Abstract
To clarify the characteristics of the thermal control of skin blood flow (SkBF) in individuals with a cold constitution, we examined the cutaneous vasoconstrictor responses in the calf and dorsal foot during whole-body and local skin cooling in young women complaining of chilliness (C group) and young women not suffering from it (N group). During whole-body skin cooling, the vasoconstrictor sensitivity in the dorsal foot, but not in the calf, was greater in the C group than in the N group. The C group also showed greater vasoconstrictor responses in the dorsal foot, but not in the calf, during local skin cooling and the iontophoretic application of norepinephrine. These findings suggest that the C group possesses a specific SkBF controlling system that is characterized by higher adrenergic sensitivity for greater cutaneous vasoconstriction in the distal portion of the lower extremities during cold exposure.
Similar content being viewed by others
Introduction
Exposure to a cool environment increases afferent nerve activity from cold receptors in the cooled skin [1, 2]. The somatosensory information for skin cooling conveys the occurrence of a cold sensation to the cerebral cortex and simultaneously induces cutaneous vasoconstriction via the sympathetic pathway for thermal homeostasis [1, 2]. The reflex vasoconstriction during whole-body skin cooling is known to occur with the release of norepinephrine (NE) and cotransmitters from sympathetic adrenergic nerve terminals [3, 4]. In conjunction with the reflex response, direct cooling of the cutaneous blood vessels evokes vasoconstriction through local mechanisms during whole-body cold exposure.
These cold-induced physiological responses usually exhibit inter-individual differences, even among healthy people. In Japan, even at times when most people do not feel cool under temperate thermal conditions, we often encounter women suffering from severe chilliness of the body, especially in the lower extremities [5–10]. A cold constitution with higher sensitivity to cold sensations is called “hi-e-sho” in Japanese, which has been identified more in females than in males [5, 6, 9]. Women with a cold constitution often feel pain due to the severe cold sensation in a cool environment, and also have minor discomfort (sleeplessness, weariness, lowered power of concentration, etc.) and a tendency to fall ill [11, 12]. Thus, a cold constitution lowers their quality of daily life and heightens their susceptibility to cold syndrome. However, the mechanisms controlling the intense vasoconstriction in those suffering from unusual chilliness are inadequately understood.
Nagashima et al. [13] reported that augmented thermal sensitivity of the body to cold and decreased skin temperature of the fingers during cold exposure could be the mechanism for the severe coldness experienced by young Japanese women suffering from unusual chilliness. They also reported that the cutaneous vascular conductance (CVC) in the forearm during cold exposure in the cold-sensitive group did not differ from those in the normal control group. It is unclear, however, whether the cutaneous vasoconstrictor sensitivity in the legs associated with severe chilliness during cold exposure is augmented in cold-sensitive women. Additionally, there is no information on the cutaneous vasoconstrictor response to local cooling in cold-sensitive women. This study was conducted to obtain a better understanding of the specific control of the skin blood flow (SkBF) in young women complaining of unusual chilliness. We hypothesized that the sensitivity of the reflex and local response for cutaneous vasoconstriction in the lower extremities is greater in young women complaining of unusual chilliness than in normal young women not suffering from it (protocols 1 and 2), and that augmented vasoconstrictor sensitivity is due to altered sympathetic postjunctional vasoconstrictor responses to NE (protocol 3).
