Abstract
Lung cancer is the most common cancer globally and has the highest mortality. Although this disease is not associated with a particular gender, its incidence is rising among women, who are diagnosed at an increasingly younger age compared with men. One of the main reasons for this rise is women taking up smoking. However, many non-smoking women also develop this disease. Other risk factors implicated in the differential development of lung cancer in women are genetic predisposition, tumour histology and molecular profile. Proportionally more women than men with lung cancer have a mutation in the EGFR gene. This consensus statement reviews the available evidence about the epidemiological, biological, diagnostic, therapeutic, social and psychological aspects of lung cancer in women.
Similar content being viewed by others
Introduction
Lung cancer is the most common cancer globally, and has the highest mortality [1]. However, whereas its mortality is falling in men, in women it is increasing exponentially [2, 3], probably as a consequence of recent changes in gender-specific smoking patterns [4]. The biological basis, natural history and prognosis of lung cancer in women are not the same as in men. However, the reasons behind these differences are not yet fully understood [5].
The Association for Lung Cancer Research in Women (ICAPEM) was set up in 2010, in response to the increasing incidence of this disease in women. Its aims are to promote knowledge, research, prevention and social awareness of this health issue. In order to perform a detailed analysis of the gender perspective in lung cancer, ICAPEM invited a number of experts in this disease to a meeting, the end result of which is the first consensus statement on this subject.
This document addresses the available evidence about the epidemiological, biological, psychological, diagnostic and therapeutic aspects of this disease. Social issues, smoking habits and patients’ own views are also considered. This multidisciplinary discussion has shown that lung cancer certainly needs to be addressed and researched in more depth, to determine whether or not different approaches to this disease are required according to gender.
Lung cancer epidemiology and risk factors
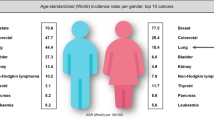
According to World Health Organisation (WHO) estimates, the incidence of cancer in 2012 was 14.1 million new cases, with 8.2 million deaths worldwide [6]. Lung cancer was the most common, in terms of both the number of new cases (1.8 million; 12.9% of the total) and the mortality rate (1.6 million deaths; 19.4% of the total). Worldwide, lung cancer is still the most common disease in men (1.2 million; 16.7% of the total). Although its incidence in women is low, there are large geographical variations depending on the number of women who have taken up smoking. Even so, a progressive rise in the incidence of this disease is apparent in all regions [2]. This fact, combined with its high mortality, constitutes the so-called “lung cancer epidemic in women” [7].
In Spain, the estimated overall cancer incidence in 2012 was 215,534 new cases, of whom 128,550 (59.64%) were male and 86,984 (40.35%) female. Of all cancers, lung cancer has the second highest incidence rate in males (16.94%) and the fourth highest in females (5.67%; 4935 new cases) [8]. In terms of mortality, it is also responsible for the greatest number of cancer deaths (20.55%; 21,118 of the total): 27.41% in males (17,430 deaths) compared with 9.41% in females (3688 deaths) (Table 1). This high mortality rate means that the 5-year prevalence of lung cancer is minimal (4.8% overall; 28,148 of the total), being slightly higher in males and only 2.1% in females.
In Spain, the incidence of lung cancer in women is among the lowest in the world, although, since the early 1990s, it is one of the countries that has seen the greatest increase [9]. This is probably because tobacco use by Spanish women started late and peaked between 1960 and 1990, tending to stabilise from the year 2000 onwards [10]. During this period, the incidence of lung cancer in the female population rose by 4.2% each year [11]. Tobacco use is, thus, the most important risk factor for the development of lung cancer, being directly responsible for 80–90% of cases and indirectly responsible because of passive smoking [12]. In fact, women are the most vulnerable to tobacco carcinogens, which means they have a higher risk than men of developing lung cancer [13].
Other known risk factors are industrial pollution, occupational exposure (asbestos, arsenic, chromium, cadmium, polycyclic aromatic hydrocarbons), exposure to radon gas in dwellings and mines, and exposure to ionising radiation. Exposure to these factors varies greatly between individuals and populations, creating a geographical pattern that also differs according to gender. The areas with the highest mortality rates are the northern area of La Coruña and Lugo regions, some towns in Pontevedra, Orense, the Malaga coast, Girona, Asturias, the Canary Islands and Madrid. The higher lung cancer mortality rate in these areas might also be linked to exposure to environmental factors, such as radon and industrial pollution, and not just to smoking [14].
Although genetic influences on lung cancer are not yet clearly defined, the presence of a first-degree relative affected by lung cancer almost doubles the risk of developing the disease, and this risk is higher in female descendants [5]. Also, molecular mechanisms associated with lung cancer susceptibility have been detected in women. Female genotypes contain higher levels of reactive metabolites and DNA adducts than are found in the male population, which might explain why women are more susceptible to molecular aberrations caused by tobacco smoke [15]. Another matter of debate is whether oestrogen affects the risk of lung cancer. Information concerning the influence of hormone therapy on lung cancer risk is also controversial [16].
