Abstract
For some years, there has been interest in exploring the effects of high-fat and high-protein diets on the control of body weight. More recently, less extreme dieting paradigms have been studied, with a focus on the use of increased plant food components. This article reviews these diets from the standpoint of potential therapeutic use in cardiovascular risk reduction. We conducted a search of the literature published in 2008 and 2009 for studies assessing the effect of diet on body weight control, especially where there was an emphasis on differences in macronutrient profiles and food sources used (e.g., plant vs. animal). No clear picture emerged on the ideal macronutrient profile for weight loss and cardiovascular disease risk factor reduction. However, in general, the use of more plant food-based approaches had the greatest effect in reducing cardiovascular disease risk factors, including blood lipids and blood pressure. Alterations in the proportion of protein and fat intakes gave inconsistent effects on body weight reduction.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Foster GD, Wyatt HR, Hill JO, et al.: A randomized trial of a low-carbohydrate diet for obesity. N Engl J Med 2003, 348:2082–2090.
Samaha FF, Iqbal N, Seshadri P, et al.: A low-carbohydrate as compared with a low-fat diet in severe obesity. N Engl J Med 2003, 348:2074–2081.
Dansinger ML, Gleason JA, Griffith JL, et al.: Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. JAMA 2005, 293:43–53.
Gardner CD, Kiazand A, Alhassan S, et al.: Comparison of the Atkins, Zone, Ornish, and LEARN diets for change in weight and related risk factors among overweight premenopausal women: the A TO Z Weight Loss Study: a randomized trial. JAMA 2007, 297:969–977. (Published erratum appears in JAMA 2007, 298:178.)
Halton TL, Liu S, Manson JE, Hu FB: Low-carbohydrate-diet score and risk of type 2 diabetes in women. Am J Clin Nutr 2008, 87:339–346.
Halton TL, Willett WC, Liu S, et al.: Low-carbohydrate-diet score and the risk of coronary heart disease in women. N Engl J Med 2006, 355:1991–2002.
Keys A, Anderson JT, Grande F: Prediction of serum-cholesterol responses of man to changes in fats in the diet. Lancet 1957, 273:959–966.
Hegsted DM, McGandy RB, Myers ML, Stare FJ: Quantitative effects of dietary fat on serum cholesterol in man. Am J Clin Nutr 1965, 17:281–295.
Mensink RP, Zock PL, Kester AD, Katan MB: Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr 2003, 77:1146–1155.
Abete I, Parra D, Martinez JA: Legume-, fish-, or high-protein-based hypocaloric diets: effects on weight loss and mitochondrial oxidation in obese men. J Med Food 2009, 12:100–108.
Pipe EA, Gobert CP, Capes SE, et al.: Soy protein reduces serum LDL cholesterol and the LDL cholesterol:HDL cholesterol and apolipoprotein B:apolipoprotein A-I ratios in adults with type 2 diabetes. J Nutr 2009, 139:1700–1706.
• Key TJ, Appleby PN, Spencer EA, et al.: Mortality in British vegetarians: results from the European Prospective Investigation into Cancer and Nutrition (EPIC-Oxford). Am J Clin Nutr 2009, 89:1613S–1619S. The European Prospective Investigation into Cancer and Nutrition recruited 64,234 participants ranging from 20 to 89 years in age through the 1990s. Within the study, mortality from circulatory disease and all cause was not significantly different between vegetarians and meat eaters, although prostate cancer mortality was nonsignificantly 20% lower among vegetarians. The Study was large enough at over 16,000 vegetarians to detect substantial differences for specific causes of death; however, because these data are not in agreement with previous reports more research on this topic is required.
Key TJ, Fraser GE, Thorogood M, et al.: Mortality in vegetarians and nonvegetarians: detailed findings from a collaborative analysis of 5 prospective studies. Am J Clin Nutr 1999, 70(3 Suppl):516S–524S.
Fraser GE: Diet, Life Expectancy, and Chronic Disease: Studies of Seventh-Day Adventists and Other Vegetarians. New York: Oxford University Press; 2003.