Methods
Subjects
The experiments were approved by the Ethics Committee of Medical Care and Research of the University of Occupational and Environmental Health. All subjects were fully informed of the methods and risks before written informed consent was obtained. A total of 19 Japanese female subjects participated in the experiments. All subjects were healthy nonsmokers, non-obese (body mass index of 16–22 kg/m2), and not taking any medications. We selected young (18–22 years of age) women whose body weight and height were close to the averages for young Japanese women (48 kg and 158 cm, respectively) in order to rule out any possible effects of age and body composition on body temperature and thermal comfort. In addition, we chose the subjects based on a 10-question interview reported previously [13], which contains questions on typical complaints of those suffering from unusual chilliness. Subjects were those who answered yes more than six times in the interview [n = 10, cold-sensitive group (C)] and those who answered yes fewer than three times in the interview [n = 9, normal group (N)]. Those who answered yes three to six times were excluded from this study. Selected subjects were proved to be healthy by a medical examination and had regular menstrual cycles. Given that body temperature is fluctuated by the phases of the menstrual cycle, the experiments for protocols 1 and 3 were performed during the follicular phase, determined by the day of menstruation. A recent report showed, however, that the menstrual cycle had no effect on thermal perception and on autonomic cold-defense response in young female subjects [14]. In the experiments for protocol 2, the menstrual cycle was not considered because a previous report showed that the vasoconstrictor response to local cooling was unaffected by reproductive hormone status [15], differences in response between follicular and luteal phases were not seen in the present studies, and their data were combined for analysis. Their physical characteristics are shown in Table 1. All values were similar between the two groups.
Measurements
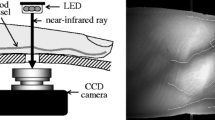
Body fat was measured using a body composition analyzer (EM-SCAN model HA-2; EM-SCAN, Springfield, IL, USA). Esophageal temperature (Tes) was measured with a polyethylene-sealed (1 mm diameter) thermocouple swallowed to the level of the heart in the esophagus. Skin temperatures (Tsk) at eight sites (forehead, chest, forearm, dorsal hand, thigh, calf, dorsal foot, and toe) were measured with copper–constantan thermocouples. The accuracy for all of the measurements was ±0.1 °C. Heart rate (HR) was determined using an electrocardiogram (ECG) with a telemetric device (BSM-2401; Nihon Kohden, Tokyo, Japan). SkBF on the left calf and left dorsal foot was measured by laser Doppler flowmetry (ALF21; Advance, Tokyo, Japan). Local temperature of the 6.3-cm2 area surrounding the site of SkBF measurement in the calf and dorsal foot was controlled using local temperature controllers combining a custom-built metal sleeve for the flow probe. A thermocouple between the skin surface and the sleeve served for measurement and feedback control. Local temperature could be easily maintained within 0.1 °C and could be rapidly changed with this controller. The measured variables for temperature and SkBF were recorded every 1 s using a data logger (DE1200 Universal; NEC Sanei, Tokyo, Japan).
Mean arterial pressure (MAP) was measured using a Dynamap automated oscillometric blood pressure device (model 8100; Criticon, Tampa, FL, USA). The measurement intervals of MAP were 10 min in protocol 1 and 5 min in protocols 2 and 3. Metabolic rate was assessed by indirect calorimetry to evaluate the heat production process; expiratory gas of a subject was collected through a face mask (Hans Rudolph; Shawnee, KS, USA); then, oxygen and carbon dioxide concentrations and flow rate of the expiratory gas were analyzed using a breath-by-breath gas-analyzing system consisting of a differential pressure transducer, sampling tube, filter, suction pump, and mass spectrometer (resolution, 0.001 %) (ARCO-2000; Arco System, Kashiwa, Japan). Metabolic rate was calculated using the values for nonprotein respiration quotient and oxygen consumption rate, and expressed as kilocalories per body surface area (m2) per hour.
During the whole-body cooling protocol, thermal comfort was evaluated every 10 min using a visual analogue scale, which is used for measuring feelings and sensations such as pain, thirst, thermal comfort [16–18]; the reliability and validity of this scale have been reported in prior studies [13, 19]. Subjects were asked to report thermal comfort for the body and lower extremities (feet and toes) separately by marking on a 15-cm line rating scale, which was labeled “cold” 2.5 cm from the left end and “not at all” 2.5 cm from the right end [13]. We instructed the subjects to mark on the scale how strongly they experienced cold discomfort due to the body cooling. In addition, the subjects were allowed to mark the level of comfort or discomfort beyond the cold or not-at-all points, if necessary. Then, the length from the point of not-at-all to the marked point was measured as the rating score of thermal discomfort, shown as a negative value.
