Abstract
Background
Obesity is a major risk factor for cardiovascular disease (CVD), with weight loss offering improvement in CVD risk factors.
Aims
To examine whether weight loss in laparoscopic adjustable gastric band (LAGB)-treated obese patients is associated with meaningful reductions in estimated 10- and 30- year Framingham CVD risk 12–15 months post-LAGB.
Methods
Obese adult patients [body mass index (BMI) ≥30 kg/m2] treated with LAGB were identified in a large US healthcare database. Patients without CVD at baseline and with measures of BMI, systolic blood pressure, diabetes, and smoking status at baseline and follow-up were eligible. Non-LAGB patients were propensity score matched to LAGB patients on baseline BMI, age, and gender. Estimated 10- and 30-year risk of developing CVD using office-based data, including BMI, was calculated at baseline and 12–15 months follow-up.
Results
Mean BMI in LAGB patients (n = 647, average age 45.66 years, 81.1% female) decreased from 42.7 to 33.4 kg/m2 (P < 0.0001), with 35.4% no longer obese; 10- and 30-year estimated CVD risk decreased from 10.8 to 7.6% (P < 0.0001) and 44.34 to 32.30% (P < 0.0001), respectively, 12–15 months post-LAGB. Improvements were significantly greater than in non-LAGB patients (N = 4,295) (P < 0.0001). In the subset with lipid data (n = 74), improvements in total (−20.6 mg/dL; P < 0.05) and high-density lipoprotein (+10.6 mg/dL, P < 0.0001) cholesterol 1 year post-LAGB were also observed.
Conclusions
Data from a US healthcare database show that individuals undergoing LAGB have significant weight loss and reductions in estimated 10- to 30-year CVD risk within 1 year post-LAGB.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is the leading cause of death in the US, accounting for over one-third of all deaths in 2007 [1]. By the year 2030, it is projected that over 40% of the US population will have some form of CVD [2]. Obesity, reported to affect 34% of the US adult population [3], is a major risk factor for CVD that may exacerbate other known CVD risk factors, such as hypertension, dyslipidemia, and diabetes [1, 4]. Weight loss improves these risk factors [5–8] with the degree of improvement often commensurate with the degree of weight loss [5, 9]. Bariatric surgery complemented by lifestyle modification is associated with gradual and sustained weight loss and has become a viable weight management approach in select patients [7, 10–12], with some guidelines including laparoscopic adjustable gastric banding (LAGB) for individuals with body mass index (BMI) ≥30 and 1 or more comorbidities of obesity [10]. Although surgery-facilitated weight loss typically improves CVD risk factors [7, 13], the long-term clinical impact of the weight loss on CVD risk factors and on outcomes after bariatric surgery is not well described.
Cardiovascular disease risk algorithms, including those developed within the Framingham Heart Study (FHS) [14–16], may inform predicted clinical impact of obesity and weight loss. Framingham Risk Scores (FRS) for 10-year coronary heart disease (CHD) are greater with BMI [17] and several studies have documented substantial reductions in 10-year CHD risk 1 year after bariatric surgery [18–22]; however, these studies have not included LAGB. Notably, significant reductions in FRS have not been observed following pharmacologic or lifestyle weight loss interventions [23].
The authors examined whether weight loss in LAGB‐treated obese patients would be associated with meaningful reductions in 10‐ and 30-year Framingham CVD risk scores 12–15 months post‐LAGB in a large observational US healthcare database.
