Abstract
Purpose
The purpose of this study was to examine the (a) prevalence of and (b) association between alcohol, risky sex, and HIV among Russians at risk for primary or secondary HIV transmission.
Method
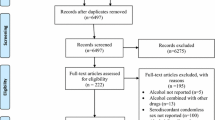
Electronic databases were searched to locate studies that sampled Russians, assessed alcohol use, and included either a behavioral measure of risk or a biological measure of HIV. Weighted mean (logit) effect sizes were calculated using random-effects assumptions. Moderator analyses were conducted using meta-regression.
Results
Studies (19) sampled 12,916 Russians (M age = 29; 36 % women). Participants were recruited from clinical (52 %; e.g., sexually transmitted infection (STI) clinic, drug treatment), other high-risk community settings (32 %; e.g., sexual/drug networks), or both (16 %). Findings indicate that a substantial proportion of the participants used alcohol (77 %; 55 % heavy drinking). One half of participants reported using condoms (52 %), but only 29 % used condoms consistently. Most participants reported drinking before sex (64 %). Of the studies testing for HIV, 10 % of participants tested positive. Meta-regression analyses indicated that hazardous/harmful alcohol use was associated with increased risky behaviors (i.e., multiple partners, inconsistent condom use).
Conclusion
These findings support the need for and potential benefit of addressing alcohol use in HIV prevention programming in Russia.


Similar content being viewed by others
Notes
Because the prevalence of alcohol use, sexual risk behaviors, and HIV/STIs may have changed over time, we examined publication date as a possible predictor of the observed prevalence estimates. Publication date was not a predictor of alcohol use, sexual risk behaviors, or HIV/STIs, ps ≥ .06.
References
UNAIDS. The Gap Report. 2014.
Piot P, Abdool Karim SS, Hecht R, et al. Defeating AIDS—advancing global health. Lancet. 2015;386(9989):171–218. doi:10.1016/s0140-6736(15)60658-4.
Pokrovsky V, Ladnaya NN, Buravtsova EV. HIV Infection: information bulletin #34. Russian Federal AIDS Center. 2010.
Centers for Disease Control and Prevention. Rapid increase in HIV rates—Orel Oblast, Russian Federation, 1999-2001. Morb Mortal Wkly Rep. 2003;52(28):657–60.
Rakhmanova A, Vinogradova E, Yakovev A. The characteristics of HIV-infection in St. Petersburg. St. Petersburg, Russian Federation 2007.
Balachova TN, Batluk JV, Bryant KJ, Shaboltas AV. International collaboration in HIV prevention research: evidence from a research seminar in Russia. AIDS Res Hum Retrovir. 2015;31(2):163–72. doi:10.1089/aid.2014.0078.
World Health Organization. Global Status Report on Alcohol and Health. 2014.
Chenet L, McKee M, Leon D, Shkolnikov V, Vassin S. Alcohol and cardiovascular mortality in Moscow; new evidence of a causal association. J Epidemiol Community Health. 1998;52(12):772–4.
Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373(9682):2223–33. doi:10.1016/s0140-6736(09)60746-7.
World Health Organization. WHO country profile: the Russian Federation. 2011. http://www.who.int/substance_abuse/publications/global_alcohol_report/profiles/rus.pdf. Accessed June 22, 2014.
Fortenberry JD, Orr DP, Katz BP, Brizendine EJ, Blythe MJ. Sex under the influence. A diary self-report study of substance use and sexual behavior among adolescent women. Sex Transm Dis. 1997;24(6):313–9.
Irwin TW, Morgenstern J, Parsons JT, Wainberg M, Labouvie E. Alcohol and sexual HIV risk behavior among problem drinking men who have sex with men: an event level analysis of timeline followback data. AIDS Behav. 2006;10(3):299–307. doi:10.1007/s10461-005-9045-7.
Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S. Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: systematic review of empirical findings. Prev Sci. 2007;8(2):141–51. doi:10.1007/s11121-006-0061-2.
Morojele NK, Kachieng’a MA, Mokoko E, et al. Alcohol use and sexual behaviour among risky drinkers and bar and shebeen patrons in Gauteng province. South Africa Social Science & Medicine. 2006;62(1):217–27. doi:10.1016/j.socscimed.2005.05.031.
Scott-Sheldon LAJ, Walstrom P, Carey KB, Johnson BT, Carey MP. Alcohol use and sexual risk behaviors among individuals infected with HIV: a systematic review and meta-analysis 2012 to early 2013. Current HIV/AIDS reports. 2013;10(4):314–23. doi:10.1007/s11904-013-0177-5.
Bryant KJ. Expanding research on the role of alcohol consumption and related risks in the prevention and treatment of HIV/AIDS. Subst Use Misuse. 2006;41(10–12):1465–507. doi:10.1080/10826080600846250.
Shuper PA, Neuman M, Kanteres F, Baliunas D, Joharchi N, Rehm J. Causal considerations on alcohol and HIV/AIDS—a systematic review. Alcohol & Alcoholism. 2010;45(2):159–66. doi:10.1093/alcalc/agp091.
Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect. 1999;75(1):3–17.
Cook RL, Clark DBI. There an association between alcohol consumption and sexually transmitted diseases? A systematic review. Sex Transm Dis. 2005;32(3):156–64.
Baliunas D, Rehm J, Irving H, Shuper P. Alcohol consumption and risk of incident human immunodeficiency virus infection: a meta-analysis. International journal of public health. 2010;55(3):159–66. doi:10.1007/s00038-009-0095-x.
Baum MK, Rafie C, Lai S, Sales S, Page JB, Campa A. Alcohol use accelerates HIV disease progression. AIDS Res Hum Retrovir. 2010;26(5):511–8. doi:10.1089/aid.2009.0211.
World Health Organization. Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations. 2014. http://apps.who.int/iris/bitstream/10665/128048/1/9789241507431_eng.pdf?ua = 1&ua = 1.
Wilsnack RW, Wilsnack SC, Kristjanson AF, Vogeltanz-Holm ND, Gmel G. Gender and alcohol consumption: patterns from the multinational GENACIS project. Addiction. 2009;104(9):1487–500. doi:10.1111/j.1360-0443.2009.02696.x.
Beyrer C, Baral SD, Walker D, Wirtz AL, Johns B, Sifakis F. The expanding epidemics of HIV type 1 among men who have sex with men in low- and middle-income countries: diversity and consistency. Epidemiol Rev. 2010;32:137–51. doi:10.1093/epirev/mxq011.
Shannon K, Strathdee SA, Goldenberg SM, et al. Global epidemiology of HIV among female sex workers: influence of structural determinants. Lancet. 2015. doi:10.1016/s0140-6736(14)60931-4.
UNAIDS. 2015 Epidemiological slides—How AIDS Changed Everything report. 2015.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41. doi:10.1016/j.ijsu.2010.02.007.
Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12.
Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–84.
Fowkes FG, Fulton PM. Critical appraisal of published research: introductory guidelines. BMJ (Clinical research ed). 1991;302(6785):1136–40.
Baral S, Kizub D, Masenior NF, et al. Male sex workers in Moscow, Russia: a pilot study of demographics, substance use patterns, and prevalence of HIV-1 and sexually transmitted infections. AIDS Care. 2010;22(1):112–8. doi:10.1080/09540120903012585.
Abdala N, Zhan WH, Shaboltas AV, Skochilov RV, Kozlov AP, Krasnoselskikh TV. Efficacy of a brief HIV prevention counseling intervention among STI clinic patients in Russia: a randomized controlled trial. AIDS Behav. 2013;17(3):1016–24. doi:10.1007/s10461-012-0311-1.
Hoffman IF, Latkin CA, Kukhareva PV, et al. A peer-educator network HIV prevention intervention among injection drug users: results of a randomized controlled trial in St. Petersburg, Russia. AIDS Behav. 2013;17(7):2510–20. doi:10.1007/s10461-013-0563-4.
Samet JH, Krupitsky EM, Cheng DM, et al. Mitigating risky sexual behaviors among Russian narcology hospital patients: the PREVENT (Partnership to Reduce the Epidemic Via Engagement in Narcology Treatment) randomized controlled trial. Addiction. 2008;103(9):1474–83.
Samet JH, Raj A, Cheng DM, et al. HERMITAGE-a randomized controlled trial to reduce sexually transmitted infections and HIV risk behaviors among HIV-infected Russian drinkers. Addiction. 2015;110(1):80–90. doi:10.1111/add.12716.
Lipsey MW, Wilson DB. Practical meta-analysis. Thousand Oaks, CA: Sage.
Stata Corp. Stata Statistical Software: Release 12. College Station, TX: Stata Corp 2011.
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
World Health Organization. AUDIT: The Alcohol Use Disorders Identification Test, guidelines for use in primary care.. 2nd ed. Geneva, Switzerland: World Health Organization,; 2001.
Wirtz AL, Zelaya CE, Latkin C, et al. Alcohol use and associated sexual and substance use behaviors among men who have sex with men in Moscow, Russia. AIDS Behav. 2015:1–14. doi:10.1007/s10461-015-1066-2.
Cook RL, Comer DM, Wiesenfeld HC, et al. Alcohol and drug use and related disorders: an underrecognized health issue among adolescents and young adults attending sexually transmitted disease clinics. Sex Transm Dis. 2006;33(9):565–70. doi:10.1097/01.olq.0000206422.40319.54.
Howards PP, Thomas JC, Earp JA. Do clinic-based STD data reflect community patterns? Int J STD AIDS. 2002;13(11):775–80. doi:10.1258/095646202320753745.
Schroder KE, Carey MP, Vanable PA. Methodological challenges in research on sexual risk behavior: II. Accuracy of self-reports. Ann Behav Med. 2003;26(2):104–23.
Niccolai LM, Shcherbakova IS, Toussova OV, Kozlov AP, Heimer R. The potential for bridging of HIV transmission in the Russian Federation: sex risk behaviors and HIV prevalence among drug users (DUs) and their non-DU sex partners. Journal of Urban Health. 2009;86(Suppl 1):131–43. doi:10.1007/s11524-009-9369-0.