Experimental protocols
The experiments consisted of three different protocols. For each protocol, the subjects arrived in the laboratory at 0900 hours after having abstained from caffeine and alcohol for at least 1 day and from food for at least 2 h. Dressed in sleeveless shirts and short pants, they entered the environmental chamber maintained at an ambient temperature (Ta) of 29.5 °C with relative humidity of 60 % and rested in a supine position on a bed. It has been verified that Ta of 29.5 °C is within the neutral range of thermal comfort in Japanese women, wearing similar clothes, who do or do not suffer from unusual chilliness [13]. All experiments were conducted in summer in Japan (from August to September) to avoid seasonal acclimation to a cold environment. In each experiment, female staff attached the electrodes of ECG and the thermocouples at chest sites.
Protocol 1. This protocol was conducted to examine the reflex component of cutaneous vasoconstriction in the lower extremities during whole-body cooling. All subjects participated and all variables described in the “Measurements” section were measured in this protocol. Subjects rested in a supine position for ~1 h while all measuring devices were applied. Subjects rested for another 20 min to obtain baseline data. Then, Ta was decreased from 29.5 to 23.5 °C at a rate of −0.1 °C/min and kept at this level for another 20 min. The temperature of 23.5 °C was not too cold to induce shivering or a sudden reduction in body temperature [13]. The Ta was automatically controlled using a personal computer (PC98BX; NEC, Tokyo, Japan). Local temperature at the sites of SkBF measurement was maintained at 35 °C throughout the experiments in this protocol.
Protocol 2. These experiments were conducted to examine the local component of SkBF control in the lower extremities. All subjects participated in this protocol. The subjects rested in a supine position for ~0.5 h while measuring devices were applied at Ta of 29.5 °C. SkBF in the calf and dorsal foot, Tes, blood pressure, HR, and Tsk at SkBF measuring sites were measured. Data collection began with a 5-min baseline control period at a local temperature of 35 °C at the two SkBF measurement sites. The sites were then cooled in −2.5 °C steps every 5 min to 25 °C over 20 min while Ta was maintained at 29.5 °C.
Protocol 3. This protocol was used to examine the adrenergic vasoconstrictor responsiveness in the lower extremities. Fourteen subjects (n = 7 for each group) recruited from the original groups participated in the experiment with this protocol. SkBF in the calf and dorsal foot, Tes, blood pressure, HR, and Tsk in SkBF measuring sites were measured. The subjects rested in a supine position for ~0.5 h while measuring devices were applied at Ta of 29.5 °C. The laser Doppler probe was installed at the center of an acrylate chamber, which permitted simultaneous blood flow measurement and iontophoresis to allow the introduction of NE into the skin by a weak electrical current (20 μA). The anode, made of platinum, was incorporated around the laser Doppler probe. The cathode was an ECG-electrode placed on the ankle. After 5-min baseline measurement, 10 mM NE (Sigma) dissolved in propylene glycol was applied to SkBF measuring sites by iontophoresis for 10 min [20, 21].
Data analysis
Measured variables were averaged over 1–10 min for data analysis in each protocol. Mean Tsk for 7 skin sites were calculated on the basis of the regional area (mean Tsk = 0.07 Tsk in forehead + 0.35 Tsk in chest + 0.14 Tsk in forearm + 0.05 Tsk in dorsal hand + 0.19 Tsk in thigh + 0.13 Tsk in calf + 0.07 Tsk in dorsal foot) [22]. Tsk in the lower extremities was expressed as the averaged values of Tsk in dorsal foot and toe (Tsk in the lower extremities = 0.5 Tsk in dorsal foot + 0.5 Tsk in toe). Cutaneous vascular conductance (CVC) was calculated as SkBF/MAP. Changes in CVC were expressed as percent changes from the averaged values during each baseline period for 20 min in protocol 1 and for 5 min in protocols 2 and 3. The differences in physical characteristics between the two groups were compared by Student’s t test. Differences in the measurement values between the C and N groups or the cooling and control periods were assessed by ANOVA with repeated measures. A significant difference of means between the two groups or periods at a specific time point was subsequently identified by the Newman–Keuls procedure. Regression analysis was conducted by the standard least-squares method. The significance of differences in slopes for the regression lines between the C and N groups was assessed by Student’s t test. All data are expressed as mean ± SE, and the null hypothesis was rejected at the level of P < 0.05. All statistical analyses were performed using the statistical and graphic software package KaleidaGraph 4.0 for Macintosh (Synergy Software, Reading, PA, USA).