Brinkworth GD, Noakes M, Buckley JD, et al.: Long-term effects of a very-low-carbohydrate weight loss diet compared with an isocaloric low-fat diet after 12 mo. Am J Clin Nutr 2009, 90:23–32.
Tay J, Brinkworth GD, Noakes M, et al.: Metabolic effects of weight loss on a very-low-carbohydrate diet compared with an isocaloric high-carbohydrate diet in abdominally obese subjects. J Am Coll Cardiol 2008, 51:59–67.
• Sacks FM, Bray GA, Carey VJ, et al.: Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med 2009, 360:859–873. In a 2-year study, 811 overweight adults were randomized into four different reduced-calorie diets (20% fat, 15% protein, 65% carbohydrate; 20% fat, 25% protein, 55% carbohydrate; 40% fat, 15% protein, 45% carbohydrate; 40% fat, 25% protein, 35% carbohydrate). All participants achieved clinically meaningful weight loss irrespective of their macronutrients intake. The diets improved lipid-related risk factors and fasting insulin levels.
Morgan LM, Griffin BA, Millward DJ, et al.: Comparison of the effects of four commercially available weight-loss programmes on lipid-based cardiovascular risk factors. Public Health Nutr 2009, 12:799–807.
Backes AC, Abbasi F, Lamendola C, et al.: Clinical experience with a relatively low carbohydrate, calorie-restricted diet improves insulin sensitivity and associated metabolic abnormalities in overweight, insulin resistant South Asian Indian women. Asia Pac J Clin Nutr 2008, 17:669–671.
• Chaput JP, Tremblay A, Rimm EB, et al.: A novel interaction between dietary composition and insulin secretion: effects on weight gain in the Quebec Family Study. Am J Clin Nutr 2008, 87:303–309. (Published erratum appears in Am J Clin Nutr 2008, 87:1541.). This study divided 267 adults, followed for 6 years, into tertiles based on their habitual fat intake. Comparison of the lowest with the highest fat tertile did not demonstrate differences in body weight or waist circumference. However, oral glucose tolerance tests at baseline and insulin concentration at 30 min as a proxy measure for insulin secretion showed that insulin concentrations strongly predicted body weight and waist circumference changes, especially for those on lower-fat diets.
Donnelly JE, Sullivan DK, Smith BK, et al.: Alteration of dietary fat intake to prevent weight gain: Jayhawk Observed Eating Trial. Obesity (Silver Spring) 2008, 16:107–112.
Due A, Larsen TM, Mu H, et al.: Comparison of 3 ad libitum diets for weight-loss maintenance, risk of cardiovascular disease, and diabetes: a 6-mo randomized, controlled trial. Am J Clin Nutr 2008, 88:1232–1241.
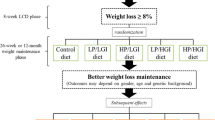
• Sloth B, Due A, Larsen TM, et al.: The effect of a high-MUFA, low-glycaemic index diet and a low-fat diet on appetite and glucose metabolism during a 6-month weight maintenance period. Br J Nutr 2009, 101:1846–1858. After a lead-in, 8-week low-energy diet and a 2- to 3-week refeeding period, 131 participants were randomized to three diets for 6 months: high MUFA–low glycemic index (35%–45% energy from fat); low fat (20%–30% of energy from fat), or control (35% of energy from fat). The two competing diets, high MUFA and low fat, showed equally beneficial outcomes with respect to glucose metabolism, whereas the control diet, resembling the typical Western diet, was associated with decreased insulin sensitivity.
Dale KS, McAuley KA, Taylor RW, et al.: Determining optimal approaches for weight maintenance: a randomized controlled trial. CMAJ 2009, 180:E39–E46.
