Abstract
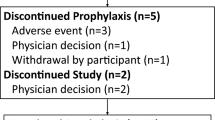
Despite the recent introduction of a new class of anti-Aspergillus agents, no standard regimen for the prevention of invasive fungal disease (IFD) following allogeneic hematopoietic stem cell transplantation has been shown to be superior to fluconazole. The present prospective, single-arm study investigated the feasibility of voriconazole (VOR) administration as primary prophylaxis in 52 recipients of umbilical cord blood transplantation (CBT) with fludarabine-based conditioning, who had no previous IFD episodes. Proven or probable IFD was determined using the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group, and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) criteria were considered as breakthrough infections. VOR was administered as prophylaxis for a total of 6884 patient-days following CBT. The mean duration of VOR administration after transplantation was 132 days (range, 1–769); 44 patients (85 %) had advanced disease, 15 (29 %) had a history of allogeneic HSCT, and 29 (56 %) received systemic corticosteroid therapy for allogeneic immune-mediated complications. Under the prophylaxis with VOR, one patient developed probable invasive aspergillosis on day 71, and the cumulative incidence of IFD was 4.5 % at day 180. None of the patients developed breakthrough candida or zygomycetes infections. Under the extensive therapeutic dose monitoring, VOR was safely administered with a calcineurin inhibitor and was well tolerated. These results suggest that VOR represents a feasible primary prophylactic agent for IFD after CBT with fludarabine-based conditioning.


Similar content being viewed by others
References
Kurokawa M, Yonezumi M, Hashino S, Tanaka J, Nishio M, Kaneda M, et al. Epidemiology and treatment outcome of invasive fungal infections in patients with hematological malignancies. Int J Hematol. 2012;96(6):748–57.
Marr KA, Carter RA, Crippa F, Wald A, Corey L. Epidemiology and outcome of mould infections in hematopoietic stem cell transplant recipients. Clin Infect Dis. 2002;34(7):909–17.
Marr KA, Carter RA, Boeckh M, Martin P, Corey L. Invasive aspergillosis in allogeneic stem cell transplant recipients: changes in epidemiology and risk factors. Blood. 2002;100(13):4358–66.
Chamilos G, Luna M, Lewis RE, Bodey GP, Chemaly R, Tarrand JJ, et al. Invasive fungal infections in patients with hematologic malignancies in a tertiary care cancer center: an autopsy study over a 15-year period (1989–2003). Haematologica. 2006;91(7):986–9.
Marco F, Pfaller MA, Messer SA, Jones RN. Antifungal activity of a new triazole, voriconazole (UK-109,496), compared with three other antifungal agents tested against clinical isolates of filamentous fungi. Med Mycol. 1998;36(6):433–6.
Marco F, Pfaller MA, Messer S, Jones RN. In vitro activities of voriconazole (UK-109,496) and four other antifungal agents against 394 clinical isolates of Candida spp. Antimicrob Agents Chemother. 1998;42(1):161–3.
Wingard JR, Carter SL, Walsh TJ, Kurtzberg J, Small TN, Baden LR, et al. Randomized, double-blind trial of fluconazole versus voriconazole for prevention of invasive fungal infection after allogeneic hematopoietic cell transplantation. Blood. 2010;116(24):5111–8.
Martino R, Parody R, Fukuda T, Maertens J, Theunissen K, Ho A, et al. Impact of the intensity of the pretransplantation conditioning regimen in patients with prior invasive aspergillosis undergoing allogeneic hematopoietic stem cell transplantation: a retrospective survey of the infectious diseases working party of the European group for blood and marrow transplantation. Blood. 2006;108(9):2928–36.
Safdar A, Rodriguez GH, De Lima MJ, Petropoulos D, Chemaly RF, Worth LL, et al. Infections in 100 cord blood transplantations: spectrum of early and late posttransplant infections in adult and pediatric patients 1996–2005. Med (Baltimore). 2007;86(6):324–33.
De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, et al. Revised definitions of invasive fungal disease from the European organization for research and treatment of cancer/invasive fungal infections cooperative group and the National institute of allergy and infectious diseases mycoses study group (EORTC/MSG) consensus group. Clin Infect Dis. 2008;46(12):1813–21.
Hughes WT, Armstrong D, Bodey GP, Bow EJ, Brown AE, Calandra T, et al. 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis. 2002;34(6):730–51.
