Abstract
Natural killer (NK) cells are attractive effector cells of the innate immune system against human immunodeficiency virus (HIV) and cancer. However, NK cell therapies are limited by the fact that target cells evade NK cells, for example, in latent reservoirs (in HIV) or through upregulation of inhibitory signals (in cancer). To address this limitation, we describe a biodegradable nanoparticlebased “priming” approach to enhance the cytotoxic efficacy of peripheral blood mononuclear cell-derived NK cells. We present poly(lactic-co-glycolic acid) (PLGA) nanodepots (NDs) that co-encapsulate prostratin, a latency-reversing agent, and anti-CD25 (aCD25), a cell surface binding antibody, to enhance primary NK cell function against HIV and cancer. We utilize a nanoemulsion synthesis scheme to encapsulate both prostratin and aCD25 within the PLGA NDs (termed Pro-aCD25-NDs). Physicochemical characterization studies of the NDs demonstrated that our synthesis scheme resulted in stable and monodisperse Pro-aCD25- NDs. The NDs successfully released both active prostratin and anti-CD25, and with controllable release kinetics. When Pro-aCD25-NDs were administered in an in vitro model of latent HIV and acute T cell leukemia using J-Lat 10.6 cells, the NDs were observed to prime J-Lat cells resulting in significantly increased NK cell-mediated cytotoxicity compared to free prostratin plus anti-CD25, and other controls. These findings demonstrate the feasibility of using our Pro-aCD25-NDs to prime target cells for enhancing the cytotoxicity of NK cells as antiviral or antitumor agents.

Similar content being viewed by others
References
Mikulak, J.; Oriolo, F.; Zaghi, E.; Di Vito, C.; Mavilio, D. Natural killer cells in HIV-1 infection and therapy. AIDS2017, 31, 2317–2330.
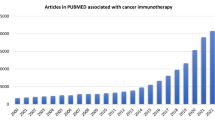
Guillerey, C.; Huntington, N. D.; Smyth, M. J. Targeting natural killer cells in cancer immunotherapy. Nat. Immunol.2016, 17, 1025–1036.
Breunig, M.; Lungwitz, U.; Liebl, R.; Goepferich, A. Breaking up the correlation between efficacy and toxicity for nonviral gene delivery. Proc. Natl. Acad. Sci. USA2007, 104, 14454–14459.
Daher, M.; Rezvani, K. Next generation natural killer cells for cancer immunotherapy: The promise of genetic engineering. Curr. Opin. Immunol.2018, 51, 146–153.
Florea, B. I.; Meaney, C.; Junginger, H. E.; Borchard, G. Transfection efficiency and toxicity of polyethylenimine in differentiated Calu-3 and nondifferentiated COS-1 cell cultures. AAPS PharmSci2002, 4, 1–11.
Kafil, V.; Omidi, Y. Cytotoxic impacts of linear and branched polyethylenimine nanostructures in a431 cells. Bioimpacts2011, 1, 23–30.
De Maria, A.; Fogli, M.; Costa, P.; Murdaca, G.; Puppo, F.; Mavilio, D.; Moretta, A.; Moretta, L. The impaired NK cell cytolytic function in viremic HIV-1 infection is associated with a reduced surface expression of natural cytotoxicity receptors (NKp46, NKp30 and NKp44). Eur. J. Immunol.2003, 33, 2410–2418.
Katz, J. D.; Mitsuyasu, R.; Gottlieb, M. S.; Lebow, L. T.; Bonavida, B. Mechanism of defective NK cell activity in patients with acquired immunodeficiency syndrome (AIDS) and AIDS-related complex. II. Normal antibody-dependent cellular cytotoxicity (ADCC) mediated by effector cells defective in natural killer (NK) cytotoxicity. J. Immunol.1987, 139, 55–60.
Cheng, J. J.; Teply, B. A.; Sherifi, I.; Sung, J.; Luther, G.; Gu, F. X.; Levy-Nissenbaum, E.; Radovic-Moreno, A. F.; Langer, R.; Farokhzad, O. C. Formulation of functionalized PLGA-PEG nanoparticles for in vivo targeted drug delivery. Biomaterials2007, 28, 869–876.
Li, Y. P.; Pei, Y. Y.; Zhang, X. Y.; Gu, Z. H.; Zhou, Z. H.; Yuan, W. F.; Zhou, J. J.; Zhu, J. H.; Gao, X. J. PEGylated PLGA nanoparticles as protein carriers: Synthesis, preparation and biodistribution in rats. J. Control. Release2001, 71, 203–211.
Gdowski, A.; Ranjan, A.; Mukerjee, A.; Vishwanatha, J. Development of biodegradable nanocarriers loaded with a monoclonal antibody. Int. J. Mol. Sci.2015, 16, 3990–3995.
Langer, R.; Folkman, J. Polymers for the sustained release of proteins and other macromolecules. Nature1976, 263, 797–800.