Results
Protocol 1
Figure 1 shows the physiological responses during whole-body mild cold exposure in the C and N groups. There was no difference in baseline Tes between the two groups (C, 36.9 ± 0.1; N, 37.0 ± 0.1 °C) (Fig. 1a). Tes remained unchanged during the cold exposure in both groups. Baseline values for mean Tsk in the whole-body and lower extremities were similar between the C and N groups (Fig. 1b, c). Mean Tsk decreased with decreasing Ta without any differences between the two groups, while Tsk in the lower extremities in the C group (−5.7 ± 0.3 °C) tended (P = 0.09) to decrease more than in the N group (−5.0 ± 0.4 °C) during the cold exposure. There were no differences in the baseline values of metabolic rate, MAP, and HR between the two groups (Fig. 1d–f). The mild cold exposure tended to increase the metabolic rate in the N group only, resulting in a significantly lower metabolic rate in the C group for the last 20 min of cold exposure. In both groups, the mild cold exposure tended (P = 0.06) to increase MAP but did not change HR.
Changes in esophageal temperature (Tes; a), mean skin temperature (Tsk; b) from 7 sites, Tsk in the lower extremities (c), metabolic rate (d), mean arterial pressure (MAP; e), and heart rate (HR; f) during the control (29.5 °C) and cooling (29.5–23.5 °C) periods in the cold-sensitive (C; closed circles) and normal (N; open circles) groups. Values are mean ± SE. Asterisks significantly different between the C and N groups (P < 0.05). Daggers significantly different between the cooling and control periods within a group (P < 0.05)
The whole-body cold exposure decreased CVC in calf and dorsal foot with decreasing Tsk. As shown in Fig. 2, there were linear relationships between mean Tsk for the body and CVC in the cooling period. The slopes of the relationship between mean Tsk for the body and CVC in calf did not differ (P = 0.65) between the two groups (C, 19.5 ± 2.2; N, 18.1 ± 2.4 %/°C) (Fig. 2a), whereas those of the relationship between mean Tsk for the body and CVC in the dorsal foot were greater (P < 0.01) in the C group (20.5 ± 1.9 %/°C) than in the N group (12.5 ± 1.9 %/°C) (Fig. 2b).
Changes in cutaneous vascular conductance (CVC) in calf (a) and dorsal foot (b) in response to decreasing mean Tsk during the cooling period in the C (closed circles) and N (open circles) groups. The slope of the relationship between CVC in dorsal foot and mean Tsk in the C group was steeper than that in the N group (P < 0.05)
As depicted in Fig. 3, the rating scores of thermal comfort were linearly reduced with decreasing Tsk during the cold exposure. The slope of the regression line for Tsk and the rating score for the body were greater (P < 0.05) in the C group (37.4 ± 5.2 units/°C) than in the N group (19.8 ± 4.0 units/°C) (Fig. 3a), and those for Tsk and the rating score for the lower extremities were also greater (P < 0.01) in the C group (34.7 ± 4.7 units/°C) than in the N group (16.8 ± 3.9 units/°C) (Fig. 3b). The rating scores of thermal comfort for the body and the lower extremities at a given Tsk were smaller in the C group than in the N group.