• Shai I, Schwarzfuchs D, Henkin Y, et al.: Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med 2008, 359(3):229–241. (Published erratum appears in N Engl J Med 2009, 361:2681.). This 2-year trial randomly assigned 322 moderately patients (86% males) with an average age of 52 years and a BMI of 31 to one of three diets: low fat, restricted calorie; Mediterranean, restricted calorie; or low carbohydrate, nonrestricted calorie. Mediterranean and low-carbohydrate diets were suggested as effective alternatives to low-fat diets. The low-carbohydrate diet had more favorable effects on lipids whereas the Mediterranean diet had beneficial effects on glycemic control.
Brehm BJ, Lattin BL, Summer SS, et al.: One-year comparison of a high-monounsaturated fat diet with a high-carbohydrate diet in type 2 diabetes. Diabetes Care 2009, 32:215–220.
Esposito K, Maiorino MI, Ciotola M, et al.: Effects of a Mediterranean-style diet on the need for antihyperglycemic drug therapy in patients with newly diagnosed type 2 diabetes: a randomized trial. Ann Intern Med 2009, 151:306–314. (Published erratum appears in Ann Intern Med 2009, 151:591.)
Perez-Guisado J, Munoz-Serrano A, Alonso-Moraga A: Spanish Ketogenic Mediterranean Diet: a healthy cardiovascular diet for weight loss. Nutr J 2008, 7:30.
Romaguera D, Norat T, Mouw T, et al.: Adherence to the Mediterranean diet is associated with lower abdominal adiposity in European men and women. J Nutr 2009, 139:1728–1737.
Panagiotakos DB, Pitsavos C, Chrysohoou C, et al.: Five-year incidence of cardiovascular disease and its predictors in Greece: the ATTICA study. Vasc Med 2008, 13:113–121.
Sanchez-Tainta A, Estruch R, Bullo M, et al.: Adherence to a Mediterranean-type diet and reduced prevalence of clustered cardiovascular risk factors in a cohort of 3,204 high-risk patients. Eur J Cardiovasc Prev Rehabil 2008, 15:589–593.
St-Onge MP, Bosarge A: Weight-loss diet that includes consumption of medium-chain triacylglycerol oil leads to a greater rate of weight and fat mass loss than does olive oil. Am J Clin Nutr 2008, 87:621–626.
St-Onge MP, Bosarge A, Goree LL, Darnell B: Medium chain triglyceride oil consumption as part of a weight loss diet does not lead to an adverse metabolic profile when compared to olive oil. J Am Coll Nutr 2008, 27:547–552.
Kratz M, Swarbrick MM, Callahan HS, et al.: Effect of dietary n-3 polyunsaturated fatty acids on plasma total and high-molecular-weight adiponectin concentrations in overweight to moderately obese men and women. Am J Clin Nutr 2008, 87:347–353.
Harman NL, Leeds AR, Griffin BA: Increased dietary cholesterol does not increase plasma low density lipoprotein when accompanied by an energy-restricted diet and weight loss. Eur J Nutr 2008, 47:287–293. (Published erratum appears in Eur J Nutr, 47:408.)
Mutungi G, Ratliff J, Puglisi M, et al.: Dietary cholesterol from eggs increases plasma HDL cholesterol in overweight men consuming a carbohydrate-restricted diet. J Nutr 2008, 138:272–276.
Demol S, Yackobovitch-Gavan M, Shalitin S, et al.: Low-carbohydrate (low & high-fat) versus high-carbohydrate low-fat diets in the treatment of obesity in adolescents. Acta Paediatr 2009, 98:346–351.
Johnson L, Mander AP, Jones LR, et al.: Energy-dense, low-fiber, high-fat dietary pattern is associated with increased fatness in childhood. Am J Clin Nutr 2008, 87:846–854.
van Hees AM, Saris WH, Dallinga-Thie GM, et al.: Fasting and postprandial remnant-like particle cholesterol concentrations in obese participants are associated with plasma triglycerides, insulin resistance, and body fat distribution. J Nutr 2008, 138:2399–2405.
