biochem 21:781–789
Acknowledgments
We thank all research participants and Dr. K. Kitajima (Fureai Machida Hospital), Mr. Yoshinaka (Group Home Ayunosato Sagami), and Ms. Terakado (Group Home Konan). This research was partly supported by Grants-in-Aid for Scientific Research from The Japan Society for the Promotion of Science [Grant No. 23659388] and The Research Funding for Longevity Sciences from the National Center for Geriatrics and Gerontology (NCGG), Japan [Grant No. 22-5 and 25-6].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
About this article
Cite this article
Todoroki, K., Ikeya, Y., Fukui, S. et al. The vital prognosis of elderly adults living in a group home in their mid-eighties. J Physiol Sci 67, 561–568 (2017). https://doi.org/10.1007/s12576-016-0485-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12576-016-0485-9