Abstract
Introduction
Neglected locked anterior shoulder dislocation is a rare condition as the injury is easily detectable. The humeral head is engaged against the anterior glenoid rim with a large Hill-Sachs defect. Due to the time lapse, there is additional soft tissue tightness. Our hypothesis is that Latarjet procedure combined with posterior capsular release will provide a stable shoulder with less limitation of external rotation in such cases.
Patients and methods
This prospective study was conducted on six shoulders. They were all addicted to tramadol and experienced fits which led to the dislocations. The mean age was 26.5 years. The mean presentation time was 9.16 weeks after injury. They all had locked anterior shoulder dislocation with mean Hill-Sachs lesion of 34 % of humeral head size. Open reduction through deltopectoral approach was done. The coracoid was osteotomized at the junction of the transverse and vertical part. The posterior capsule was released just after “unlocking” of the dislocation. After reduction, the coracoid was fixed to the freshened glenoid neck to increase the glenoid arc and avoid engaging of the humeral head defect. The subscapularis was re-attached in neutral rotation position.
Results
The mean follow up was 36.66 months. None of the cases had dislocation. The mean postoperative Constant score was 78.6, the postoperative Rowe score was 73.3, and external rotation in adduction was 46°.
Discussion
The results obtained support our hypothesis that, Latarjet procedure provides a stable and functional glenohumeral joint in cases of neglected anterior shoulder dislocation.
Similar content being viewed by others
Introduction
Locked anterior shoulder dislocation is a rare problem to face in orthopedic practice. Moreover, being missed, and subsequently encountered as neglected, is very rare as it is easily diagnosed [1]. Tramadol addicts tend to experience recurrent convulsive fits and subsequent shoulder violent dislocations [2, 3]. Patients usually are reluctant to seek specialized medical consultation. Some of them are presented with the problem of neglected locked anterior shoulder dislocation. The pathology is always a large bony “Hill-Sachs” defect together with soft tissue tightness due to the time lapse. Release of the tight posterior capsule and management of the head defect to avoid its further engagement against the glenoid rim is needed to avoid future recurrence [4]. We believe that with growing addiction to tramadol, this condition will be more frequently encountered. The use of bone allograft to reconstruct the head defect has been described as a management option with good outcome, but this option is not available in all counties [5]. Infraspinatus tenodesis (remplissage) provides a stable shoulder but with limitation of external rotation [4, 6]. Transhumeral headplasty has also been described but is difficult in neglected and large, Hill-Sachs defects; disimpaction may be most suited to acute lesions of less than 3 weeks old [7]. As these patients are usually young, shoulder arthroplasty is a remote surgical option. The high possibility for recurring fits makes relying solely on soft tissue procedures to stabilize the shoulder may be unreliable and subjected to failure [8]. Moreover, we need not only a stable joint, but a good function regarding range of motion and power. It is our hypothesis that an open reduction together with the release of the tight posterior capsule followed by a Latarjet procedure [9] to render the large engaging Hill-Sachs lesion non-engaging will end in a stable joint without marked limitation in the range of motion.
Materials and methods
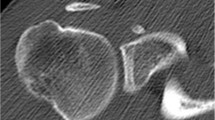
Between 2009 and 2011, this prospective study was conducted on six shoulders (five patients, one bilateral case) who presented with neglected locked anterior shoulder dislocation. They were all male patients addicted to tramadol of variable doses (800 mg up to 3 g per day) and experienced violent fits which led to dislocation. The age ranged between 22 and 31 years (mean 26.5 years). There were four right shoulders and two left shoulders. The mean presentation time was 9.16 weeks (4–13 weeks) after the injury as they did not seek prior specialized medical advice. The study was approved by the ethical committee at our institute, and all patients gave informed consent to participate in the study. X-rays, AP (anteroposterior) and true AP, were done for all the patients together with CT (computerized tomography) scan (Fig. 1). They all had locked anterior shoulder dislocation with mean Hill-Sachs lesion 34 % of humeral head size (Table 1). All patients were referred to toxicology department to start treatment of addiction.
Surgical technique
All our patients were operated in the beach-chair position under general anesthesia. After proper draping and antibiotic prophylaxis, a deltopectoral incision was made. The incision started 2 cm below the acromioclavicular joint as the coracoid cannot be easily palpated in these cases with locked dislocation. The incision extended for 15 cm distally aiming at the axillary fold. We approached the deltopectoral interval with 5 mm cuff of the deltoid fibers to protect the cephalic vein.