Relationships between Tsk and thermal comfort for the body (a) and between Tsk and thermal comfort for the lower extremities (b) during the cooling period in the C (closed circle) and N (open circles) groups. A score of −100 indicates cold and a score of 0 indicates not cold at all. The slopes of the relationships between Tsk and thermal comfort in the C group were steeper than those in the N group (P < 0.05)
Protocol 2
Direct cooling of a small area in the lower extremities decreased the SkBF at the cooled sites without any changes in Tes, MAP, and HR. Figure 4 shows the changes in CVC in the calf and dorsal foot when the local temperature was decreased from 35 to 25 °C. Although there was no group difference in the CVC responses in calf (Fig. 4a), the local cooling-induced reduction in CVC in the dorsal foot was greater (P < 0.05) in the C group than in the N group (Fig. 4b).
Changes in CVC in calf (a) and dorsal foot (b) during decrease of local Tsk (35–25 °C) by direct skin cooling in the C (closed circles) and N (open circles) groups. Asterisks significantly different between the C and N groups (P < 0.05). Daggers significantly different between the cooling and control periods within a group (P < 0.05)
Protocol 3
Figure 5 shows the CVC responses to the application of exogenous NE at the sites of the calf and dorsal foot. In both sites, the exogenous NE significantly decreased CVC from that in the baseline control period. The NE-induced reduction of CVC in the calf did not differ between the two groups (Fig. 5a), whereas the reduction in the dorsal foot was greater (P < 0.01) in the C group than in the N group (Fig. 5b).
Changes in CVC during iontophoretic application of norepinephrine (NE) at the calf and the dorsal foot sites in the C (closed circles) and N (open circles) groups. Asterisks significantly different between the C and N groups (P < 0.05). Daggers significantly different between the NE iontophoresis and control periods within a group (P < 0.05)
Discussion
The novel findings from the current study are as follows. First, the sensitivity of cutaneous vasoconstrictor response in the dorsal foot to decreasing whole-body Tsk was greater in the C group than in the N group (protocol 1). Second, the cutaneous vasoconstrictor response in the dorsal foot to decreasing local Tsk was greater in the C group than in the N group (protocol 2). Third, the cutaneous vasoconstrictor response in the dorsal foot during NE iontophoresis was greater in the C group than in the N group (protocol 3). Finally, such augmented vasoconstrictor responsiveness in the C group was not observed in the calf for any of the experimental protocols.
It is generally recognized in Japan that individuals with a cold constitution suffer intense cold discomfort in the body, especially at the ends of the limbs, even under normal temperature conditions [5–10]. There are no definitive diagnostic criteria of a cold constitution, called “hi-e-sho” in Japanese, but about 50 % of Japanese women are conscious of it [5, 8–10]. In a preliminary study, we investigated the rate of the population suffering from unusual chilliness in daily life in 428 young female students using the questionnaire applied in this study. The investigation revealed that 44 (10.3 %) of the female students could be categorized into the C group (unpublished observations). In protocol 1, the cold discomfort of the body or the lower extremities at a given Tsk was greater in the C group than in the N group during mild cold exposure (Fig. 3). These results experimentally verify that the C group consisted of individuals with higher thermal sensitivity to cold. The greater thermal discomfort during cooling of the body did not derive from a lower core temperature because there was no significant difference in the levels in Tes between the two groups throughout the experiments in protocol 1 (Fig. 1a). The higher thermal sensitivity to cold in the C group would be due to: (1) a greater activity in somatosensory neurons in the cerebral cortex at a given peripheral thermosensitive input, (2) greater thermosensitive neural activity in the afferent pathway from skin to cerebral cortex, and/or (3) greater thermoreceptor excitation in the cutaneous endings of somatosensory neurons at a similar temperature. Since it has been reported that the number of cold and warm spots on the skin in the dorsal foot did not differ between the cold constitution group and the normal group [23], higher somatosensory neural activity within the central nervous system including cerebral cortex may be responsible for the higher thermal sensitivity to cold in the C group.