Higgins JPT. Commentary: heterogeneity in meta-analysis should be expected and appropriately quantified. Int J Epidemiol. 2008;37(5):1158–60. doi:10.1093/ije/dyn204.
Higgins JPT, Thompson SG, Spiegelhalter DJA. Re-evaluation of random-effects meta-analysis. Journal of the Royal Statistical Society: Series A (Statistics in Society). 2009;172(1):137–59. doi:10.1111/j.1467-985X.2008.00552.x.
IOGT International. HIV and Alcohol. Sweeden. 2009. http://ec.europa.eu/health/alcohol/docs/alcohol_lib23_en.pdf. Accessed March 10 2016.
Amirkhanian YA, Kelly JA, Takacs J, et al. HIV/STD prevalence, risk behavior, and substance use patterns and predictors in Russian and Hungarian sociocentric social networks of men who have sex with men. AIDS Educ Prev. 2009;21(3):266–79.
Eritsyan KU, Levina OS, White E, Smolskaya TT, Heimer R. HIV prevalence and risk behavior among injection drug users and their sex partners in two Russian cities. AIDS Res Hum Retrovir. 2013;29(4):687–90. doi:10.1089/aid.2012.0161.
Fleming MF, Krupitsky EM, Tsoy M, et al. Alcohol and drug use disorders, HIV status and drug resistance in a sample of Russian TB patients. International Journal of Tuberculosis and Lung Disease. 2006;10(5):565–70.
Iguchi MY, Ober AJ, Berry SH, et al. Simultaneous recruitment of drug users and men who have sex with men in the United States and Russia using respondent-driven sampling: sampling methods and implications. Journal of Urban Health. 2009;86(Suppl 1):5–31. doi:10.1007/s11524-009-9365-4.
Krupitsky EM, Zvartau E, Karandashova G, et al. The onset of HIV infection in the Leningrad region of Russia: a focus on drug and alcohol dependence. HIV medicine. 2004;5(1):30–3.
Krupitsky EM, Horton NJ, Williams EC, et al. Alcohol use and HIV risk behaviors among HIV-infected hospitalized patients in St. Petersburg, Russia. Drug Alcohol Depend. 2005;79(2):251–6. doi:10.1016/j.drugalcdep.2005.01.015.
Niccolai LM, Odinokova VA, Safiullina LZ, et al. Clients of street-based female sex workers and potential bridging of HIV/STI in Russia: results of a pilot study. AIDS Care. 2012;24(5):665–72. doi:10.1080/09540121.2011.630356.
Odinokova V, Rusakova M, Urada LA, Silverman JG, Raj A. Police sexual coercion and its association with risky sex work and substance use behaviors among female sex workers in St. Petersburg and Orenburg, Russia. International Journal of Drug Policy. 2014;25(1):96–104. doi:10.1016/j.drugpo.2013.06.008.
Shipitsyna E, Krasnoselskikh T, Zolotoverkhaya E, et al. Sexual behaviours, knowledge and attitudes regarding safe sex, and prevalence of non-viral sexually transmitted infections among attendees of youth clinics in St. Petersburg, Russia. Journal of the European Academy of Dermatology and Venereology : JEADV. 2013;27(1):e75–84. doi:10.1111/j.1468-3083.2012.04512.x.
Vasquez C, Lioznov D, Nikolaenko S, et al. Gender disparities in HIV risk behavior and access to health care in St. Petersburg, Russia. AIDS Patient Care STDs. 2013;27(5):304–10. doi:10.1089/apc.2013.0019.
Zhan WH, Krasnoselskikh TV, Niccolai LM, Golovanov S, Kozlov AP, Abdala N. Concurrent sexual partnerships and sexually transmitted diseases in Russia. Sex Transm Dis. 2011;38(6):543–7. doi:10.1097/OLQ.0b013e318205e449.
Zhan WH, Shaboltas AV, Skochilov RV, Kozlov AP, Krasnoselskikh TV, Abdala N. Alcohol misuse, drinking contexts and intimate partner violence in St. Petersburg, Russia: results from a cross-sectional study. BMC Public Health. 2011;11:629. doi:10.1186/1471-2458-11-629.
Zhan WH, Shaboltas AV, Skochilov RV, Krasnoselskikh TV, Abdala N. History of childhood abuse, sensation seeking, and intimate partner violence under/not under the influence of a substance: a cross-sectional study in Russia. PLoS One. 2013;8(7):e68027. doi:10.1371/journal.pone.0068027.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Funding
Research reported in this paper was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health under award number R01 AA021355 to Lori A. J. Scott-Sheldon, PhD. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Rights and permissions
About this article
Cite this article
Lan, CW., Scott-Sheldon, L.A.J., Carey, K.B. et al. Prevalence of Alcohol Use, Sexual Risk Behavior, and HIV Among Russians in High-Risk Settings: a Systematic Review and Meta-Analysis. Int.J. Behav. Med. 24, 180–190 (2017). https://doi.org/10.1007/s12529-016-9596-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-016-9596-1