• Keogh JB, Brinkworth GD, Noakes M, et al.: Effects of weight loss from a very-low-carbohydrate diet on endothelial function and markers of cardiovascular disease risk in subjects with abdominal obesity. Am J Clin Nutr 2008, 87:567–576. With a recruitment of 99 participants and an average age of 50 years and a BMI of 33.7, this study examined endothelial function for two 8-week weight loss interventions. No difference was seen in the flow-mediated vasodilatation on the low-carbohydrate, high saturated fat diet compared with the high-carbohydrate diet. Weight loss was greater on the low-carbohydrate diet, but LDL-C, CRP, and homocysteine levels were significantly lower on the high-carbohydrate diet.
Phillips SA, Jurva JW, Syed AQ, et al.: Benefit of low-fat over low-carbohydrate diet on endothelial health in obesity. Hypertension 2008, 51:376–382.
Rallidis LS, Lekakis J, Kolomvotsou A, et al.: Close adherence to a Mediterranean diet improves endothelial function in subjects with abdominal obesity. Am J Clin Nutr 2009, 90:263–268.
Arefhosseini SR, Edwards CA, Malkova D, Higgins S: Effect of advice to increase carbohydrate and reduce fat intake on dietary profile and plasma lipid concentrations in healthy postmenopausal women. Ann Nutr Metab 2009, 54:138–144.
Martin LJ, Greenberg CV, Kriukov V, et al.: Intervention with a low-fat, high-carbohydrate diet does not influence the timing of menopause. Am J Clin Nutr 2006, 84:920–928.
Saquib N, Natarajan L, Rock CL, et al.: The impact of a long-term reduction in dietary energy density on body weight within a randomized diet trial. Nutr Cancer 2008, 60:31–38.
Tanumihardjo SA, Valentine AR, Zhang Z, et al.: Strategies to increase vegetable or reduce energy and fat intake induce weight loss in adults. Exp Biol Med (Maywood) 2009, 234:542–552.
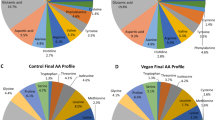
• Barnard ND, Cohen J, Jenkins DJ, et al.: A low-fat vegan diet and a conventional diabetes diet in the treatment of type 2 diabetes: a randomized, controlled, 74-wk clinical trial. Am J Clin Nutr 2009, 89:1588S–1596S. This study showed that consumption of a low-fat vegan diet for 74 weeks under free-living conditions was associated with serum lipid and body weight reduction in 49 type 2 diabetes patients. In an analysis, controlling for medication changes, the vegan diet better improved serum lipids and glycemic control compared with the conventional ADA diet (2003 ADA Diet).
Jenkins DJ, Wong JM, Kendall CW, et al.: The effect of a plant-based low-carbohydrate (“Eco-Atkins”) diet on body weight and blood lipid concentrations in hyperlipidemic subjects. Arch Intern Med 2009, 169:1046–1054. (Published erratum appears in Arch Intern Med 2009, 169:1490.)
Burke LE, Warziski M, Styn MA, et al.: A randomized clinical trial of a standard versus vegetarian diet for weight loss: the impact of treatment preference. Int J Obes (Lond) 2008, 32:166–176.
Grant R, Bilgin A, Zeuschner C, et al.: The relative impact of a vegetable-rich diet on key markers of health in a cohort of Australian adolescents. Asia Pac J Clin Nutr 2008, 17:107–115.
• Joshipura KJ, Hung HC, Li TY, et al.: Intakes of fruits, vegetables and carbohydrate and the risk of CVD. Public Health Nutr 2009, 12:115–121. The pooled analysis of the Nurses’ Health Study (n = 70,870) and the Health Professionals’ Follow-Up Study (n = 38,918) assessed the effect of different levels of carbohydrate intake and relation of fruit and vegetable intake to CVD risk. Among the group consuming low carbohydrate, intake of total and green leafy vegetables and carotene-rich fruits and vegetables showed stronger negative associations with CVD. No consistent trends were observed for fruit intake.
Craig WJ, Mangels AR: Position of the American Dietetic Association: vegetarian diets. J Am Diet Assoc 2009, 109:1266–1282.