The vasoconstrictor response in human skin includes both reflex and local components during exposure to a cold environment [3, 24]. The roles of these components in SkBF control should be separately examined for the different underlying mechanisms [3, 24]. However, the characteristics of reflex and local vasomotor control in the populations with cold constitution are insufficiently known. In protocol 1, Ta was slowly decreased at 0.1 °C/min to 23.5 °C while local temperature around the SkBF measuring sites was maintained at 35 °C. During the whole-body mild cold exposure by reducing Ta from 29.5 to 23.5 °C, an unchanged plasma epinephrine concentration was previously observed [13]. Thus, it is thought that the cutaneous vasoconstriction observed in protocol 1 did not originate from a local-temperature-derived component and also occurred independently of activity of the adrenal gland. In protocol 1, there was no group difference in the changes in MAP and calf CVC during cold exposure, suggesting a similar centrally driven activity in skin sympathetic nerve in the C and N groups. We thus hypothesized that the regional difference of cutaneous vasoconstrictor reflex responses between the two groups might have been due to the process downstream of the sympathetic nerve. This hypothesis was tested in protocol 3. In humans, the cutaneous vasoconstrictor responsiveness to exogenous NE is greater in the legs than in the arms due to higher α1- and α2-adrenoceptor reactivity, while the β-adrenoceptor function plays a minor role in regional differences in adrenergic vasoconstriction [25]. From these findings, it is speculated that higher α1- and α2-adrenoceptor reactivity is responsible for the greater cutaneous vasoconstrictor response in the dorsal foot to the iontophoretic application of NE in the C group. Furthermore, higher adrenoceptor reactivity in the smooth muscle cells in skin vessels would contribute to the greater sensitivity in vasoconstrictor reflex response in the dorsal foot in the C group.
In protocol 2, when whole-body temperature was maintained at a thermoneutral level, the local skin cooling-induced vasoconstrictor response in the dorsal foot was greater in the C group (Fig. 4). It has been reported that Japanese women with the subjective symptom of chilliness showed slow recovery of finger temperature after immersion of the hand into slightly cool water (15 or 20 °C), when sympathetic nerve activity is minimally activated [8, 26]. These findings indicate that women with a cold constitution could show greater cutaneous vasoconstriction in the distal portions of the extremities regardless of reflex response. With respect to local components in SkBF control, both adrenergic mechanisms and functional nitric oxide synthase participate in the vasoconstrictor response during local skin cooling [3, 27, 28]. With adrenergic participation, the affinity of postsynaptic α2-adrenergic receptors for NE is enhanced by local cooling [29, 30]. Thus, we speculate that, in the C group, the greater cutaneous vasoconstriction at the distal sites in the lower extremities during local cooling was due to higher sensitivity in postsynaptic α2-adrenergic receptors and/or lower bioavailability of nitric oxide.
The metabolic rate in the N group tended to increase during exposure to a cool environment in protocol 1 (Fig. 1d). Cold-induced thermogenesis includes both shivering and non-shivering components. Since we did not observe visible shivering in any subjects throughout the experiments in this study, the increased metabolic rate in the N group might mainly have had a non-shivering origin. In a previous study [13], it was reported that serum thyroxine (T4) level was lower in the C group than in the N group, but without any significant differences in plasma epinephrine and cortisol levels. Okada et al. [31] reported a lower level of free triiodothyronine (T3) in women with a cold constitution. It is possible that a lower thyroid function in the C group was responsible for the lower metabolic rate during mild cold exposure. Recent studies demonstrated the existence of metabolically active brown adipose tissue (BAT) in adult humans, although the BAT activity after cold exposure shows inter-individual differences [32, 33]. A lower BAT activity in the C group is also postulated for the different metabolic responses during mild cold exposure, but further inverstigations are required into the role of BAT in cold constitution. In any case, it is thought that the greater vasoconstrictor sensitivity in the skin in individuals with cold constitution is an adaptive characteristic for preventing hypothermia caused by lower thermogenesis during exposure to a cold environment.