Kishi Y, Kami M, Miyakoshi S, Kanda Y, Murashige N, Teshima T, et al. Early immune reaction after reduced-intensity cord-blood transplantation for adult patients. Transplantation. 2005;80(1):34–40.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 consensus conference on acute GVHD grading. Bone Marrow Transpl. 1995;15(6):825–8.
Sullivan KM, Agura E, Anasetti C, Appelbaum F, Badger C, Bearman S, et al. Chronic graft-versus-host disease and other late complications of bone marrow transplantation. Semin Hematol. 1991;28(3):250–9.
National Cancer Institute (2006) Serious adverse events definitions: National Cancer Institute online guidelines. available at: http://www.ctep.cancer.gov.
Gooley TA, Leisenring W, Crowley J, Storer BE. Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med. 1999;18(6):695–706.
Miyakoshi S, Kusumi E, Matsumura T, Hori A, Murashige N, Hamaki T, et al. Invasive fungal infection following reduced-intensity cord blood transplantation for adult patients with hematologic diseases. Biol Blood Marrow Transpl. 2007;13(7):771–7.
Lewis RE. What is the “therapeutic range” for voriconazole? Clin Infect Dis. 2008;46(2):212–4.
Trifilio SM, Yarnold PR, Scheetz MH, Pi J, Pennick G, Mehta J. Serial plasma voriconazole concentrations after allogeneic hematopoietic stem cell transplantation. Antimicrob Agents Chemother. 2009;53(5):1793–6.
Capitano B, Potoski BA, Husain S, Zhang S, Paterson DL, Studer SM, et al. Intrapulmonary penetration of voriconazole in patients receiving an oral prophylactic regimen. Antimicrob Agents Chemother. 2006;50(5):1878–80.
Mori T, Aisa Y, Kato J, Nakamura Y, Ikeda Y, Okamoto S. Drug interaction between voriconazole and calcineurin inhibitors in allogeneic hematopoietic stem cell transplant recipients. Bone Marrow Transpl. 2009;44(6):371–4.
Trifilio SM, Scheetz MH, Pi J, Mehta J. Tacrolimus use in adult allogeneic stem cell transplant recipients receiving voriconazole: preemptive dose modification and therapeutic drug monitoring. Bone Marrow Transpl. 2010;45(8):1352–6.
Ratanatharathorn V, Nash RA, Przepiorka D, Devine SM, Klein JL, Weisdorf D, et al. Phase III study comparing methotrexate and tacrolimus (prograf, FK506) with methotrexate and cyclosporine for graft-versus-host disease prophylaxis after HLA-identical sibling bone marrow transplantation. Blood. 1998;92(7):2303–14.
Nash RA, Antin JH, Karanes C, Fay JW, Avalos BR, Yeager AM, et al. Phase 3 study comparing methotrexate and tacrolimus with methotrexate and cyclosporine for prophylaxis of acute graft-versus-host disease after marrow transplantation from unrelated donors. Blood. 2000;96(6):2062–8.
Oshima K, Sato M, Terasako K, Kimura S, Okuda S, Kako S, et al. Target blood concentrations of CYA and tacrolimus in randomized controlled trials for the prevention of acute GVHD after hematopoietic SCT. Bone Marrow Transpl. 2010;45(4):781–2.
Matsuno N, Wake A, Uchida N, Ishiwata K, Araoka H, Takagi S, et al. Impact of HLA disparity in the graft-versus-host direction on engraftment in adult patients receiving reduced-intensity cord blood transplantation. Blood. 2009;114(8):1689–95.
Takagi S, Masuoka K, Uchida N, Ishiwata K, Araoka H, Tsuji M, et al. High incidence of haemophagocytic syndrome following umbilical cord blood transplantation for adults. Br J Haematol. 2009;147(4):543–53.
Acknowledgments
The authors thank Pfizer Japan Inc. for measuring VOR plasma concentrations. The authors also thank all physicians, nurses, pharmacists, transplantation coordinator (Ms. Madoka Narita), data managers (Ms. Naomi Yamada, Ms. Rumiko Tsuchihashi and Ms. Kaoru Kobayashi), and support personnel for their compassionate care of the patients involved in this study, which was supported in part by the Japanese Ministry of Health, Labor and Welfare (Research Grant for Allergic Disease and Immunology H20-015).
Conflict of interest
The authors declare no competing financial interests.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Takagi, S., Araoka, H., Uchida, N. et al. A prospective feasibility study of primary prophylaxis against invasive fungal disease with voriconazole following umbilical cord blood transplantation with fludarabine-based conditioning. Int J Hematol 99, 652–658 (2014). https://doi.org/10.1007/s12185-014-1529-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-014-1529-7