Wolever TM, Gibbs AL, Mehling C, et al.: The Canadian Trial of Carbohydrates in Diabetes (CCD), a 1-y controlled trial of low-glycemic-index dietary carbohydrate in type 2 diabetes: no effect on glycated hemoglobin but reduction in C-reactive protein. Am J Clin Nutr 2008, 87:114–125.
Jenkins DJ, Kendall CW, McKeown-Eyssen G, et al.: Effect of a low-glycemic index or a high-cereal fiber diet on type 2 diabetes: a randomized trial. JAMA 2008, 300:2742–2753.
• Levitan EB, Cook NR, Stampfer MJ, et al.: Dietary glycemic index, dietary glycemic load, blood lipids, and C-reactive protein. Metabolism 2008, 57:437–443. This study evaluated fasting blood samples of 18,137 healthy women (no CVD, cancer, or diabetes) from The Women’s Health Study to demonstrate whether a relation existed between glycemic index or glycemic load and CHD risk factors. Comparison of top and bottom quintiles of glycemic index and glycemic load demonstrated a significant association with HDL-C, the ratio of LDL-C to HDL-C, and triglyceride, with glycemic index also relating to CRP.
Abete I, Parra D, Martinez JA: Energy-restricted diets based on a distinct food selection affecting the glycemic index induce different weight loss and oxidative response. Clin Nutr 2008, 27:545–551.
• Philippou E, McGowan BM, Brynes AE, et al.: The effect of a 12-week low glycaemic index diet on heart disease risk factors and 24 h glycaemic response in healthy middle-aged volunteers at risk of heart disease: a pilot study. Eur J Clin Nutr 2008, 62:145–149. This 12-week randomized, parallel pilot study involving 18 patients at risk of heart disease provided evidence that consuming a low glycemic index diet increased weight loss and reduced day long blood glucose. This study did not show a lipid-lowering advantage of either diet.
Ebbeling CB, Leidig MM, Sinclair KB, et al.: Effects of an ad libitum low-glycemic load diet on cardiovascular disease risk factors in obese young adults. Am J Clin Nutr 2005, 81:976–982.
Pereira MA, Swain J, Goldfine AB, et al.: Effects of a low-glycemic load diet on resting energy expenditure and heart disease risk factors during weight loss. JAMA 2004, 292:2482–2490.
Katcher HI, Legro RS, Kunselman AR, et al.: The effects of a whole grain-enriched hypocaloric diet on cardiovascular disease risk factors in men and women with metabolic syndrome. Am J Clin Nutr 2008, 87:79–90.
Salmeron J, Manson JE, Stampfer MJ, et al.: Dietary fiber, glycemic load, and risk of non-insulin-dependent diabetes mellitus in women. JAMA 1997, 277:472–477.
Liu S, Willett WC, Stampfer MJ, et al.: A prospective study of dietary glycemic load, carbohydrate intake, and risk of coronary heart disease in US women. Am J Clin Nutr 2000, 71:1455–1461.
Spieth LE, Harnish JD, Lenders CM, et al.: A low-glycemic index diet in the treatment of pediatric obesity. Arch Pediatr Adolesc Med 2000, 154:947–951.
Layman DK, Clifton P, Gannon MC, et al.: Protein in optimal health: heart disease and type 2 diabetes. Am J Clin Nutr 2008, 87:1571S–1575S.
Gannon MC, Nuttall FQ: Effect of a high-protein, low-carbohydrate diet on blood glucose control in people with type 2 diabetes. Diabetes 2004, 53:2375–2382.
Layman DK, Evans EM, Erickson D, et al.: A moderate-protein diet produces sustained weight loss and long-term changes in body composition and blood lipids in obese adults. J Nutr 2009, 139:514–521.
• Clifton PM, Keogh JB, Noakes M: Long-term effects of a high-protein weight-loss diet. Am J Clin Nutr 2008, 87:23–29. Seventy-nine healthy women with average age of 49 years and BMI of 32.8 were recruited for a 12-week weight loss and 52-week follow-up study. Weight loss was not different based on randomization to high-protein or low-protein diets. Ironically, protein intake assessed as the comparison of upper tertile versus lower 2 tertiles of reported protein intake showed a significant weight loss related to increased protein intake.