Spivak, A. M.; Planelles, V. Novel latency reversal agents for HIV-1 cure. Annu. Rev. Med.2018, 69, 421–436.
Kulkosky, J.; Culnan, D. M.; Roman, J.; Dornadula, G.; Schnell, M.; Boyd, M. R.; Pomerantz, R. J. Prostratin: Activation of latent HIV-1 expression suggests a potential inductive adjuvant therapy for HAART. Blood2001, 98, 3006–3015.
Desimio, M. G.; Giuliani, E.; Ferraro, A. S.; Adorno, G.; Doria, M. In vitro exposure to prostratin but not bryostatin-1 improves natural killer cell functions including killing of CD4+ T cells harboring reactivated human immunodeficiency virus. Front. Immunol.2018, 9, 1514.
Makadia, H. K.; Siegel, S. J. Poly lactic-co-glycolic acid (PLGA) as biodegradable controlled drug delivery carrier. Polymers2011, 3, 1377–1397.
Danhier, F.; Ansorena, E.; Silva, J. M.; Coco, R.; Le Breton, A.; Préat, V. PLGA-based nanoparticles: An overview of biomedical applications. J. Control. Release2012, 161, 505–522.
Español, L.; Larrea, A.; Andreu, V.; Mendoza, G.; Arruebo, M.; Sebastian, V.; Aurora-Prado, M. S.; Kedor-Hackmann, E. R. M.; Santoro, M. I. R. M.; Santamaria, J. Dual encapsulation of hydrophobic and hydrophilic drugs in PLGA nanoparticles by a single-step method: Drug delivery and cytotoxicity assays. RSC Adv.2016, 6, 111060–111069.
Goldberg, M. S. Immunoengineering: How nanotechnology can enhance cancer immunotherapy. Cell2015, 161, 201–204.
Martínez Rivas, C. J.; Tarhini, M.; Badri, W.; Miladi, K.; Greige- Gerges, H.; Nazari, Q. A.; Galindo Rodríguez, S. A.; Román, R. Á.; Fessi, H.; Elaissari, A. Nanoprecipitation process: From encapsulation to drug delivery. Int. J. Pharm.2017, 532, 66–81.
Astete, C. E.; Sabliov, C. M. Synthesis and characterization of PLGA nanoparticles. J. Biomat. Sci., Polym Ed.2006, 17, 247–289.
Wang, W.; Erbe, A. K.; Hank, J. A.; Morris, Z. S.; Sondel, P. M. NK Cell-mediated antibody-dependent cellular cytotoxicity in cancer immunotherapy. Front. Immunol.2015, 6, 368.
Ramilo, O.; Bell, K. D.; Uhr, J. W.; Vitetta, E. S. Role of CD25+ and CD25- T cells in acute HIV infection in vitro.J. Immunol.1993, 150, 5202–5208.
Arce Vargas, F.; Furness, A. J. S.; Solomon, I.; Joshi, K.; Mekkaoui, L.; Lesko, M. H.; Miranda Rota, E.; Dahan, R.; Georgiou, A.; Sledzinska, A. et al. Fc-optimized Anti-CD25 depletes tumorinfiltrating regulatory T cells and synergizes with PD-1 blockade to eradicate established tumors. Immunity2017, 46, 577–586.
Flynn, M. J.; Hartley, J. A. The emerging role of anti-CD25 directed therapies as both immune modulators and targeted agents in cancer. Brit. J. Haematol.2017, 179, 20–35.
Jordan, A.; Bisgrove, D.; Verdin, E. HIV reproducibly establishes a latent infection after acute infection of T cells in vitro.EMBO J.2003, 22, 1868–1877.
Chen, M. S.; Ouyang, H. C.; Zhou, S. Y.; Li, J. Y.; Ye, Y. B. PLGA-nanoparticle mediated delivery of anti-OX40 monoclonal antibody enhances anti-tumor cytotoxic T cell responses. Cell. Immunol.2014, 287, 91–99.
Sousa, F.; Cruz, A.; Pinto, I. M.; Sarmento, B. Nanoparticles provide long-term stability of bevacizumab preserving its antiangiogenic activity. Acta Biomater.2018, 78, 285–295.
Feczkó, T.; Tóth, J.; Dósa, G.; Gyenis, J. Optimization of protein encapsulation in PLGA nanoparticles. Chem. Eng. Process.2011, 50, 757–765.
Son, S.; Lee, W. R.; Joung, Y. K.; Kwon, M. H.; Kim, Y. S.; Park, K. D. Optimized stability retention of a monoclonal antibody in the PLGA nanoparticles. Int. J. Pharm.2009, 368, 178–185.
Lee, Y. H.; Lai, Y. H. Synthesis, characterization, and biological evaluation of anti-HER2 indocyanine green-encapsulated PEGcoated PLGA nanoparticles for targeted phototherapy of breast cancer cells. PLoS One2016, 11, e0168192.