Methods
The analysis in this article is based on previously collected data and does not involve any new studies of human or animal subjects performed by any of the authors. This study utilized data from a national network of outpatient offices, the Medical Quality Improvement Consortium (MQIC), using the GE Centricity electronic medical records system. The MQIC database contains de-identified patient clinical information from a nationally representative patient population in the US. Patients in the MQIC database with LAGB procedure were selected based on the following: LAGB procedure between January 1 2005 and April 30 2010 (baseline); BMI ≥30 kg/m2 at baseline, aged 30–73 years, with 12–15 months of data available after baseline. Patients with CVD diagnoses before baseline were excluded. Baseline measures were taken at the closest visit prior to, but not more than 90 days before, LAGB procedure. Matched non-LAGB patients were selected for each LAGB patient based on the following: no history of weight reduction surgery; index date between January 1 2005 and April 30, 2010 (baseline); BMI ≥ 30 kg/m2 at baseline; aged 30–73 years; and with 12–15 months of data available after baseline. Both groups of patients were required to have two BMI measures 12–15 months apart, and their baseline date was the first of these two measures. LAGB and non-LAGB patients were propensity score matched (according to year of baseline date) on baseline BMI, age, and gender. Within each year, selected matching patients were only used for one LAGB patient. It is possible that a non-LAGB patient selected as a match for an LAGB patient one year could also be identified as a match for a different patient in a subsequent year. Estimated risk for developing general CVD (coronary death, myocardial infarction, coronary insufficiency, angina, stroke, transient ischemic attack, peripheral artery disease, and heart failure) in the subsequent 10 or 30 years was calculated by two of the following methods: using office-based non-laboratory values and using lipid values where available [14, 15]. The office-based FRS is estimated using the following variables: gender, age, systolic blood pressure (SBP), BMI, smoking status, antihypertensive treatment, and diabetes status, while the lipid-based FRS replaces BMI with total cholesterol (TC) and high-density lipoprotein (HDL) cholesterol.
Diabetes was defined by International Classification of Diseases, 9th Revision (ICD-9) diagnosis and use of hypoglycemic medications (measured at baseline and 12–15 months). Remissions were defined as cessation of hypoglycemic medications.
Statistical Analysis
Changes in components of the Framingham CVD risk algorithms (BMI, SBP, TC, HDL, and diabetes) were also assessed. Changes were evaluated using paired (within group) or independent sample (between group) t tests for continuous measures and using Chi square test of proportions for categorical variables. Changes in outcome measures at 1 year were calculated using an average of values between 12 and 15 months. In addition, changes in CVD risk factors and scores were evaluated for subgroups stratified by gender and baseline BMI.
In order to assess individual contributions to changes in risk scores among LAGB patients, variables were assessed using a stepwise regression model and F statistics were calculated. P-values <0.05 were considered statistically significant. Data manipulation and statistical analyses were performed using SAS® (version 9.2, SAS Institute, Cary, NC, USA).
Results
A sample of 2,186 patients aged 30–73 years, with BMI ≥30 kg/m2, with LAGB after 2005, and 12–15 months of follow-up was identified in the MQIC database. Of these, 647 LAGB patients also had BMI measures at follow-up. A matched comparison group of 4,295 patients without surgical weight loss intervention was also identified.
Baseline Measures
Patient characteristics and CVD risk factor distributions at baseline and follow-up are presented in Table 1. At baseline, LAGB patients were more likely to have diabetes than comparison patients (15.5 and 8.4%, respectively), while SBP was similar in both groups. Using office-based measures, the estimated 10- and 30-year Framingham CVD risks were 10.8 and 44.34% for LAGB patients and 10.56 and 41.79% for comparison patients at baseline, respectively.
Changes in Measures at Follow-Up
At 12–15 months’ follow-up, mean BMI decreased significantly in LAGB patients (−9.3 kg/m2, P < 0.0001) and in comparison patients (−0.6 kg/m2, P < 0.0001; Table 1). In addition, there were significant reductions in SBP for both LAGB (P < 0.0001) and comparison patients (P < 0.05). At follow-up, the proportion of patients using anti-diabetic medications decreased in LAGB patients (P < 0.0001) and increased in comparison group (P < 0.01). Estimated 10- and 30-year CVD risk scores decreased significantly in LAGB patients (−3.2%, P < 0.0001 and −12.04%, P < 0.0001, respectively), but did not change significantly in comparison patients (+0.01%, P = 0.91 and +0.13%, P = 0.42, respectively).