Arciero PJ, Gentile CL, Pressman R, et al: Moderate protein intake improves total and regional body composition and insulin sensitivity in overweight adults. Metabolism 2008, 57:757–765.
Appel LJ, Moore TJ, Obarzanek E, et al.: A clinical trial of the effects of dietary patterns on BP. DASH Collaborative Research Group. N Engl J Med 1997, 336:1117–1124.
Maruthur NM, Wang NY, Appel LJ: Lifestyle interventions reduce coronary heart disease risk: results from the PREMIER Trial. Circulation 2009, 119:2026–2031.
Nowson CA, Wattanapenpaiboon N, Pachett A: Low-sodium Dietary Approaches to Stop Hypertension-type diet including lean red meat lowers BP in postmenopausal women. Nutr Res 2009, 29:8–18.
• Forman JP, Stampfer MJ, Curhan GC: Diet and lifestyle risk factors associated with incident hypertension in women. JAMA 2009, 302:401–411. The Second Nurses’ Health Study, a prospective cohort, examined the development of hypertension in 83,882 women 27–44 years of age. The women, healthy at baseline, were followed up for 14 years (1991–2005) for self-reported occurrence of hypertension. BMI was the most powerful indicator of hypertension; those with BMI of 25 or greater were shown to have an adjusted population-attributable risk (PAR) of 40%. Adherence to low-risk dietary and lifestyle factors was associated with a significantly lower incidence of self-reported hypertension. Low-risk lifestyle factors were defined as 30 min of exercise daily, BMI less than 25, alcohol intake of 0.1–10 g/d, and non-narcotic analgesic use of less than 1 day per week. Low-risk dietary factors included using folic acid supplementation of ≥400 μg/d and scoring in the top quintile of DASH score. The DASH score was in turn based on how much participants increased servings of fruit, vegetables, and whole grain and decreased servings of sodium, red and processed meats, and sweetened beverages. Data on these dietary components were not given for the present study.
Sacks FM, Svetkey LP, Vollmer WM, et al.: Effects on BP of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 2001, 344:3–10.
Appel LJ, Sacks FM, Carey VJ, et al.: Effects of protein, monounsaturated fat, and carbohydrate intake on BP and serum lipids: results of the OmniHeart randomized trial. JAMA 2005, 294:2455–2464.
Jenkins DJ, Kendall CW, Faulkner DA, et al.: Long-term effects of a plant-based dietary portfolio of cholesterol-lowering foods on BP. Eur J Clin Nutr 2008, 62:781–788.
Griffith LE, Guyatt GH, Cook RJ, et al.: The influence of dietary and nondietary calcium supplementation on BP: an updated metaanalysis of randomized controlled trials. Am J Hypertens 1999, 12:84–92.
Resnick LM, Oparil S, Chait A, et al.: Factors affecting BP responses to diet: the Vanguard study. Am J Hypertens 2000, 13:956–965.
Jenkins DJ, Sievenpiper JL, Pauly D, et al.: Are dietary recommendations for the use of fish oils sustainable? CMAJ 2009, 180:633–637
Disclosure
Dr. Jenkins has served on the Scientific Advisory Board of Unilever, the Sanitarium Company, and the California Strawberry Commission and received research grants from Loblaws, Unilever, Barilla, and the Almond Board of California. Dr. Jenkins and Kendall have been on the speaker’s panel for the Almond Board of California. Dr. Jenkins has received honoraria for scientific advice from the Almond Board of California, Barilla, Unilever Canada, and Solae.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jenkins, D.J.A., Mirrahimi, A., Nguyen, T.H. et al. Macronutrients, Weight Control, and Cardiovascular Health: A Systematic Review. Curr Cardio Risk Rep 4, 89–100 (2010). https://doi.org/10.1007/s12170-010-0082-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12170-010-0082-z