At this stage, we proceeded to coracoid osteotomy. This had two advantages. It helped with the exposure which was very tight at this stage and will be used for grafting at the end of the procedure. Proper exposure of the coracoids is done, together with the attachments of the conjoint tendon, coracoclavicular ligament, coracoacromial ligament, and pectoralis minor. The insertion of pectoralis minor was removed using electrocautery. A wafer of bone was removed from the medial coracoid edge using a saw with small blade to prepare this surface to face the glenoid neck. According to Burkhart and de Beer’s modification of Latarjet procedure “congruent-arc procedure,” this technique provides a greater extension of the glenoid arc [10]. Coracoacromial ligament was released from the coracoid process. Coracoid osteotomy was done just anterior to the attachment of the coracoclavicular ligaments to separate the horizontal from the vertical parts of the coracoid, taking as large piece of bone as possible without compromising the attachment of the coracoclavicular ligament. This was done with caution so that the saw blade would not injure the humeral head which is in a subcoracoid position. A small osteotome was used for the final “freeing” of the coracoid osteotomy. The coracoids fragment with the attached conjoint tendon was then carefully released to free it from the coracohumeral ligament using electrocautery till it was freely moving and could be used to pull on the conjoint tendon. The coracoids fragment was carefully held with an Allis forceps, and two drill holes were made from the prepared surface in a retrograde manner to ensure the central position of both holes with a good bone surrounding, these holes were made using 2.5 mm drill bit and 1 cm apart.
The bicipital groove was carefully palpated, and the subscapularis (together with the anterior shoulder capsule) was carefully released with the wafer of bone from the lesser tuberosity starting just medial to the medial edge of the bicipital groove. This technique allows a more secure fixation of the subscapularis at the end of the procedure which is essential in such cases. The subscapularis was held with heavy No. 2 Ethibond sutures (Ethicon; J&J), released, and allowed to slide medially, allowing full exposure of the humeral head. Gentle pull and manipulation were done till the humeral head was disengaged from the glenoid rim. Assessments of the head defect and cartilage condition were done, and then the humeral head was gently manipulated into the glenoid. At this stage, no instruments should be insinuated between the humeral head and glenoid to “lever” the heads back in place as this will lead to collapse of the usually soft humeral head cartilage at this stage. The head was usually reduced under pressure with the tendency to “jump” out of the glenoid once the manual pressure was released. This was the stage for posterior capsular release. With the head in external rotation, the release of the posterior glenohumeral capsule using electrocautery from 1 till 5 o’clock (in right shoulder) was done. This was done and repeated till we realize that the humeral head did not need that pressure to rest in place. Owing to the release of the subscapularis, any external rotation or extension will push the humeral head anteriorly out of the glenoid (but not jumping again medially as prior to the capsular release).
With the head reduced back in place, freshening of the distal half (3 to 6 o’clock on right shoulder) of the glenoid neck was done using curette. A drill hole was done in the freshened glenoid neck using the 2.5 mm drill bit 3 mm medial to the glenoid rim in the 5 o’clock position (a small blunt Hohmman retractor is placed in the axillary fold flush with the lower end of the glenoid for proper exposure). The direction of the drill bit was in line with the glenoid surface putting in mind its retroversion. The coracoid fragment was pulled back, and the 35 mm partial threaded screw (with its final threads standing out for easier entry into the drill hole) and then the fragment were fixed. The fragment was carefully controlled so that its upper part does not rotate outwards and stays flush with the glenoid rim. With the fragment fixed in place, the proximal screw was done with drilling the glenoid neck through the premade coracoid hole, followed by measuring the screw length followed by tapping and screw insertion. If the length of the measured (upper) screw was more than 5 mm from 35 mm inferior one, the distal screw was removed, checked for length. The subscapularis was pulled back and fixed in place using transossious Ethibond No. 2 sutures with the shoulder held in neutral rotation. Closure of the deltopectoral interval, subcutaneous tissue, and skin was done interruptedly. No drain was used. The arm was held in a simple arm sling with immobilizer to avoid external rotation.
Postoperative X-rays (AP and true AP) were done for all our patients together with CT scan. Plain X-rays were repeated after 3 and 6 months and at the last follow-up to detect any change of screws’ positions (Fig. 2).
We used a standard protocol postoperatively. An arm sling with immobilizer was used for 6 weeks, during which, pendulum exercises were started from the second postoperative day. Avoidance of shoulder extension and external rotation was stressed on. Strengthening exercises with gradual increase in the range of external rotation were started after 6 weeks. Postoperative clinical results were evaluated using Constant and Rowe scores [11, 12]. External rotation range was documented separately.
Results
The follow-up ranged between 24 and 45 months (mean 36.66). None of these cases had dislocation, infection, or neurological complications. One case had mild apprehension in external rotation. No case had change in screws’ position at last follow-up. Mean preoperative Constant score was 17 points (11–23). We did not do a preoperative Rowe score for these locked patients, believing that the score will not reflect the function of the shoulder as the stability due to locking is a functionless stability. Postoperative Constant and Rowe scores were calculated for all patients. The mean Constant score at the final follow-up was 78.6 points (Table 2), and the mean Rowe score was 73.3 points (Table 3). Mean external rotation in adduction was 46°.
Discussion
Tramadol addicts are in need of a long recovery protocol; during this period, they are subjected to recurrent fits [13]. These fits put a lot of stress over the reconstructed shoulder.