Biological aspects implicated
There is some evidence to suggest greater susceptibility to tobacco carcinogens in women than in men, irrespective of their smoking habits. Lung carcinomas that arise in women have significantly more tobacco-related mutations (G → T transversions in the TP53 or KRAS genes), despite women being diagnosed at a younger age and smoking fewer packs a year than men [17,18,19,20,21]. An attractive hypothesis therefore postulates that targetable oncogenes should be highly prevalent in female lung cancers, because many of these oncogenes have classically been associated with light smoking.
Analysis of several recent studies from both the USA and Europe shows that female gender is, on the whole, more often associated with a genotype that permits personalised therapy, especially among primary adenocarcinomas of the lung [22,23,24]. A trend is apparent in these global studies for mutations in the epidermal growth factor receptor gene (EGFR), but less obviously for ALK, ROS1 and RETS translocations or mutations in HER2 [22,23,24]. This is partly because the systematic study of some of these genes is very recent, and not all studies include them or test for them by methods that are sufficiently sensitive and specific. Data from studies addressing a single gene are discussed below. To avoid the conclusions being biased by the greater presence of Asian patients in studies from the USA, we focus mainly on European studies.
In the case of ALK translocation, two Spanish articles reported finding this alteration in roughly 60–90% of women [25, 26]. Another French study, involving the screening of over 3,000 patients, documented a more than twofold relative risk for this molecular event in women [27]. Analysis of the literature on ROS1 translocation is interesting. A multicentre study involving one of the largest series of patients with lung adenocarcinoma only documented 19 cases positive for this translocation, with no differences by gender [28]. These results are in contrast to the clear preponderance for women with ROS1-positive lung carcinoma in two other European studies, including a Spanish study in which the percentage was 80% [29, 30]. As regards RET translocation, this seems more common in males, and the smoking context is not so clear [31]. A review of HER2 mutation data yields very similar results: between 62 and 69% of HER2-mutated lung carcinomas were detected in women [32, 33].
All this evidence points to the need for thorough molecular investigation of lung adenocarcinomas in women. Recently published genome data for these cancers further reinforces the idea that therapeutic targets in lung adenocarcinomas are almost always mutually exclusive [34], that is, for every negative predictive biomarker result obtained in these patients, the likelihood of finding a targeted treatment might increase.
Social and psychological aspects
There are differences in the way tobacco use affects males and females. One of the most important is weight gain; in general, women worry more than men about gaining weight and tobacco can help them control it. Also, women gain more weight than men when they stop smoking. Women also smoke to protect themselves or manage negative feelings, whereas men tend to smoke to enhance pleasurable sensations. Lastly, some women smoke to switch off from the demands of running a household.
How adjustment to cancer is influenced by gender is not clearly defined. Gender differences are evident in the physical impact of cancer, quality of life, coping styles and partners’ adjustment to the disease. In general, it seems it may be easier for women to adjust favourably to cancer than for men because they have larger social support systems [35].
Lung cancer in smokers tends to be associated with feelings of guilt and shame. It is experienced as a self-inflicted disease because of its link to smoking, and it leads to social isolation [36, 37]. Also, lung cancer patients have more feelings of guilt, shame, anxiety and depression than patients with other types of cancer [38].
Despite lung cancer now being the leading cause of cancer death in women worldwide, little information is available for evaluating female patients’ quality of life. Most female patients experience severe disruption to their psychological and social wellbeing. Also, they see the disease as a complex challenge to be faced. Women with lung cancer have been reported to experience more mood disorders than men [39]. However, results are contradictory on this issue. Increased rates of depression in women with lung cancer have been found when compared to men, only when performance status (PS) is good, but gender difference is reduced for poor PS patients because of increased depression rates for men [40]. Women with lung cancer have higher levels of anxiety and concerns following diagnosis [41].
Quality of life data in women with lung cancer, however, yield better scores than in men at all stages of the disease [42]. Nevertheless, women are subject to a number of limitations that affect their quality of life more than men, such as difficulty performing domestic chores, caring for children, or other demands associated with their role. This is especially apparent in young women with recurrent disease or low socio-economic status [43]. Another important piece of information to bear in mind is that long-term lung cancer survivors suffer significant symptoms for a long time after the end of treatment, and these have an adverse impact on their quality of life [44].
Family is essential for maintaining and improving cancer patients’ quality of life [45]. Although a diagnosis of cancer has a significant impact on the family’s quality of life, the impact of lung cancer on family quality of life is variable and unrelated to the patient’s quality of life or physical condition [46]. If a relative has health problems, his or her quality of life will be reduced, and he or she will also be less able to care for a cancer patient, and may experience more stress than the cancer survivor [47, 48].