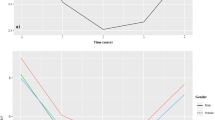
Seventy-four LAGB and 319 comparison patients had lipid data at baseline and follow-up. The LAGB subset with lipid data were older (P = 0.05), more likely to be male (P = 0.01), and have diabetes (P = 0.02) than patients without lipid data. In addition to BMI and SBP improvements, significant reductions in TC and HDL cholesterol occurred in both LAGB and comparison patients. The proportion of LAGB patients using anti-diabetic medications at follow-up decreased (P = 0.08), whereas this proportion increased among comparison patients (P = 0.28). Using lipid-based measures, estimated 10- and 30-year CVD risk decreased significantly in LAGB (−4.1%, P < 0.0001 and −11.55%, P < 0.0001, respectively) and comparison patients (−1.0%, P = 0.005 and −1.87%, P = 0.002, respectively; Table 2). Direct comparison of office-based and lipid-based estimated 10- and 30-year CVD risk in the group with lipid data indicated that office-based calculations tended to estimate risk higher than lipid-based calculations. Mean (SD) estimated 10-year CVD risk in the 74 LAGB patients with lipid data available was 15.2% (12.8) and 9.7% (6.9) using office-based and lipid-based calculations, respectively, at baseline (t = 3.2; P = 0.002) and 9.7% (9.1) and 5.6% (4.8), respectively, at follow-up (t = 3.4; P < 0.001). Mean (SD) estimated 30-year CVD risk in the 74 LAGB patients with lipid data available was 54.3% (23.6) and 34.3% (15.0) for office- and lipid-based calculations, respectively, at baseline (t = 6.2; P < 0.001) and 38.4% (24.0) and 22.73% (12.7), respectively, at follow-up (t = 4.9; P < 0.001). At follow-up, consistent relative risk reductions (−29.6 and −42.3% for 10-year CVD risk, −27.1 and −33.7% for 30-year CVD risk) were observed for either office- or lipid-based calculations, respectively (Fig. 1).
Relative change in CVD risk factors, and estimated 10- and 30-year CVD risk at 12–15 months. BMI body mass index, CVD cardiovascular disease, HDL high-density lipoprotein, LAGB laparoscopic adjustable gastric banding, SBP systolic blood pressure. Asterisk estimated 10- and 30-year CVD risk calculated using office-based algorithms for all patients, and using lipid-based algorithms for patients with lab measures [18, 19]
Between group comparisons of estimated CVD risk changes indicated that LAGB patients experienced significantly greater improvements than non-LAGB patients in 10- and 30-year CVD risk for both office-based (P < 0.0001) and lipid-based (P < 0.001) assessments (Fig. 2).
Change in estimated 10- and 30-year CVD risk at 12–15 months, LAGB versus non-LAGB patients. CVD cardiovascular disease, LAGB laparoscopic adjustable gastric banding. P values reported for difference between LAGB and non-LAGB patients. Asterisk estimated 10- and 30-year CVD risk calculated using office-based algorithms for all patients, and using lipid-based algorithms for patients with lab measures [18, 19]
Subgroup Analyses
Changes in CVD risk factors and scores were evaluated for subgroups stratified by gender and baseline BMI (Fig. 3). Reductions in risk factors and estimated CVD risk were consistently observed for all LAGB as compared with non-LAGB groups, with the exception of lipid-based estimated CVD risks for patients with BMI 30 to <35 kg/m2 (n = 5) and BMI 35 to <40 kg/m2 (n = 16), though insufficient sample sizes may have limited statistical power in these groups. Overall, males and those with baseline BMI ≥40 kg/m2 experienced the greatest absolute risk reductions.
Factors Driving Risk Reduction
The main drivers of estimated 10-year CVD risk reduction among LAGB patients were baseline CVD risk (F = 478.6; P < 0.0001), SBP (F = 182.4; P < 0.0001), and BMI (F = 38.4; P < 0.0001) for office-based measures analysis, and baseline CVD risk (F = 113.8; P < 0.0001), TC (F = 22.5; P < 0.0001), and HDL (F = 12.5; P = 0.0007) for lipid-based measures analysis. The main drivers of estimated 30-year CVD risk reduction were baseline CVD risk (F = 308.9; P < 0.0001), BMI (F = 236.0; P < 0.0001), and SBP (F = 116.0; P < 0.0001) for office-based measures analysis, and TC (F = 69.6; P < 0.0001), baseline CVD risk (F = 56.0; P < 0.0001), and HDL (F = 23.2; P < 0.0001) for lipid-based measures analysis.
Discussion
Cardiovascular diseases are among the most significant health consequences of obesity. In this analysis, without intervention, approximately 44% of obese patients who underwent the LAGB procedure would be predicted to experience CVD over the subsequent 30 years. These LAGB patients experienced both significant weight loss and improvements in CVD risk factors, including SBP, total and HDL cholesterol, and diabetes. One year after the LAGB procedure, patients reduced their estimated risk of developing CVD over the next 10–30 years by approximately one-third.