A methodological consideration is required in the present study. The techniques of laser Doppler flowmetry and iontophoresis enabled the continuous measurement of SkBF responses to vasoactive agents. Although iontophoresis provides a non-invasive technique to introduce charged substances across the surface of the skin, it is important to consider possible shortcomings of this technique [3]. For example, current alone may affect tissue perfusion. Therefore, the vasoconstrictor responses during iontophoretic applications of NE include effects of both drug and electrical current. It is thought, however, that the group differences in CVC responses in the dorsal foot during NE iontophoresis using the weak electrical current (20 μA) represented altered characteristics of the adrenergic vasoconstrictor response in the C group. In addition, the NE iontophoresis-induced reduction of CVC was within the range of reductions of CVC during whole-body and local cooling. It is surmised, therefore, that the amount of efficacious NE entry to the dermis was within the physiological ranges.
In conclusion, the findings from the current study suggest that young women with the complaint of chilliness show a greater cutaneous vasoconstrictor response to mild cold stress via altered adrenergic receptor sensitivity in the distal portion of the lower extremities.
References
Hensel H (1981) Thermoreception and temperature regulation. Academic, London
Nakamura K, Morrison SF (2008) Preoptic mechanism for cold-defensive responses to skin cooling. J Physiol 586:2611–2620
Johnson JM, Minson CT, Kellogg DL Jr (2014) Cutaneous vasodilator and vasoconstrictor mechanisms in temperature regulation. Compr Physiol 4:33–89
Stephens DP, Saad AR, Bennett LAT, Kosiba WA, Johnson JM (2004) Neuropeptide Y antagonism reduces reflex cutaneous vasoconstriction in humans. Am J Physiol Heart Circ Physiol 287:H1404–H1409
Miura T, Katano Y, Sumimoto K, Kanayama N (2001) Study on chilliness and lifestyle in young women. Jpn J Maternal Health 42:784–789
Sadakata M, Satoh E, Sayama M (2007) The skin surface temperature in the women with excessive sensitivity to cold (HIESHO) in the neutral-temperature environment. The study of the measurement-part helping to make the judging guideline and characteristic of the skin surface temperature. Biomed Thermol 27:1–7
Tanaka H, Shikimi T (2005) Thermal adjustment to mild-cold or mild-hot water immersion test in young women with cold constitution. Jpn Red Cross Med J 56:507–511
Yamada N, Bekku N, Yoshimura H (2007) Determinants for discriminating young woman with and without chilliness. Jpn J Neuropsychopharmacol 27:191–199
Yamada N, Yoshimura H (2009) Determinants of chilliness among young women and their application to psychopharmacological trials. Jpn J Neuropsychopharmacol 29:171–179
Yamato T, Aomine M (2002) Physical characteristics and living environment in female students with cold constitution. Health Eval Promot 29:878–884
Ikeda T, Suzuki Y, Maeda T (2013) Relationships between menstrual symptoms, lifestyle, habit, and cold sensitivity in high school students. Jpn J Maternal Health 53:487–496
Nakamura S (2010) “Sensitivity to cold”: a concept analysis. J Jpn Acad Nurs Sci 30:62–71
Nagashima K, Yoda T, Yagishita T, Taniguchi A, Hosono T, Kanosue K (2002) Thermal regulation and comfort during a mild-cold exposure in young Japanese women complaining of unusual coldness. J Appl Physiol 92:1029–1035
Matsuda-Nakamura M, Yasuhara S, Nagashima K (2015) Effect of menstrual cycle on thermal perception and autonomic thermoregulatory responses during mild cold exposure. J Physiol Sci. doi:10.1007/s12576-015-0371-x
Charkoudian N, Stephens DP, Pirkle KC, Kosiba WA, Johnson JM (1999) Influence of female reproductive hormones on local thermal control of skin blood flow. J Appl Physiol 87:1719–1723
Campbell WI, Lewis S (1990) Visual analogue measurement of pain. Ulster Med J 59:149–154