Little information is available about the needs of female lung cancer patients and their relatives, and the resources they use. To learn more about this, ICAPEM set up the CIRCULOS study in 2015, focusing on women with lung cancer and their family environment in the Autonomous Region of Galicia (Spain). One thing seen in the study is a demand for greater emotional and social support, not just by patients, but also by families and carers, to be able to care for patients better. The overall study results will be published shortly.
Diagnosis and gender differences
At the time of lung cancer diagnosis, there are differences in some characteristics between men and women, notably age, tumour histology, smoking habits and mutations in the EGFR gene.
It seems that women with lung cancer are younger than men at the time of diagnosis. In the WORLD07 study, which recorded characteristics from 2,060 women diagnosed with lung cancer, the median age of women diagnosed with this cancer was 61 years [49]. In this same study, median age was 59 years for patients with a wild-type EGFR gene and 66 years for EGFR-mutated patients.
The distribution of histological types differs somewhat between men and women. In women, the most common histological subtype is adenocarcinoma. In the WORLD07 study, 86% of patients were diagnosed with NSCLC and 14% had small-cell carcinoma. Among patients diagnosed with non-small-cell carcinoma, 75% had adenocarcinoma, 11% squamous cell carcinoma, and 7% large-cell carcinoma [49].
Although the increased incidence of female lung cancer is clearly related to women taking up smoking, a substantial percentage of women with lung cancer are non-smokers. In the WORLD07 study, 39% of women diagnosed with lung cancer included in the database were non-smokers [49].
Mutations in the EGFR gene are seen in 10–16% of lung cancer patients in the Caucasian population. EGFR mutations are more common in adenocarcinoma histology, non-smokers, Asian population and women [50]. In a study examining the molecular profile of lung cancer patients in France, 11% of patients had a mutated EGFR gene, but when women were analysed, the percentage of patients with an EGFR mutation rose to 21% [23]. In a meta-analysis looking at patients with EGFR mutations treated with first-line EGFR inhibitors, female gender and not smoking were predictors of a better outcome [51]. In a study by the Spanish Lung Cancer Group (SLCG), longer progression-free survival was also seen in women with EGFR mutations treated with erlotinib compared with men [52].
Treatment and gender perspective
In numerous large studies, women with lung cancer were diagnosed at younger ages than men, and women, compared with their male counterparts, were more likely to be lifetime nonsmokers, smoked fewer years and consumed fewer cigarettes per day, suggesting different tobacco susceptibility [5]. All of these lung cancer clinicopathological characteristics in women should be borne in mind when implementing lung cancer screening programmes and women should be screened younger and with a lower pack/year cut-off point. Also, 25% of lung cancers occur in never-smokers: lung cancer in never-smokers is the seventh cause of cancer-related death worldwide with a truncated age-adjusted incidence higher among women compared with men [5]. However, based on National Lung Cancer Screening Trial cohort, currently, never-smokers should not be screened [53].
Surgery
The surveillance, epidemiology, and end results programme (SEER) database currently shows that 16% of NSCLC are diagnosed at localised stage [54], where surgery remains the standard treatment for fit patients and platinum-based adjuvant chemotherapy is recommended for stage II-IIIA patients. Nowadays, it is unclear whether less invasive surgical procedures in early stages may be optimal. Two randomised phase III trials (CALGB 140503 and JCOG0802) are trying to validate sub-lobar resection as a surgical procedure in stage IA lung cancer patients compared with lobectomy (ClinTrials.gov NCT00499330) [55].
It is not known whether gender has any influence in surgical procedure and in post-surgical complications. A prospective Spanish trial investigated clinical characteristics and post-surgical complications according to gender in a cohort of 3,307 resected NSCLC patients [56]. Similar to previous clinical series, women (n = 741, 22.4% of the total cohort) were diagnosed younger than men (62 years vs. 66 years; p < 0.05); adenocarcinoma was more common in females than males (70.4 vs. 46.2; p < 0.001); the proportions of never-smokers were higher among females (35% vs. 5.3%; p < 0.001); and among smoking patients, women smoked fewer packs/year than men (36.6 vs. 52.9; p < 0.001). This lower smoking history among women corresponds with their lower comorbidities reported in this study (p < 0.05). All these factors rather than gender might justify the significantly lower number of pneumonectomy interventions, post-surgical complications and mortality among women compared with men.
Chemotherapy
Approximately 60% of NSCLC are diagnosed with advanced disease [54]. Platinum-based doublet chemotherapy is the standard first-line treatment for non-selected patients with advanced NSCLC who have a good PS. A French study reported that gender is a prognostic factor. One-year survival is 41.9% for women and 38.8% for men [57]. Moreover, in locally advanced and metastatic stages, women live longer than men especially with platinum-base schedules [58, 59]. However, no survival differences according to gender occurred with new agents such as pemetrexed and bevacizumab [60, 61]. Women experienced more gastrointestinal and neuropathy treatment toxicity. It is postulated that decreased DNA repair capacity in women might be responsible for the increased response rate and toxicity with platinum agents [5]. Therefore, gender should be the first thing to bear in mind for personalised treatment among lung cancer patients.