Improvements in estimated CVD risk among LAGB patients also were significantly greater than among matched patients who did not undergo LAGB. Modest improvements in some CVD risk factors were observed in comparison patients, including SBP and lipids, which might be attributed to lifestyle or pharmacologic interventions. However, the proportion of patients with diabetes increased in non-LAGB patients, which may have adversely impacted CVD risk scores in this group.
Multivariate risk prediction algorithms such as those developed within FHS allow clinicians to predict short- and long-term CVD risk for patients to help guide medical decision-making. The consistency of observed CVD risk reduction using lipid-based algorithms among the subset with lipid data strengthens results, as this algorithm was not based on changes in BMI. However, a limitation of the study was the small sample with lipid data available and it is noted that the predicted CVD risk was higher for the office-based algorithms.
These findings are substantiated by recent results from the Swedish Obese Subjects study, a prospective, non-randomized study of obese patients treated with either bariatric surgery (19% with banding) or non-surgical intervention with median follow-up of 14.7 years. Among bariatric surgery patients, risk of total and fatal CV events was reduced by 33 and 53%, respectively, as compared with control patients after adjusting for baseline conditions [24]. In addition, a recent systematic review and meta-analysis of studies reporting long-term mortality in morbid obesity among bariatric surgery patients reported significant reduced overall mortality in three studies and borderline reduced CVD mortality among two studies reviewed for LAGB procedure [25]. Previous studies have demonstrated an association between increasing BMI and both overall and CVD-specific mortality [26–28], and weight loss has been consistently demonstrated to improve CVD risk factors, including hypertension, type 2 diabetes, and dyslipidemia [29–33]. In addition to improving CVD risk factors for individuals with comorbidities at time of intervention, weight loss is also associated with reduced risk of developing type 2 diabetes (58–88% risk reduction) [7, 32], low HDL cholesterol (43–79% risk reduction) [7], hypertension (45% risk reduction) [9], hypertriglyceridemia (49–71% risk reduction) [7], metabolic syndrome (41% risk reduction) [30], and stroke (22% risk reduction) [34].
Significant weight loss after bariatric surgery is accompanied by substantial reductions in CVD risk factors [7–9, 35] and overall mortality [7, 36]. Previous studies following other bariatric surgical procedures have also demonstrated significant reductions in predicted risk of CHD using FRS [19]. Obese patients who receive bariatric surgery experience an overall decrease in Framingham 10-year CHD risk score of 2.0–3.5 points [20–22]. In comparison, a study examining Framingham CVD risk following lifestyle and pharmacological intervention with orlistat did not report significant reduction in predicted CVD risk at 1 year of follow-up [23]. The present report is distinguished from and adds to previous investigations in terms of three significant approaches: (1) use of general CVD algorithms (including stroke and peripheral artery disease) rather than the more limited CHD algorithm, (2) use of 30-year Framingham risk prediction algorithms that may approximate lifetime risk for a younger patient population, and (3) estimating risk after the LAGB procedure.
The strengths of this analysis include the observational setting that utilized a large database of patients that are likely to be representative of US patients undergoing LAGB. Patients studied in this report reflect the following typical characteristics of LAGB patients: they are primarily female [37], aged in their mid-40s [37, 38], with mean BMI of ~43–45 kg/m2 [38–40]. An additional strength of the study was the availability of a matched comparator group of obese patients who did not undergo surgical weight loss intervention. While lack of a randomized controlled design could be criticized, the practical and ethical nature of such a design is questionable and the propensity matched design is considered a strength to try to ensure comparability between the groups. However, because the design was non-randomized, differences between LAGB and non-LAGB patients other than matched characteristics could have existed (such as the unequal distribution of diabetes at baseline) and influenced results, although within group changes would not have been affected by the non-randomized design. Other limitations of the study include lack of data on lifestyle changes or pharmacologic interventions beyond those used for hypertension and diabetes management. Non-LAGB patients were expected to receive non-surgical standard of care, including lifestyle and pharmacologic interventions. Also, requiring 12–15 months of follow-up may have introduced selection bias, as it was unclear whether these patients were similar to patients who did not have the required follow-up. Furthermore, adverse events due to the LAGB procedure were not included in the analysis. Framingham CVD risk scores have not been validated for measuring changes in CVD risk over time or specifically in obese populations; however, in the present analysis scores based on BMI versus lipid data indicate similar and consistent magnitude of risk reduction. In addition, patients older than 59 years were included and the estimation procedure for 30-year CVD risk algorithm was developed on a sample aged 20–59 years [15].