Frank SM, Raja SN, Bulcao CF, Goldstein DS (1999) Relative contribution of core and cutaneous temperatures to thermal comfort and autonomic responses in humans. J Appl Physiol 86:1588–1593
Wada F, Sagawa S, Miki K, Nagaya K, Nakamitsu S, Shiraki K, Greenleaf JE (1995) Mechanism of thirst attenuation during head-out water immersion in men. Am J Physiol 268:R583–R589
Aitken RC (1969) Measurement of feelings using visual analogue scales. Proc R Soc Med 62:989–993
Stephens DP, Aoki K, Kosiba WA, Johnson JM (2001) Nonnoradrenergic mechanism of reflex cutaneous vasoconstriction in men. Am J Physiol Heart Circ Physiol 280:H1496–H1504
Stephens DP, Bennett LAT, Ken Aoki K, Kosiba WA, Charkoudian N, Johnson JM (2002) Sympathetic nonnoradrenergic cutaneous vasoconstriction in women is associated with reproductive hormone status. Am J Physiol Heart Circ Physiol 282:H264–H272
Hardy JD, Du Bois EF (1938) The technic of measuring radiation and convection. J Nutr 15:461–475
Sadakata M, Yamada Y (2007) Perception of foot temperature in young women with cold constitution: analysis of skin temperature and warm and cold sensation thresholds. J Physiol Anthropol. 26:449–457
Alvarez GE, Zhao K, Kosiba WA, Johnson JM (2006) Relative roles of local and reflex components in cutaneous vasoconstriction during skin cooling in humans. J Appl Physiol 100:2083–2088
Yamazaki F, Yuge N (2011) Limb-specific differences in the skin vascular responsiveness to adrenergic agonists. J Appl Physiol 111:170–176
Kusumi Y, Emori Y (2009) Evaluation of hiesho using a cold-water load test in adults females. J Jpn Acad Midwif 23:241–250
Yamazaki F, Sone R, Zhao K, Alvarez GE, Kosiba WA, Johnson JM (2006) Rate dependency and role of nitric oxide in the vascular response to direct cooling in the human skin. J Appl Physiol 100:42–50
Hodges GJ, Zhao K, Kosiba WA, Johnson JM (2006) The involvement of nitric oxide in the cutaneous vasoconstrictor response to local cooling in humans. J Physiol 574:849–857
Ekenvall L, Lindblad LE, Norbeck O, Etzell BM (1988) α-adreneroceptors and cold-induced vasoconstriction in human finger skin. Am J Physiol 255:H1000–H1003
Flavahan NA, Lindblad L-E, Verbeuren TJ, Shepherd JT, Vanhoutte PM (1985) Cooling and α1- and α2-adrenergic responses in cutaneous veins: role of receptor reserve. Am J Physiol 249:H950–H955
Okada M, Uno M, Nagano E, Nomura Y, Ohira T, Sato S, Shimamoto T (2005) The relation of cold-water loading thermography with physical findings and lifestyle habit among women who have a cold constitution. Biomed Thermol 24:44–50
Nedergaard J, Bengtsson T, Cannon B (2007) Unexpected evidence for active brown adipose tissue in adult humans. Am J Physiol Endocrinol Metab 293:E444–E452
Yoneshiro T, Aita S, Matsushita M, Kameya T, Nakada K, Kawai Y, Saito M (2011) Brown adipose tissue, whole-body energy expenditure, and thermogenesis in healthy adult men. Obesity 19:13–16
Acknowledgments
The author thanks the subjects who participated in this experiment. I would also like to thank Mr. Yasuhiro Sogabe, Mr. Kouichi Monji and Ms. Nagisa Yuge for experimental assistance. This study was supported by Grant-in-Aid for Scientific Research (C) from the Japan Society for the Promotion of Science (24500688). The management of Grant-in-Aid for Scientific Research and the documents for this study was properly transferred from the University of Occupational and Environmental Health to the Yamaguchi Prefectural University for the movement of the author (Fumio Yamazaki).
Conflict of interest
The author declares that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Yamazaki, F. The cutaneous vasoconstrictor response in lower extremities during whole-body and local skin cooling in young women with a cold constitution. J Physiol Sci 65, 397–405 (2015). https://doi.org/10.1007/s12576-015-0378-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12576-015-0378-3