Targeted therapies
Personalised treatment based on the recognition of oncogenic driver mutations has changed the treatment paradigm of lung cancer patients, especially among the adenocarcinoma subtype. Approximately 50% of advanced NSCLC have a genetic alteration but only 20–25% of them are actionable oncogenic driver mutations [23].
To date, nine randomised phase III trials have established EGFR tyrosine kinase inhibitors (TKI) as standard first-line treatment in EGFR mutant NSCLC [62]. A recent meta-analysis has reported lack of association between the type of EGFR mutation and gender (p = 0.81). EGFR TKI treatment demonstrated a 27% greater benefit in women than in men in terms of progression-free survival compared with chemotherapy (p = 0.02). The predictive effect of gender was independent of smoking status and EGFR mutation type [63].
EML4-ALK rearrangements occurred in ~5% of NSCLC patients, and it is more frequent in never/light smokers, adenocarcinoma subtype and young patients. Compared with female NSCLC patients, the odds ratio of carrying ALK rearrangements was reduced by 28% in males, especially among Asian patients [64]. However, opposite results have been reported among European populations [65]. In randomised phase III trials with crizotinib, higher numbers of females have been included with a trend toward differences in the efficacy of crizotinib according to gender-subgroup analysis [66, 67].
BRAF mutations have been described in 2-4% of lung cancers, especially adenocarcinoma without ethnicity, smoking pattern or gender predominance [68, 69]. These clinicopathological characteristics have been also reported in a European cohort [70]. The V600E mutation accounts for 50% of cases, more frequent in women, and it is a negative prognostic factor [69]. In a phase II trial, the BRAF inhibitor dabrafenib in combination with the MEK1 inhibitor trametinib showed a response rate of 63%. In this trial, a high number of females were included, but outcome according to gender is not reported [68].
ROS1 rearrangements have been detected in 1.5% of patients, usually young (~50 years), never-smokers and patients with adenocarcinoma subtype, and female predominance. Crizotinib showed marked antitumor activity in this subgroup of lung cancer patients. In the European cohort, a higher number of females had ROS1 rearrangements than males [71].
In a retrospective study, HER2 mutations occurred in 65 (1.7%) of 3800 patients with lung adenocarcinoma, mainly female and never-smokers [33]. In another study, HER2 mutations represented 6% of cases but were not gender-related [32]. In a retrospective European cohort, HER2 mutations were more common in females (62.4%) and HER2-targeted agents demonstrated their potential activity in these patients [33].
RET rearrangements occur in 1–2% of NSCLC patients, mainly in never-smokers and men [31]. Oncogenic MET mutations in exon 14 occur in 4% of lung adenocarcinomas, especially in women of older age (~75 years). This mutation confers clinical sensitivity to MET inhibitors such as crizotinib and cabozantinib [72].
Nowadays, the limited number of patients included in some of these databases does not allow conclusions to be drawn about gender predominance in some of these molecular alterations or whether smoking pattern might be a confounding factor in the interaction between gender and the molecular profile. Moreover, it is important to evaluate whether the toxicity profile of these TKIs are different according to gender.
Immunotherapy
Immunotherapy is a second-line option in advanced NSCLC. PD-L1 expression has been reported as a putative predictive marker and its expression is higher in tumours in women than in men [73]. However, there is no a clear relationship between gender and immunotherapy efficacy, which could be influenced by smoking pattern [74].
Cancer therapy toxicity and fertility
It is known that the side effects of treatments, and responses to them, can differ between men and women. For example, chemotherapy treatments can produce higher rates of vomiting and haematological toxicity in women than in men. Conversely, males have a higher incidence of lower gastrointestinal tract toxicity, related to lower expression and activity of glutathione S-transferase in the gut [75].
In the last few years, various sociological factors have led to a delay in the age at which women embark on motherhood. Because cancer is increasingly diagnosed at a younger age (an estimated 2% of lung cancer cases occur in women under 40 years old) the wish to start a family is jeopardised, as the cancer treatments indicated may compromise fertility [76, 77]. To date, specific clinical guidelines on fertility are only available for breast cancer and lymphomas. A young woman diagnosed with cancer must always be informed about the long-term repercussions treatment may have on fertility.
Chemotherapy may affect ovarian reserve to differing degrees depending on the type of drug (Table 2) [78]. Radiotherapy also entails a risk to fertility, depending on the dose and the area to which it is administered. The risk is higher when the abdomen, pelvis or central nervous system (hypothalamic-pituitary axis) is irradiated.
Therefore, when cancer is diagnosed in women of childbearing age, it is important to offer them comprehensive information about their life expectancy and the risks and benefits of indicated treatments, taking account of whether the patient has already completed her family (Fig. 1) [79, 80].
