Abstract
Purpose
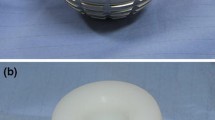
Patients with neurologic disorders are at a higher risk for hip arthroplasty dislocation. This can be attributed to hip muscle weakness, especially the abductor group. We inquired into the use of dual mobility acetabular component for the prevention of early hip dislocation in these patients.
Patients and methods
Thirty patients with documented neurological disorders and muscle weakness affecting the operated side underwent dual mobility total hip arthroplasty in the period between December 2012 and January 2014. The neurological disorders were cerebrovascular stroke, weakness due to brain tumors, Parkinsonism, old poliomyelitis, and multiple sclerosis. Twelve cases underwent primary dual mobility cup total hip arthroplasty as a treatment for proximal femoral fractures. Eighteen patients were revision to dual mobility total hip arthroplasty either due to failure of proximal femoral fracture fixation or failure of previous arthroplasty. All patients were ambulant (assisted walking) before the primary incident (either surgery or trauma). All patients were operated upon through the lateral approach. All the cups used were cemented.
Results
The mean age group of the patients was 64.6 years old. No definite postoperative infection occurred. The mean follow-up period was 13.2 months. One case died 6 months postoperative due to another cerebrovascular stroke. Functionally, all our patients could ambulate (assisted walking) postoperatively. No dislocation was recorded during the follow-up period.
Conclusion
The dual mobility cup is effective in the prevention of early dislocation in patients with muscle weakness due to neurological disorders. Long-term follow-up is needed for the assessment of late dislocation, as well as the rate of loosening in this group of patients.




Similar content being viewed by others
References
Mukka SS, Mahmood SS, Sayed-Noor AS (2013) Dual mobility cups for preventing early hip arthroplasty dislocation in patients at risk: experience in a county hospital. Orthop Rev 5(2):e10. doi:10.4081/or.2013.e10
Guyen O, GualterVaz VP, Chevillotte C, Béjui-Hugues J (2009) Use of a dual mobility socket to manage total hip arthroplasty instability. Clin Orthop Relat Res 467(2):465–472. doi:10.1007/s11999-008-0476-0
Kristiansen B, Jorgensen L, Holmich P (1985) Dislocation following total hip arthroplasty. Arch Orthop Trauma Surg 103:375–377
Dorr LD, Wolf AW, Chandler R, Conaty JP (1983) Classification and treatment of dislocations of total hip arthroplasty. Clin Orthop Relat Res 173:151–158
Soong M, Rubash HE, Macaulay W (2004) Dislocation after total hip arthroplasty. J Am Acad Orthop Surg 12:314–321
Bourne RB, Mehin R (2004) The dislocating hip: what to do, what to do. J Arthroplasty 19:111–114
Zhao F, Ma C, Xiong C (2007) Treatments of dislocation after total hip replacement. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 21:12–14
Woolson ST, Rahimtoola ZO (1999) Risk factors for dislocation during the first 3 months after primary total hip replacement. J Arthroplasty 14:662–668
Guyen O, Pibarot V, Vaz G, Chevillotte C, Carret JP, Bejui-Hugues J (2007) Unconstrained tripolar implants for primary total hip arthroplasty in patients at risk for dislocation. J Arthroplasty 22:849–858
Côté R, Battista RN, Wolfson C, Boucher J, Adam J, Hachinski V (1989) The Canadian neurological scale: validation and reliability assessment. Neurology 39(5):638–643
John J (1984) Grading of muscle power: comparison of MRC and analogue scales by physiotherapists. Medical Research Council. Int J Rehabil Res 7(2):173–181
Parker MJ, Maheshwer CB (1997) The use of a hip score in assessing the results of treatment of proximal femoral fractures. Int Orthod 21:262–264
Dorr L, Wan Z (1998) Causes of and treatment protocol for instability of total hip replacement. Clin Orthop Relat Res 335:144–151
Werner BC, Brown TE (2012) Instability after total hip arthroplasty. World J Orthop 3(8):122–130
Jämsen E, Puolakka T, Peltola M, Eskelinen A, Lehto MUK (2014) Surgical outcomes of primary hip and knee replacements in patients with Parkinson’s disease. A nationwide registry-based case-controlled study. Bone Joint J 96-B(4):486–49
Alberton G, High W, Morrey B (2002) Dislocation after revision total hip arthroplasty. J Bone Joint Surg Am 84-A(10):1788–1792
Williams JT, Ragland PS, Clarke S (2007) Constrained components for the unstable hip following total hip arthroplasty: a literature review. Int Orthop 31(3):273–277
Vielpeau C, Lebel B, Ardouin L, Burdin G, Lautridou C (2011) The dual mobility socket concept: experience with 668 cases. Int Orthop 35(2):225–230
Bouchet R, Mercier N, Saragaglia D (2011) Posterior approach and dislocation rate: a 213 total hip replacements case–control study comparing the dual mobility cup with a conventional 28-mm metal head/polyethylene prosthesis. Orthop Traumatol Surg Res 97(1):2–7
McKee GK, Watson-Farrar J (1966) Replacement of arthritic hips by the McKee-Farrar prosthesis. J Bone Joint Surg (Br) 48(2):245–259
Charnley J (1972) The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg (Br) 54(1):61–76
McArthur BA, Nam D, Cross MB, Westrich GH, Sculco TP (2013) Dual-mobility acetabular components in total hip arthroplasty. A review paper. Am J Orthop. 473-278
Boyer B, Philippot R, Geringer J, Farizon F (2012) Primary total hip arthroplasty with dual mobility socket to prevent dislocation: a 22-year follow-up of 240 hips. Int Orthop 36(3):511–518
Leiber-Wackenheim F, Brunschweiler B, Ehlinger M, Gabrion A, Mertl P (2011) Treatment of recurrent THR dislocation using of a cementless dual-mobility cup: a 59 cases series with a mean 8 years’ follow-up. Orthop Traumatol Surg Res 97(1):8–13
Philippot R, Adam P, Reckhaus M et al (2009) Prevention of dislocation in total hip revision surgery using a dual mobility design. Orthop Traumatol Surg Res 95(6):407–413
Guyen O, Pibarot V, Vaz G, Chevillotte C, Béjui-Hugues J (2009) Use of a dual mobility socket to manage total hip arthroplasty instability. Clin Orthop 467(2):465–472
Tarasevicius S, Busevicius M, Robertsson O, Wingstrand H (2010) Dual mobility cup reduces dislocation rate after arthroplasty for femoral neck fracture. BMC Musculoskelet Disord 11:175
Cross MB (2015) Dual mobility acetabular components for revision THA. J Orthop Traumatol 16(1):21–22
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Abdelazim, H., Michael, F. Dual mobility cup for prevention of early total hip arthroplasty dislocation in patients with neurological disorders. Eur Orthop Traumatol 6, 427–432 (2015). https://doi.org/10.1007/s12570-015-0336-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12570-015-0336-9