The predicted risk reductions assume patients would maintain the weight loss and improvements in risk factors over time; however, without longer-term follow-up, the authors cannot confirm this would be the case. However, several studies have demonstrated long-term weight loss maintenance among LAGB treated patients 4–12 years after the procedure [11, 12].
Conclusion
In conclusion, data from a large US healthcare database show patients receiving LAGB to have significant weight loss, and reduced CVD risk factors and estimated CVD risk, supporting the effectiveness of the LAGB procedure as a potential approach for management of obesity. These results add to the evidence of the cardiovascular benefits of significant weight loss among obese individuals and the potential long-term clinical impact of the LAGB procedure as a therapeutic intervention for obesity. Larger and long-term studies are needed to further document whether effects of LAGB on weight loss and CVD risk factors translate into reduced CVD incidence.
References
Roger VL, Go AS, Lloyd-Jones DM, American Heart Association Statistical Committee and Stroke Statistics Committee, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–209.
Heidenreich PA, Trogdon JG, Khavjou OA, The American Heart Association Advocacy Coordinating Committee, Stroke Council, Council on Cardiovascular Radiology and Intervention, Council on Clinical Cardiology, Council on Epidemiology and Prevention, Council on Arteriosclerosis, Thrombosis and Vascular Biology, Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, Council on Cardiovascular Nursing, Council on the Kidney in Cardiovascular Disease, Council on Cardiovascular Surgery and Anesthesia, Interdisciplinary Council on Quality of Care and Outcomes Research, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–44.
CDC/NCHS. National Health and Nutrition Examination Survey Data. Centers for Disease Control and Prevention (CDC) and National Center for Health Statistics (NCHS) 2011. Available at http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm. Last accessed 25 April 2012.
Poirier P, Giles TD, Bray GA, American Heart Association Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;2006(113):898–918.
Dattilo AM, Kris-Etherton PM. Effects of weight reduction on blood lipids and lipoproteins: a meta-analysis. Am J Clin Nutr. 1992;56:320–8.
Eilat-Adar S, Eldar M, Goldbourt U. Association of intentional changes in body weight with coronary heart disease event rates in overweight subjects who have an additional coronary risk factor. Am J Epidemiol. 2005;161:352–8.
Sjostrom L, Lindroos AK, Peltonen M, et al. Swedish Obesity Subjects Study Scientific Group. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–93.
Woodard GA, Peraza J, Bravo S, Toplosky L, Hernandez-Boussard T, Morton JM. One year improvements in cardiovascular risk factors: a comparative trial of laparoscopic Roux-en-Y gastric bypass vs. adjustable gastric banding. Obes Surg. 2010;20:578–82.
Huang Z, Willett WC, Manson JE, et al. Body weight, weight change, and risk for hypertension in women. Ann Intern Med. 1998;128:81–8.
Society of American Gastrointestinal and Endoscopic Surgeons. SAGES guideline for clinical application of laparoscopic bariatric surgery. Surg Obes Relat Dis. 2009;5:387–405.
Favretti F, Segato G, Ashton D, et al. Laparoscopic adjustable gastric banding in 1,791 consecutive obese patients: 12-year results. Obes Surg. 2007;17:168–75.
O’Brien PE, McPhail T, Chaston TB, Dixon JB. Systematic review of medium-term weight loss after bariatric operations. Obes Surg. 2006;16:1032–40.
Poirier P, Cornier MA, Mazzone T, et al. American Heart Association Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Bariatric surgery and cardiovascular risk factors: a scientific statement from the American Heart Association. Circulation. 2011;123:1683–701.
D’Agostino RB Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart study. Circulation. 2008;117:743–53.
Pencina MJ, D’Agostino RB Sr, Larson MG, Massaro JM, Vasan RS. Predicting the 30-year risk of cardiovascular disease: the Framingham heart study. Circulation. 2009;119:3078–84.
Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–47.
Nguyen NT, Nguyen XM, Wooldridge JB, Slone JA, Lane JS. Association of obesity with risk of coronary heart disease: findings from the National Health and Nutrition Examination Survey, 1999-2006. Surg Obes Relat Dis. 2010;6:465–9.
Arterburn D, Schauer DP, Wise RE, et al. Change in predicted 10-year cardiovascular risk following laparoscopic Roux-en-Y gastric bypass surgery. Obes Surg. 2009;19:184–9.