Conclusions
The significant increase in smoking in the female population has produced a dramatic rise in lung cancer incidence and mortality.
Various lines of evidence suggest that this disease behaves differently in women, with a higher percentage of adenocarcinoma or EGFR mutations, and no history of smoking in 30% of cases. There has also been speculation about greater female susceptibility to possible carcinogens implicated in the development of this cancer, or greater toxicity experienced with chemotherapy. Moreover, the potential impact on quality of life, fertility or emotional repercussions for female patients and their families is unknown.
For all these reasons, studies designed specifically for women are a high priority, to provide greater understanding of the biology and course of lung cancer, and to develop support programmes to improve treatment (Table 3).
References
Allemani C, Weir HK, Carreira H, Harewood R, Spika D, Wang XS, et al. Global surveillance of cancer survival 1995–2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2). Lancet. 2015;385:977–1010.
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–86.
Malvezzi M, Bertuccio P, Rosso T, Rota M, Levi F, La Vecchia C, et al. European cancer mortality predictions for the year 2015: does lung cancer have the highest death rate in EU women? Ann Oncol. 2015;26:779–86.
Encuesta Nacional de Salud de España 2011/12. http://www.msssi.gob.es/estadEstudios/estadisticas/encuestaNacional/encuesta2011.htm. Accessed May 2016.
Remon J, Molina-Montes E, Majem M, Lianes P, Isla D, Garrido P, et al. Lung cancer in women: an overview with special focus on Spanish women. Clin Transl Oncol. 2014;16:517–28.
GLOBOCAN 2012: Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012. http://globocan.iarc.fr/Default.aspx. Accessed May 2016.
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29.
Las Cifras del Cáncer en España 2016. Sociedad Española de Oncología Médica http://www.seom.org/es/prensa/el-cancer-en-espanyacom/105460-el-cancer-en-espana-2016. Accessed May 2016.
Cleries R, Buxo M, Martinez JM, Espinas JA, Dyba T, Borras JM. Contribution of changes in demography and in the risk factors to the predicted pattern of cancer mortality among Spanish women by 2022. Cancer Epidemiol. 2016;40:113–8.
Schiaffino A, Fernandez E, Borrell C, Salto E, Garcia M, Borras JM. Gender and educational differences in smoking initiation rates in Spain from 1948 to 1992. Eur J Pub Health. 2003;13:56–60.
Linares I, Molina-Portillo E, Exposito J, Baeyens JA, Suarez C, Sanchez MJ. Trends in lung cancer incidence by histologic subtype in the south of Spain, 1985–2012: a population-based study. Clin Transl Oncol. 2016;18:489–96.
Lopez MJ, Perez-Rios M, Schiaffino A, Fernandez E. Mortality attributable to secondhand smoke exposure in Spain (2011). Nicotine Tob Res. 2016;18:1307–10.
Kreuzer M, Boffetta P, Whitley E, Ahrens W, Gaborieau V, Heinrich J, et al. Gender differences in lung cancer risk by smoking: a multicentre case-control study in Germany and Italy. Br J Cancer. 2000;82:227–33.
Galcerán J, Ameijide A, Carulla M, Mateos A, Quirós JR, Alemán A et al. Estimaciones de la incidencia y la supervivencia del cáncer en España y su situación en Europa. Red Española de Registros de Cáncer (REDECAN) 2014.
Freedman ND, Leitzmann MF, Hollenbeck AR, Schatzkin A, Abnet CC. Cigarette smoking and subsequent risk of lung cancer in men and women: analysis of a prospective cohort study. Lancet Oncol. 2008;9:649–56.
Rouquette I, Lauwers-Cances V, Allera C, Brouchet L, Milia J, Nicaise Y, et al. Characteristics of lung cancer in women: importance of hormonal and growth factors. Lung Cancer. 2012;76:280–5.
Kiyohara C, Ohno Y. Sex differences in lung cancer susceptibility: a review. Gend Med. 2010;7:381–401.
Pesatori AC, Carugno M, Consonni D, Caporaso NE, Wacholder S, Tucker M, et al. Reproductive and hormonal factors and the risk of lung cancer: the EAGLE study. Int J Cancer. 2013;132:2630–9.
Zang EA, Wynder EL. Differences in lung cancer risk between men and women: examination of the evidence. J Natl Cancer Inst. 1996;88:183–92.
Marrogi AJ, Mechanic LE, Welsh JA, Bowman ED, Khan MA, Enewold L, et al. TP53 mutation spectrum in lung cancer is not different in women and men. Cancer Epidemiol Biomarkers Prev. 2005;14:1031–3.
Dogan S, Shen R, Ang DC, Johnson ML, D’Angelo SP, Paik PK, et al. Molecular epidemiology of EGFR and KRAS mutations in 3,026 lung adenocarcinomas: higher susceptibility of women to smoking-related KRAS-mutant cancers. Clin Cancer Res. 2012;18:6169–77.
