Abstract
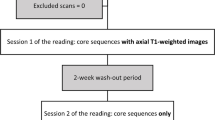
The aim of this study was to determine the vertebral level and variations in the position of the termination of both conus medullaris (CMT) and dural sac (DST) with special reference to the apex of the sacral hiatus (SHA) using magnetic resonance (MR) images and human cadavers. Different measurements were made on 200 MR sagittal T1- and T2-weighted lumbosacral images and 60 formalin-fixed adult human cadavers. The linear distances between the CMT, DST and SHA, the anteroposterior diameter at SHA, delete length and thickness of the sacrococcygeal membrane were also measured. These measurements were correlated with age and sex. In the MRI study, the mean vertebral level of CMT and its highest incidence were seen at the lower third of L1 (L1L) in male patients and at the L1-2 disc in female patients; that of DST was observed at the upper third of S2 (S2U) in male patients and the middle third of S2 (S2M) in female patients and the mean vertebral level of the SHA was noted at the middle third of S4 (S4M) in both males and females with no significant age or sex differences (P < 0.05). In the cadaveric specimens, the mean vertebral levels of CMT, DST and SHA were seen at L1L, S2M and S4U, respectively in both male and female specimens, with no sex difference. Also in the MRI study, all linear distances in the male patients were significantly different (P < 0.05) from those in female patients with exception of the thickness of SCM and the AP diameter at SHA. Accurate knowledge of these levels and the distances in-between are important for safe and successful spinal and caudal anaesthesia.




Similar content being viewed by others
Change history
02 January 2017
An erratum to this article has been published.
References
Aggarwal A, Kaur H, Batra YK, Aggarwal AK, Rajeev S, Sahni D (2009) Anatomic consideration of caudal epidural space: a cadaver study. Clin Anat 22:730–737
Cilliers A, Schulenburg DH, Janse van Rensburg J (2010) MRI determination of the vertebral termination of the dural sac tip in a South African population: clinical significance during spinal irradiation and caudal anaesthesia. SA J Radiol 14(3):52–55
Crighton IM, Barry BP, Hobbs GJ (1997) A study of the anatomy of the caudal space using magnetic resonance imaging. Br J Anaesth 78:391–395
Demiryürek D, Aydingöz Ü, Akşit MD, Yener N, Geyik PÖ (2002) MR imaging determination of the normal level of conus medullaris. Clin Imaging 26:375–377
Ievins FA (1991) Accuracy of placement of extradural needles in the L3/4 interspace: comparison of two methods of identifying L4. Br J Anaesth 66:381–382
Kim JT, Bahk JH, Sung J (2003) Influence of age and sex on the position of the conus medullaris and Tuffier’s line in adults. Anesthesiology 99:1359–1363
Lanier VS, McKnight HE, Trotter M (1944) Caudal analgesia: an experimental and anatomical study. Am J Obstet Gynecol 47:633–641
Lin N, Bebawy JF, Hua L, Wang BG (2010) Is spinal anaesthesia at L2–L3 interspace safe in disorders of the vertebral column? A magnetic resonance imaging study. Br J Anaesth 105(6):857–862
Lirk P, Messner H, Deibl M, Mitterschiffthaler G, Colvin J, Steger B et al (2004) Accuracy in estimating the correct intervertebral space level during lumbar, thoracic and cervical epidural anaesthesia. Acta Anaesthesiol Scand 48:347–349
Macdonald A, Chatrath P, Spector T, Ellis H (1999) Level of termination of the spinal cord and the dural sac: a magnetic resonance study. Clin Anat 12:149–152
Matveeva Niki, Chabukovska Radulova J, Strateska A, Bojadzieva B, Trpkovska B (2013) Anatomic landmarks for save spinal and epidural anesthesia. Acta morphol 10(1):10–14
Mc Cotter RE (1916) Regarding the length and extent of the human medulla spinalis. Anat Rec 10(559–564):1916
Moussallem CD, El Masri H, El-Yahchouchi C, Abou Fakher F, Ibrahim A (2014) Relationship of the lumbar lordosis angle to the level of termination of the conus medullaris and thecal sac. ARIJ, Article ID 351769, pp 4. 10.1155/2014/351769
Mustafa MS, Mahmoud OM, El Raouf HH, Atef HM (2012) Morphometric study of sacral hiatus in adult human Egyptian sacra: Their significance in caudal epidural anesthesia. Saudi J Anaesth 6(4):350–357
Nagar SK (2004) A study of sacral hiatus in dry human sacra. J Anat Soc India 53:18–21
Needles JH (1935) The caudal level of termination of the spinal cord in American whites and American Negroes. Anat Rec 63:417–424
Patil DS, Jadav Hrishikesh R, Binodkumar Mehta CD, Patel Vipul D (2012) Anatomical study of sacral hiatus for caudal epidural block. Nat J Med Res 2(3):272–275
Phongkitkarum S, Jaovisidha S, Dhanachai M (2004) Determination of the thecal sac ending using magnetic resonance imaging: clinical applications in craniospinal irradiation. J Med Assoc Thai 87:1368–1373
Rahmani M, Shabani Samghabadi MA, Vaziri Bozorg SM (2009) Magnetic resonance imaging based determination of conus medullaris position in adults. Res J Biol Sci 4(2):157–159
Reiman AF, Anson BJ (1944) Vertebral level of termination of the spinal cord with report of a case of a sacral cord. Anat Rec 88:127–138
Saifuddin A, Burnett SJD, White J (1998) The variation of position of the conus medullaris in an adult population. A magnetic resonance imaging study. Spine 23:1452–1456
Scharf CB, Paulino AC, Goldberg KN (1998) Determination of the inferior border of the thecal sac using magnetic resonance imaging: implications on radiation therapy treatment planning. Int J Radiat Oncol Biol Phys 41:621–624
Sekiguchi M, Yabuki S, Saton K, Kikuchi S (2004) An anatomical study of the sacral hiatus: a basis for successful caudal epidural block. Clin J Pain 20:51–54
Senoglu N, Senoglu M, Oksuz H, Gumusalan Y, Yukse KZ, Zencirci B et al (2005) Landmarks of the Sacral hiatus for caudal epidural block: an anatomical study. Br J Anaesth 95:692–695. doi:10.1093/bja/aei236
Soleiman J, Demaerel P, Rocher S, Maes F, Marchal G (2005) Magnetic resonance imaging study of the level of termination of the conus medullaris and the thecal sac: influence of age and gender. Spine 30(16):1875–1880
Standring S (2008) Gray’s anatomy, the anatomical basis of clinical practice, 40th edn. Churchill Livingstone Elsevier, London
Waldman SD (2004) Caudal epidural block: prone position. Atlas of interventional pain management, 2nd edn. Saunders, Philadelphia
Wilson DA, Prince JR (1989) MR imaging determination of the location of the normal conus medullaris throughout childhood. AJR Am J Neuroradiol 10:259–262. doi:0195-6108/89/1002-0259
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that he has no conflict of interest.
Additional information
An erratum to this article is available at https://doi.org/10.1007/s12565-016-0387-1.
Rights and permissions
About this article
Cite this article
Nasr, A.Y. Clinical relevance of conus medullaris and dural sac termination level with special reference to sacral hiatus apex: anatomical and MRI radiologic study. Anat Sci Int 92, 456–467 (2017). https://doi.org/10.1007/s12565-016-0343-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12565-016-0343-0