Heneghan HM, Meron-Eldar S, Brethauer SA, Schauer PR, Young JB. Effect of Bariatric surgery on cardiovascular risk profile. Am J Cardiol. 2011;108:1499–507.
Kligman MD, Dexter DJ, Omer S, Park AE. Shrinking cardiovascular risk through bariatric surgery: application of Framingham risk score in gastric bypass. Surgery. 2008;143:533–8.
Torquati A, Wright K, Melvin W, Richards W. Effect of gastric bypass operation on Framingham and actual risk of cardiovascular events in class II to III obesity. J Am Coll Surg. 2007;204:776–82.
Vogel JA, Franklin BA, Zalesin KC, et al. Reduction in predicted coronary heart disease risk after substantial weight reduction after bariatric surgery. Am J Cardiol. 2007;99:222–6.
Swinburn BA, Carey D, Hills AP, et al. Effect of orlistat on cardiovascular disease risk in obese adults. Diabetes Obes Metab. 2005;7:254–62.
Sjostrom L, Peltonen M, Jacobson P, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307:56–65.
Pontiroli AE, Morabito A. Long-term prevention of mortality in morbid obesity through bariatric surgery. a systematic review and meta-analysis of trials performed with gastric banding and gastric bypass. Ann Surg. 2011;253:484–7.
Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW Jr. Body-mass index and mortality in a prospective cohort of US adults. N Engl J Med. 1999;341:1097–105.
de Gonzalez BA, Hartge P, Cerhan JR, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010;363:2211–9.
Prospective Studies Collaboration, Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900,000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–96.
Diabetes Prevention Program Research Group, Knowler WC, Fowler SE, Hamman RF, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374:1677–86.
Orchard TJ, Temprosa M, Goldberg R, et al. The effect of metformin and intensive lifestyle intervention on the metabolic syndrome: the Diabetes Prevention Program randomized trial. Ann Intern Med. 2005;142:611–9.
Ratner R, Goldberg R, Haffner S, et al. Impact of intensive lifestyle and metformin therapy on cardiovascular disease risk factors in the diabetes prevention program. Diabetes Care. 2005;28:888–94.
Tuomilehto J, Lindstrom J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–50.
Wing RR. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med. 2010;170:1566–75.
Rexrode KM, Hennekens CH, Willett WC, Colditz GA, Stampfer MJ, Rich-Edwards JW, et al. A prospective study of body mass index, weight change, and risk of stroke in women. JAMA. 1997;277(19):1539–45.
Dixon JB, O’Brien PE, Playfair J, et al. Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA. 2008;299:316–23.
Sjostrom L, Narbro K, Sjostrom CD, et al. Swedish Obese Subjects Study. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52.
Hinojosa MW, Varela JE, Parikh D, Smith BR, Nguyen XM, Nguyen NT. National trends in use and outcome of laparoscopic adjustable gastric banding. Surg Obes Relat Dis. 2009;5:150–5.
Weichman K, Ren C, Kurian M, et al. The effectiveness of adjustable gastric banding: a retrospective 6-year US follow-up study. Surg Endosc. 2011;25:397–403.
Cunneen SA. Review of meta-analytic comparisons of bariatric surgery with a focus on laparoscopic adjustable gastric banding. Surg Obes Relat Dis. 2008;4(3 Suppl):S47–55.
Inabnet WB III, Winegar DA, Sherif B, Sarr MG. Early outcomes of bariatric surgery in patients with metabolic syndrome: an analysis of the bariatric outcomes longitudinal database. J Am Coll Surg. 2012;214:550–6.
Acknowledgments
The authors thank Ruth Quah, GE Healthcare, for programming and analysis support. Editorial assistance with copyediting and manuscript submission was provided by Susan M. Kaup, PhD, Evidence Scientific Solutions, funded by Allergan, Inc. The analysis and publication charges were sponsored by Allergan, Inc. Dr Largent is the guarantor for this article, and takes responsibility for the integrity of the work as a whole.
Ethical standards
The analysis in this article is based on previously collected data and does not involve any new studies of human or animal subjects performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Largent, J.A., Vasey, J., Bessonova, L. et al. Reduction in Framingham Risk of Cardiovascular Disease in Obese Patients Undergoing Laparoscopic Adjustable Gastric Banding. Adv Ther 30, 684–696 (2013). https://doi.org/10.1007/s12325-013-0045-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-013-0045-0