Sholl LM, Aisner DL, Varella-Garcia M, Berry LD, Dias-Santagata D, Wistuba II, et al. Multi-institutional oncogenic driver mutation analysis in lung adenocarcinoma: the lung cancer mutation consortium experience. J Thorac Oncol. 2015;10:768–77.
Barlesi F, Mazieres J, Merlio JP, Debieuvre D, Mosser J, Lena H, et al. Routine molecular profiling of patients with advanced non-small-cell lung cancer: results of a 1-year nationwide programme of the French Cooperative Thoracic Intergroup (IFCT). Lancet. 2016;387:1415–26.
Sacher AG, Dahlberg SE, Heng J, Mach S, Janne PA, Oxnard GR. Association between younger age and targetable genomic alterations and prognosis in non-small-cell lung cancer. JAMA Oncol. 2016;2:313–20.
Conde E, Angulo B, Izquierdo E, Munoz L, Suarez-Gauthier A, Plaza C, et al. The ALK translocation in advanced non-small-cell lung carcinomas: preapproval testing experience at a single cancer centre. Histopathology. 2013;62:609–16.
Martinez P, Hernandez-Losa J, Montero MA, Cedres S, Castellvi J, Martinez-Marti A, et al. Fluorescence in situ hybridization and immunohistochemistry as diagnostic methods for ALK positive non-small cell lung cancer patients. PLoS ONE. 2013;8:e52261.
Cabillic F, Gros A, Dugay F, Begueret H, Mesturoux L, Chiforeanu DC, et al. Parallel FISH and immunohistochemical studies of ALK status in 3244 non-small-cell lung cancers reveal major discordances. J Thorac Oncol. 2014;9:295–306.
Scheffler M, Schultheis A, Teixido C, Michels S, Morales-Espinosa D, Viteri S, et al. ROS1 rearrangements in lung adenocarcinoma: prognostic impact, therapeutic options and genetic variability. Oncotarget. 2015;6:10577–85.
Clave S, Gimeno J, Munoz-Marmol AM, Vidal J, Reguart N, Carcereny E, et al. ROS1 copy number alterations are frequent in non-small cell lung cancer. Oncotarget. 2016;7:8019–28.
Warth A, Muley T, Dienemann H, Goeppert B, Stenzinger A, Schnabel PA, et al. ROS1 expression and translocations in non-small-cell lung cancer: clinicopathological analysis of 1478 cases. Histopathology. 2014;65:187–94.
Michels S, Scheel AH, Scheffler M, Schultheis AM, Gautschi O, Aebersold F, et al. Clinicopathological characteristics of RET rearranged lung cancer in european patients. J Thorac Oncol. 2016;11:122–7.
Arcila ME, Chaft JE, Nafa K, Roy-Chowdhuri S, Lau C, Zaidinski M, et al. Prevalence, clinicopathologic associations, and molecular spectrum of ERBB2 (HER2) tyrosine kinase mutations in lung adenocarcinomas. Clin Cancer Res. 2012;18:4910–8.
Mazieres J, Barlesi F, Filleron T, Besse B, Monnet I, Beau-Faller M, et al. Lung cancer patients with HER2 mutations treated with chemotherapy and HER2-targeted drugs: results from the European EUHER2 cohort. Ann Oncol. 2016;27:281–6.
Campbell JD, Alexandrov A, Kim J, Wala J, Berger AH, Pedamallu CS et al. Distinct patterns of somatic genome alterations in lung adenocarcinomas and squamous cell carcinomas. Nat Genet. 2016:[Epub ahead of print].
Volkers N. In coping with cancer, gender matters. J Natl Cancer Inst. 1999;91:1712–4.
Sriram N, Mills J, Lang E, Dickson HK, Hamann HA, Nosek BA, et al. Attitudes and stereotypes in lung cancer versus breast cancer. PLoS ONE. 2015;10:e0145715.
Cataldo JK, Brodsky JL. Lung cancer stigma, anxiety, depression and symptom severity. Oncology. 2013;85:33–40.
LoConte NK, Else-Quest NM, Eickhoff J, Hyde J, Schiller JH. Assessment of guilt and shame in patients with non-small-cell lung cancer compared with patients with breast and prostate cancer. Clin Lung Cancer. 2008;9:171–8.
Cella DF, Orofiamma B, Holland JC, Silberfarb PM, Tross S, Feldstein M, et al. The relationship of psychological distress, extent of disease, and performance status in patients with lung cancer. Cancer. 1987;60:1661–7.
Hopwood P, Stephens RJ. Depression in patients with lung cancer: prevalence and risk factors derived from quality-of-life data. J Clin Oncol. 2000;18:893–903.
Hill KM, Amir Z, Muers MF, Connolly CK, Round CE. Do newly diagnosed lung cancer patients feel their concerns are being met? Eur J Cancer Care (Engl). 2003;12:35–45.
