Abstract
Objective
Analyze the characteristics, surgical technique, morbidity and survival of patients treated with extreme liver surgery.
Materials and methods
We present a series of consecutive patients with malignant liver tumors in hepatocaval confluence treated in a single center with extreme liver surgery (April 2008–March 2015). Data were collected prospectively and analyzed with SPSS 21.0.
Results
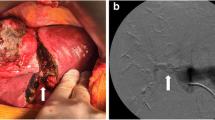
12 patients were included. 50 % were male and 50 % were female with a mean age of 59 ± 10 years old. The median of comorbidities was 7 according to the Charlson Age Comorbidity Index. The 75 % of the tumors were metastases, most of them from colorectal cancer. Most of the patients received neoadjuvant chemotherapy and in 58 % preoperative portal embolization was performed. Major hepatectomies were performed (66.7 % extended right hepatectomy, 33.3 % left extended hepatectomy). The 83.3 % of the patients needed vascular reconstruction. Postoperative morbidity was more than grade II in 50 % of the patients according to Dindo–Clavien classification. There was no intraoperative mortality. The postoperative mortality rate at 90 days was 33 % due to hepatic failure and biliary fistula. In December 2015, 33 % of the patients are still alive with a mean survival of 19 months (13–23) with an ECOG Performance Status of 0.
Conclusion
Extreme liver surgery carries a high rate of morbidity and mortality that seem to increase with age and with higher tumor volumes, according to the literature. It is a therapeutic option to consider in patients with low comorbidity suffering from malignant neoplasms that involve the hepatocaval confluence, when no other treatment with curative intention can be performed.



Similar content being viewed by others
References
Hatzaras I, Bischof DA, Fahy B, Cosgrove D, Pawlik TM. Treatment options and surveillance strategies after therapy for hepatocellular carcinoma. Ann Surg Oncol. 2014;21(3):758–66.
Lee H, Heo JS, Cho YB, Yun SH, Kim HC, Lee WY, et al. Hepatectomy vs radiofrequency ablation for colorectal liver metastasis: a propensity score analysis. World J Gastroenterol. 2015;21(11):3300–7.
Mossdorf A, Ulmer F, Junge K, Heidenhain C, Hein M, Temizel I, et al. Bypass during liver transplantation: anachronism or revival? Liver transplantation using a combined venovenous/portal venous bypass-experiences with 163 liver transplants in a newly established liver transplantation program. Gastroenterol Res Pract. 2015;2015:967951. doi:10.1155/2015/967951.
Budd JM, Isaac JL, Bennett J, Freeman JW. Morbidity and mortality associated with large-bore percutaneous venovenous bypass cannulation for 312 orthotopic liver transplantations. Liver Transpl. 2001;7(4):359–62.
Hemming AW, Reed AI, Langham MR Jr, Fujita S, Howard RJ. Combined resection of the liver and inferior vena cava for hepatic malignancy. Ann Surg. 2004;239:712–9 (discussion 719–21).
Azoulay D, Pascal G, Salloum C, Adam R, Castaing D, Tranecol N. Vascular reconstruction combined with liver resection for malignant tumours. Br J Surg. 2013;100(13):1764–75.
Chan AC, Chan SC, Yiu MK, Ho KL, Wong EH, Lo CH. Technical considerations for radical resection of a primary leiomyosarcoma of the vena cava. HPB (Oxford). 2012;14(8):565–8.
Azoulay D, Castaing D, Smail A, Adam R, Cailliez V, Laurent A, et al. Resection of nonresectable liver metastases from colorectal cancer after percutaneous portal vein embolization. Ann Surg. 2000;231(4):480–6.
Azoulay D, Andreani P, Maggi U, Salloum C, Perdigao F, Sebagh M. Combined liver resection and reconstruction of the supra-renal vena cava: the Paul Brousse experience. Ann Surg. 2006;244(1):80–8.
Heaney JP, Stanton WK, Halbert DS, Seidel J, Vice T. An improved technic for vascular isolation of the liver: experimental study and case reports. Ann Surg. 1966;163(2):237–41.
Shaw BW, Martin DJ, Marquez JM, Kang YG, Bugbee AC, Iwatsuki S, et al. Venous bypass in clinical liver transplantation. Ann Surg. 1984;200(4):524–34.
Fortner JG, Shiu MH, Kinne DW, Kim DK, Castro EB, Watson RC, et al. Major hepatic resection using vascular isolation and hypothermic perfusion. Ann Surg. 1974;180(4):644–52.