Lee, Y. H.; Chang, D. S. Fabrication, characterization, and biological evaluation of anti-HER2 indocyanine green-doxorubicin-encapsulated PEG-b-PLGA copolymeric nanoparticles for targeted photochemotherapy of breast cancer cells. Sci. Rep.2017, 7, 46688.
Sainz, V.; Peres, C.; Ciman, T.; Rodrigues, C.; Viana, A. S.; Afonso, C. A. M.; Barata, T.; Brocchini, S.; Zloh, M.; Gaspar, R. S. et al. Optimization of protein loaded PLGA nanoparticle manufacturing parameters following a quality-by-design approach. RSC Adv.2016, 6, 104502–104512.
Fonte, P.; Soares, S.; Costa, A.; Andrade, J. C.; Seabra, V.; Reis, S.; Sarmento, B. Effect of cryoprotectants on the porosity and stability of insulin-loaded PLGA nanoparticles after freeze-drying. Biomatter.2012, 2, 329–339.
Hines, D. J.; Kaplan, D. L. Poly(lactic-co-glycolic) acid-controlledrelease systems: Experimental and modeling insights. Crit. Rev. Ther. Drug. Carrier Syst.2013, 30, 257–276.
Fredenberg, S.; Wahlgren, M.; Reslow, M.; Axelsson, A. The mechanisms of drug release in poly(lactic-co-glycolic acid)-based drug delivery systems-a review. Int. J. Pharm.2011, 415, 34–52.
Jeong, B.; Bae, Y. H.; Kim, S. W. Drug release from biodegradable injectable thermosensitive hydrogel of PEG-PLGA-PEG triblock copolymers. J. Control. Release2000, 63, 155–163.
Faisant, N.; Siepmann, J.; Richard, J.; Benoit, J. P. Mathematical modeling of drug release from bioerodible microparticles: Effect of gamma-irradiation. Eur. J. Pharm. Biopharm.2003, 56, 271–279.
Williams, S. A.; Chen, L. F.; Kwon, H.; Fenard, D.; Bisgrove, D.; Verdin, E.; Greene, W. C. Prostratin antagonizes HIV latency by activating NF-?B. J. Biol. Chem.2004, 279, 42008–42017.
Spina, C. A.; Anderson, J.; Archin, N. M.; Bosque, A.; Chan, J.; Famiglietti, M.; Greene, W. C.; Kashuba, A.; Lewin, S. R.; Margolis, D. M. et al. An in-depth comparison of latent HIV-1 reactivation in multiple cell model systems and resting CD4+ T cells from aviremic patients. PLoS Pathog.2013, 9, e1003834.
Lv, S. X.; Tang, Z. H.; Li, M. Q.; Lin, J.; Song, W. T.; Liu, H. Y.; Huang, Y. B.; Zhang, Y. Y.; Chen, X. S. Co-delivery of doxorubicin and paclitaxel by PEG-polypeptide nanovehicle for the treatment of non-small cell lung cancer. Biomaterials2014, 35, 6118–6129.
Guo, S. T.; Lin, C. M.; Xu, Z. H.; Miao, L.; Wang, Y. H.; Huang, L. Co-delivery of cisplatin and rapamycin for enhanced anticancer therapy through synergistic effects and microenvironment modulation. ACS Nano2014, 8, 4996–5009.
Wang, Y.; Gao, S. J.; Ye, W. H.; Yoon, H. S.; Yang, Y. Y. Codelivery of drugs and DNA from cationic core-shell nanoparticles self-assembled from a biodegradable copolymer. Nat. Mater.2006, 5, 791–796.
Fujisaki, H.; Kakuda, H.; Shimasaki, N.; Imai, C.; Ma, J.; Lockey, T.; Eldridge, P.; Leung, W. H.; Campana, D. Expansion of highly cytotoxic human natural killer cells for cancer cell therapy. Cancer Res.2009, 69, 4010–4017.
Cho, D.; Campana, D. Expansion and activation of natural killer cells for cancer immunotherapy. Korean J. Lab. Med.2009, 29, 89–96.
Acknowledgements
Research reported in this publication was supported in part by the George Washington Cancer Center and by the National Institute Of Allergy And Infectious Diseases of the National Institutes of Health under Award Number R21AI136102. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
12274_2020_2684_MOESM1_ESM.pdf
PLGA nanodepots co-encapsulating prostratin and anti-CD25 enhance primary natural killer cell antiviral and antitumor function
Rights and permissions
About this article
Cite this article
Sweeney, E.E., Balakrishnan, P.B., Powell, A.B. et al. PLGA nanodepots co-encapsulating prostratin and anti-CD25 enhance primary natural killer cell antiviral and antitumor function. Nano Res. 13, 736–744 (2020). https://doi.org/10.1007/s12274-020-2684-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12274-020-2684-1