Svobodnik A, Yang P, Novotny PJ, Bass E, Garces YI, Jett JR, et al. Quality of life in 650 lung cancer survivors 6 months to 4 years after diagnosis. Mayo Clin Proc. 2004;79:1024–30.
Sarna L, Brown JK, Cooley ME, Williams RD, Chernecky C, Padilla G, et al. Quality of life and meaning of illness of women with lung cancer. Oncol Nurs Forum. 2005;32:E9–19.
Brown JK, Cooley ME, Chernecky C, Sarna L. A symptom cluster and sentinel symptom experienced by women with lung cancer. Oncol Nurs Forum. 2011;38:E425–35.
Badr H, Smith CB, Goldstein NE, Gomez JE, Redd WH. Dyadic psychosocial intervention for advanced lung cancer patients and their family caregivers: results of a randomized pilot trial. Cancer. 2015;121:150–8.
Ferrell BR, Virani R, Grant M. Analysis of symptom assessment and management content in nursing textbooks. J Palliat Med. 1999;2:161–72.
Sarna L, Cooley ME, Brown JK, Williams RD, Chernecky C, Padilla G, et al. Quality of life and health status of dyads of women with lung cancer and family members. Oncol Nurs Forum. 2006;33:1109–16.
Hagedoorn M, Buunk BP, Kuijer RG, Wobbes T, Sanderman R. Couples dealing with cancer: role and gender differences regarding psychological distress and quality of life. Psychooncology. 2000;9:232–42.
Vinolas N, Magem M, Garrido P, Artal A, de Castro J, Campelo RG et al. Lung cancer in women: The Spanish female-specific database WORLD 07. J Clin Oncol. 2009;27:15 s (Abstract 8084).
Wakelee HA, Chang ET, Gomez SL, Keegan TH, Feskanich D, Clarke CA, et al. Lung cancer incidence in never smokers. J Clin Oncol. 2007;25:472–8.
Bria E, Milella M, Cuppone F, Novello S, Ceribelli A, Vaccaro V, et al. Outcome of advanced NSCLC patients harboring sensitizing EGFR mutations randomized to EGFR tyrosine kinase inhibitors or chemotherapy as first-line treatment: a meta-analysis. Ann Oncol. 2011;22:2277–85.
Rosell R, Moran T, Queralt C, Porta R, Cardenal F, Camps C, et al. Screening for epidermal growth factor receptor mutations in lung cancer. N Engl J Med. 2009;361:958–67.
Tammemagi MC, Church TR, Hocking WG, Silvestri GA, Kvale PA, Riley TL, et al. Evaluation of the lung cancer risks at which to screen ever- and never-smokers: screening rules applied to the PLCO and NLST cohorts. PLoS Med. 2014;11:e1001764.
Surveillance, Epidemiology, and End Results Program (SEER) Stat Fact Sheets: Lung and Bronchus Cancer. http://seer.cancer.gov/statfacts/html/lungb.html. Accessed May 2016.
Nakamura K, Saji H, Nakajima R, Okada M, Asamura H, Shibata T, et al. A phase III randomized trial of lobectomy versus limited resection for small-sized peripheral non-small cell lung cancer (JCOG0802/WJOG4607L). Jpn J Clin Oncol. 2010;40:271–4.
Cueto A, Quero F, Bayarri CI, Izquierdo C, Izquierdo JM, Fibla JJ et al., editors. Características diferenciales de la cirugía del carcinoma broncogénico en la mujer y sus complicaciones postoperatorias. 7 Congreso de la Sociedad Espaola de Ciruga Torcica; 2016; Valencia, Spain.
Debieuvre D, Oster JP, Riou R, Berruchon J, Levy A, Mathieu JP, et al. The new face of non-small-cell lung cancer in men: results of two French prospective epidemiological studies conducted 10 years apart. Lung Cancer. 2016;91:1–6.
Albain KS, Rusch VW, Crowley JJ, Rice TW, Turrisi AT 3rd, Weick JK, et al. Concurrent cisplatin/etoposide plus chest radiotherapy followed by surgery for stages IIIA (N2) and IIIB non-small-cell lung cancer: mature results of Southwest Oncology Group phase II study 8805. J Clin Oncol. 1995;13:1880–92.
Wakelee HA, Wang W, Schiller JH, Langer CJ, Sandler AB, Belani CP, et al. Survival differences by sex for patients with advanced non-small cell lung cancer on Eastern Cooperative Oncology Group trial 1594. J Thorac Oncol. 2006;1:441–6.
Scagliotti GV, Parikh P, von Pawel J, Biesma B, Vansteenkiste J, Manegold C, et al. Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naive patients with advanced-stage non-small-cell lung cancer. J Clin Oncol. 2008;26:3543–51.
Soria JC, Mauguen A, Reck M, Sandler AB, Saijo N, Johnson DH, et al. Systematic review and meta-analysis of randomised, phase II/III trials adding bevacizumab to platinum-based chemotherapy as first-line treatment in patients with advanced non-small-cell lung cancer. Ann Oncol. 2013;24:20–30.
