Abstract
Background
Medically unexplained (somatoform) symptoms (MUS) are highly prevalent in primary care. It remains unclear to what extent patients and their general practitioners (GPs) agree upon the etiology of physical symptoms as well as on the number of visits to the GP.
Purpose
The purpose of this study is to determine patient–physician agreement on reported symptoms.
Method
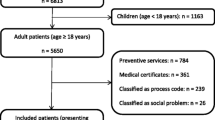
A sample of 103 persons provided information on MUS and health care utilization (HCU) during the previous 12 months. The persons' GPs (n = 103) were asked for the same information. By determining patient–physician agreement on reported symptoms, the sample was subdivided into a concordance group (high agreement: Pt = GP) and two discordance groups (substantial disagreement: Pt > GP, Pt < GP).
Results
Patients and their GPs showed substantial disagreement concerning physical symptom reports for the prior 12 months. On means, patients named 3.26 (SD = 3.23; range 0–21) physical complaints of which 71.6% were considered to be medically unexplained (MUS), whereas GPs only determined 1.77 (SD = 1.94; range 0–11) symptoms of which 57.5% were MUS. Substantial patient–physician agreement regarding the number of reported MUS was detected in 29.1% of the cases (Pt = GP). Patients of all groups underestimated their HCU.
Conclusion
Since patients' and GPs' reports differ substantially concerning the etiology of symptoms and concerning HCU, both sources of data gathering should be treated carefully in primary care research.

Similar content being viewed by others
Abbreviations
- MUS:
-
Medically unexplained symptoms
- MES:
-
Medically explained symptoms
- GP:
-
General practitioner
- HCU:
-
Health care utilization
- Pt:
-
Patient
References
Fink P, Sorensen L, Engberg M, Holm M, Munk-Jorgensen P. Somatization in primary care: prevalence, health care utilization and general practitioner recognition. Psychosomatics. 1999;40:330–8.
Hiller W, Rief W, Brähler E. Somatization in the population: from mild bodily misperceptions to disabling symptoms. Soc Psychiatry Psychiatr Epidemiol. 2006;41:704–12.
Rief W, Hessel A, Brähler E. Somatization symptoms and hypochondriacal features in the general population. Psychosom Med. 2001;63:595–602.
Katon WJ, Walker EA. Medically unexplained symptoms in primary care. J Clin Psychiatry. 1998;59:15–21.
Khan AA, Khan A, Harezlak J, Tu W, Kroenke K. Somatic symptoms in primary care: etiology and outcome. Psychosomatics. 2003;44:471–8.
Kroenke K, Mangelsdorff D. Common symptoms in ambulatory care: incidence, evaluation, therapy and outcome. Am J Med. 1989;86:262–6.
Al-Windi A. The influence of complaint symptoms on health care utilisation, medicine use and sickness absence. A comparison between retrospective and prospective utilisation. J Psychosom Res. 2005;59:139–46.
Barsky AJ, Orav EJ, Bates DW. Somatization increases medical utilization and costs independent of psychiatric and medical comorbidity. Arch Gen Psychiatry. 2005;62:903–10.
Mewes R, Rief W, Brähler E, Martin A, Glaesmer H. Lower decision threshold for doctor visits as a predictor of health care use in somatoform disorders and in the general population. Gen Hosp Psychiatry. 2008;30:349–55.
Deyo RA. Cascade effects of medical technology. Annu Rev Public Health. 2002;23:23–44.
Heywood PL, Blackie GC, Cameron IH, Dowell AC. An assessment of the attributes of frequent attenders to general practice. Fam Pract. 1998;15:198–204.
Jyväsjärvi S, Joukamaa M, Väisanen E, Larivaraa P, Kivelä S-L, Keinänen-Kiukaanniemi S. Somatizing frequent attenders in primary health care. J Psychosom Res. 2001;50:185–92.
Portegijs P, van der Horst FG, Proot IM, Kraan HF, Gunther NC, Knottnerus JA. Somatization in frequent attenders of general practice. Soc Psychiatry Psychiatr Epidemiol. 1996;31:29–37.
Jackson J. Communication about symptoms in primary care: impact on patient outcomes. J Altern Complement Med. 2005;11:51–6.
Boland BJ, Scheitek SM, Wollan PC, Silverstein MD. Patient–physician agreement on reasons for ambulatory general medical examinations. Mayo Clin Proc. 1998;73:109–17.
Scheuer E, Steurer J, Buddeberg C. Predictors of differences in symptom perception in older patients and their doctors. Fam Pract. 2002;19:357–61.
Greer J, Halgin R. Predictors of physician–patient-agreement on symptom etiology in primary care. Psychosom Med. 2006;68:277–82.
Helman CG. Communication in primary care: the role of patient and practitioner explanatory models. Soc Sci Med. 1985;20:923–31.
Peveler R, Kilkenny L, Kinmonth A-L. Medically unexplained physical symptoms in primary care: a comparison of self-report screening questionnaires and clinical opinion. J Psychosom Res. 1997;42:245–52.
Rief W, Mewes R, Martin A, Glaesmer H, Brähler E. Are psychological features useful in classifying patients with somatic symptoms? Psychosom Med. 2010;72:648–55.
World Health Organization (WHO). Composite International Diagnostic Interview (CIDI 3.0, Version 7). WHO; 2007.
Andrews G, Peters L. The psychometric properties of the Composite International Diagnostic Interview. Soc Psychiatry Psychiatr Epidemiol. 1998;33:80–8.
Steinbrecher N, Koerber S, Frieser D, Hiller W. The prevalence of medically unexplained symptoms in primary care. Psychosomatics. 2011;52:263–71.
Hiller W, Cebulla M, Korn H-J, Leibbrand R, Röers B, Nilges P. Causal symptom attribution in somatoform disorder and chronic pain. J Psychosom Res. 2010;68:9–19.
Frostholm L, Ornbol E, Schou Hansen H, Olesen F, Weinman J, Fink P. Which is more important for outcome: the physician's or the patient's understanding of a health problem? A 2-year follow-up study in primary care. Gen Hosp Psychiatry. 2010;32:1–8.
Rief W, Nanke A, Emmerich J, Bender A, Zech T. Causal illness attributions in somatoform disorders. Associations with comorbidity and illness behaviour. J Psychosom Res. 2004;57:367–71.
Ring A, Dowrick CF, Humphris GM, Davies J, Salmon P. The somatising effect of clinical consultation: what patients and doctors say and do not say when patients present medically unexplained physical symptoms. Soc Sci Med. 2005;61:1505–15.
Acknowledgements and Funding
This study was supported by a grant from the German Research Foundation to Prof. Rief, Brähler & Martin (grant RI 574/14-1).
The study protocol was approved by the ethics committee of the German Research Foundation.
Competing interests
The authors declare that they have no competing interests.
Authors' Contributions
All listed authors have contributed to this study. SS participated in data acquisition, performed the statistical analysis, and drafted the manuscript. WR, EB, and AM conceived the study and revised the manuscript critically for important intellectual content. WR participated in interpretation of data and helped to draft the manuscript. HG participated in the design of the study and data acquisition. RM participated in the design of the study and coordination, helped interpreting the data, and to draft the manuscript. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schumacher, S., Rief, W., Brähler, E. et al. Disagreement in Doctor's and Patient's Rating About Medically Unexplained Symptoms and Health Care Use. Int.J. Behav. Med. 20, 30–37 (2013). https://doi.org/10.1007/s12529-011-9213-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-011-9213-2