Engaged large head defects, posterior capsular tightness, and the high possibility of recurrent fits are the main problems that need to be solved to reach a stable joint with good functions. In the setting of humeral bone loss (Hill-Sachs) injury, treatment can be directed at the restoration of the glenohumeral articular arc with either glenoid-based solutions, humeral-based strategies, or both [14]. Burkhart advocates that if the Hill-Sachs injury is engaging, glenoid-based bone augmentation (e.g., Latarjet procedure) is sufficient for glenohumeral stability [10]. Reconstruction of the glenoid using the inferior surface of the coracoid graft to lengthen the glenoid articular arc and prevent the humeral defect from engaging the glenoid rim is a modification to the original surgery to utilize the length and the shape of the inferior coracoid surface to extend the articular arc of the glenoid and to provide good range of external rotation [10].
We calculated the mean external rotation in adduction to compare the results of the Latarjet procedure with the remplissage procedure which was performed previously on similar patients in a study by the first author (AM AbdelHady), in which postoperative limitation of external rotation was found (46 vs 27°) [4]. Apart from this study, little is written in the literature regarding locked anterior shoulder dislocation, and by comparing the current results with the prementioned paper, we found that Latarjet procedure yields superior function due to the better range of external rotation. Although some other studies revealed good range of external rotation after remplissage operation, all of these studies were made on cases with Hill-Sachs lesion without being in combination with neglected dislocation [15, 16].
Latarjet procedure is known to stand the test of time, and if no dislocation event occurs in the first 2 to 3 years, it is unlikely that it will happen later unlike soft tissue procedures (e.g., Bankart repairs) in which redislocation can happen up to 8 years following the operation [17, 18].
We believe that the limitation of our study was the low number of cases operated. As aforementioned, this is not a common problem, but we believe that it will be, unfortunately, increasing with the growing addiction to tramadol.
Conclusion
The results obtained support our hypothesis that Latarjet procedure provides a stable and functional glenohumeral joint in cases of neglected anterior shoulder dislocation.
References
Rowe CR, Zarins B, Ciullo JV (1984) Recurrent anterior dislocation of the shoulder after surgical repair. Apparent causes of failure and treatment. J Bone Joint Surg 66-A:159–168
Khan LH, Alderfer RJ, Graham DJ (1997) Seizures reported with tramadol. J Am Med Assoc 278:1661
Cicak N (2004) Posterior dislocation of the shoulder. J Bone Joint Surg 86-B:324–332
Abdelhady AM (2010) Neglected anterior shoulder dislocation: open remplissage of the Hill-Sachs lesion with the infraspinatus tendon. Acta Orthop Belg 76(2):162–165
Provencher MT, Frank RM, LeClere LE, Metzger PD, Ryu JJ, Bernhardson LA, Romeo A (2012) The Hill-Sachs lesion: diagnosis, classification, and management. J Am Acad Orthop Surg 20(4):242–252
Elkinson I, Giles J, Boons H, Faber K, Ferreira L, Johnson J, Athwa G (2013) The shoulder remplissage procedure for Hill-Sachs defects: does technique matter? J Shoulder Elbow Surg 22(6):835–841
Chen AL, Hunt SA, Zuckerman JD (2005) Humeral head impression fractures and head-splitting fractures. In: Zuckerman JD, Koval KJ (eds) Shoulder fractures: the practical guide to management. Thieme, New York, pp 120–145
Tauber M, Resch H, Forstner R, Raffl M, Josef SJ (2004) Reasons for failure after surgical repair of anterior shoulder instability. J Shoulder Elbow Surg 13(3):279–285
Latarjet M (1954) Treatment of recurrent dislocation of the shoulder. Lyon Chir 49:994–997
Burkhart SS, De Beer JF, Barth JR, Cresswell T, Roberts C, Richards DP (2007) Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. J Arthrosc 23(10):I033–I1041
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop 214:160
Rowe CR, Patel D, Southmayd WW (1978) The Bankart procedure: a long-term end-result study. J Bone Joint Surg 60A:1–16
Jovanović-Cupić V, Martinovic Z, Nesic N (2006) Seizures associated with intoxication and abuse of tramadol. Clin Toxicol (Phila) 44:143–146
Provencher MT; Rose M, Peace W (2012) Hill-Sachs injuries of the shoulder: when are these important and how should I manage them? In Provencher MT & Romeo AA eds, Shoulder instability: a comprehensive approach. 1st ed, Saunders. pp 235–251
Boileau P, O’Shea K, Vargas P, Pinedo M, Old J, Zumstein M (2012) Anatomical and functional results after arthroscopic Hill-Sachs remplissage. J Bone Joint Surg 94A:618–626
Zhu YM, Lu Y, Zhang J, Shen JW, Jiang CY (2011) Arthroscopic Bankart repair combined with remplissage technique for the treatment of anterior shoulder instability with engaging Hill-Sachs lesion: a report of 49 cases with a minimum 2-year follow-up. Am J Sports Med 39:1640–1647
Hovelius L, Sandström B, Saebö M (2006) One hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years. J Shoulder Elbow Surg 15:279–289
Lafosse L, Boyle S (2010) Arthroscopic Latarjet procedure. J Shoulder Elbow Surg 19:2–12
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abdelhady, A.M., AbouElsoud, M.M. Posterior capsular release and coracoid transfer for cases of neglected locked anterior shoulder dislocation in tramadol addicts. Eur Orthop Traumatol 6, 39–43 (2015). https://doi.org/10.1007/s12570-014-0279-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12570-014-0279-6