Reguart N, Remon J. Common EGFR-mutated subgroups (Del19/L858R) in advanced non-small-cell lung cancer: chasing better outcomes with tyrosine kinase inhibitors. Future Oncol. 2015;11:1245–57.
Lee CK, Wu YL, Ding PN, Lord SJ, Inoue A, Zhou C, et al. Impact of specific epidermal growth factor receptor (EGFR) mutations and clinical characteristics on outcomes after treatment with EGFR tyrosine kinase inhibitors versus chemotherapy in egfr-mutant lung cancer: a meta-analysis. J Clin Oncol. 2015;33:1958–65.
Fan L, Feng Y, Wan H, Shi G, Niu W. Clinicopathological and demographical characteristics of non-small cell lung cancer patients with ALK rearrangements: a systematic review and meta-analysis. PLoS ONE. 2014;9:e100866.
Fallet V, Cadranel J, Doubre H, Toper C, Monnet I, Chinet T, et al. Prospective screening for ALK: clinical features and outcome according to ALK status. Eur J Cancer. 2014;50:1239–46.
Shaw AT, Kim DW, Nakagawa K, Seto T, Crino L, Ahn MJ, et al. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N Engl J Med. 2013;368:2385–94.
Solomon BJ, Mok T, Kim DW, Wu YL, Nakagawa K, Mekhail T, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med. 2014;371:2167–77.
Nguyen-Ngoc T, Bouchaab H, Adjei AA, Peters S. BRAF alterations as therapeutic targets in non-small-cell lung cancer. J Thorac Oncol. 2015;10:1396–403.
Chen D, Zhang LQ, Huang JF, Liu K, Chuai ZR, Yang Z, et al. BRAF mutations in patients with non-small cell lung cancer: a systematic review and meta-analysis. PLoS ONE. 2014;9:e101354.
Gautschi O, Milia J, Cabarrou B, Bluthgen MV, Besse B, Smit EF, et al. Targeted therapy for patients with BRAF-mutant lung cancer: results from the European EURAF cohort. J Thorac Oncol. 2015;10:1451–7.
Mazieres J, Zalcman G, Crino L, Biondani P, Barlesi F, Filleron T, et al. Crizotinib therapy for advanced lung adenocarcinoma and a ROS1 rearrangement: results from the EUROS1 cohort. J Clin Oncol. 2015;33:992–9.
Awad MM, Oxnard GR, Jackman DM, Savukoski DO, Hall D, Shivdasani P, et al. MET Exon 14 mutations in non-small-cell lung cancer are associated with advanced age and stage-dependent MET genomic amplification and c-Met overexpression. J Clin Oncol. 2016;34:721–30.
Ota K, Azuma K, Kawahara A, Hattori S, Iwama E, Tanizaki J, et al. Induction of PD-L1 expression by the EML4-ALK oncoprotein and downstream signaling pathways in non-small cell lung cancer. Clin Cancer Res. 2015;21:4014–21.
Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med. 2015;373:1627–39.
Hoensch H, Morgenstern I, Petereit G, Siepmann M, Peters WH, Roelofs HM, et al. Influence of clinical factors, diet, and drugs on the human upper gastrointestinal glutathione system. Gut. 2002;50:235–40.
Peccatori FA, Azim HA, Jr., Orecchia R, Hoekstra HJ, Pavlidis N, Kesic V et al. Cancer, pregnancy and fertility: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24 Suppl 6:vi160–70.
Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH, et al. Fertility preservation for patients with cancer: american Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013;31:2500–10.
Bermejo B, Navarro B, Lluch A. Cáncer y fertilidad. ARBOR Ciencia, Pensamiento y Cultura. 2015;191:a239.
Woodruff TK, Smith K, Gradishar W. Oncologists’ role in patient fertility care: a call to action. JAMA Oncol. 2016;2:171–2.
Pollán M, Planchuelo A, Campelo RG, López Ríos F, Gómez J, Trigo JM, et al. Cáncer de Pulmón en Mujeres. ICAPEM: Aspectos Diferenciales; 2015.
Acknowledgements
The authors wish to thank Fernando Sánchez-Barbero from HealthCo S.L. (Madrid, Spain) for his editorial help in preparing the first draft of this manuscript. The necessary scientific meetings along with medical writing services were supported financially by ICAPEM. All authors have approved the final version of the submitted manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they do not have any conflict of interest that may inappropriately influence this work.
Ethical statement
The study has been performed in accordance with the ethical standards of the Declaration of Helsinki and its later amendments. This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent statement
Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Rights and permissions
About this article
Cite this article
Isla, D., Majem, M., Viñolas, N. et al. A consensus statement on the gender perspective in lung cancer. Clin Transl Oncol 19, 527–535 (2017). https://doi.org/10.1007/s12094-016-1578-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-016-1578-x