Hoti E, Salloum C, Azoulay D. Hepatic resection with in situ hypothermic perfusion is superior to other resection techniques. Dig Surg. 2011;28(2):94–9.
Raab R, Schlitt HJ, Oldhafer KJ, Bornscheuer A, Lang H, Pichlmayr R. Ex-vivo resection techniques in tissue-preserving surgery for liver malignancies. Langenbecks Arch Surg. 2000;385(3):179–84.
Azoulay D, Lim C, Salloum C, Andreani P, Maggi U, Bartelmaos T, et al. Complex liver resection using standard total vascular exclusion, venovenous bypass, and in situ hypothermic portal perfusion: an audit of 77 consecutive cases. Ann Surg. 2014;00:1–12.
Hannoun L, Delrivière L, Gibbs P, Borie D, Vaillant JC, Delva E. Major extended hepatic resections in diseased livers using hypothermic protection: preliminary results from the first 12 patients treated with this new technique. J Am Coll Surg. 1996;183(6):597–605.
Dinant S, van Veen SQ, Roseboom HJ, van Vliet AK, van Gulik TM. Liver protection by hypothermic perfusion at different temperatures during total vascular exclusion. Liver Int. 2006;26(4):486–93.
FitzHenry J. The ASA classification and peri-operative risk. Ann R Coll Surg Engl. 2011;93(3):185–7.
Dias-Santos D, Ferrone CR, Zheng H, Lillemoe KD, Fernández-Del Castillo C. The Charlson age comorbidity index predicts early mortality after surgery for pancreatic cancer. Surgery. 2015;157(5):881–7.
Dindo D, Demartines H, Clavien P. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Makuuchi M, Hasegawa H, Yamazaki S, Takayasu K. Four new hepatectomy procedures for resection of the right hepatic vein and preservation of the inferior right hepatic vein. Surg Gynecol Obstet. 1987;164(1):68–72.
Hirai I, Kimura W, Fuse A, Yamamoto T, Moriya T, Mizutani M. Evaluation of inferior right hepatic vein-preserving hepatectomy with resection of the superior right hepatic vein. Hepatogastroenterology. 2006;53(70):516–20.
Nakamura S, Sakaguchi S, Kitazawa T, Suzuki S, Koyano K, Muro H. Hepatic vein reconstruction for preserving remnant liver function. Arch Surg. 1990;125(11):1455–9.
Hemming AW, Reed AI, Langham MR, Fujita S, van der Werf WJ, Howard RJ. Hepatic vein reconstruction for resection of hepatic tumors. Ann Surg. 2002;235(6):850–8.
Soejima Y, Matsumoto T, Shirabe K, Maehara Y. Tube cavoplasty using autologous vein grafts for resected inferior vena cava reconstruction. Surg Today. 2013;43(4):452–5.
Shimoda M, Marubashi S, Dono K, Miyamoto A, Takeda Y, Nagano H, et al. Utilization of autologous vein graft for replacement of the inferior vena cava in living-donor liver transplantation for obliterative hepatocavopathy. Transpl Int. 2007;20(9):804–7.
Ohwada S, Hamada K, Kawate S, Sunose Y, Tomizawa N, Yamada T, et al. Left renal vein graft for vascular reconstruction in abdominal malignancy. World J Surg. 2007;31(6):1215–20.
Aoki T, Sugawara Y, Imamura H, Seyama Y, Minagawa M, Hasegawa K, et al. Hepatic resection with reconstruction of the inferior vena cava or hepatic venous confluence for metastatic liver tumor from colorectal cancer. J Am Coll Surg. 2004;198(3):366–72.
Hemming AW, Mekeel KL, Zendejas I, Kim RD, Sicklick JK, Reed AI. Resection of the liver and inferior vena cava for hepatic malignancy. J Am Coll Surg. 2013;217(1):115–24 (discussion 124–5).
Arii S, Teramoto K, Kawamura T, Takamatsu S, Sato E, Nakamura N, et al. Significance of hepatic resection combined with inferior vena cava resection and its reconstruction with expanded polytetrafluoroethylene for treatment of liver tumors. J Am Coll Surg. 2003;196(2):243–9.
Wachtel H, Jackson BM, Bartlett EK, Karakousis GC, Roses RE, Bavaria JE, et al. Resection of primary leiomyosarcoma of the inferior vena cava (IVC) with reconstruction: a case series and review of the literature. J Surg Oncol. 2015;111(3):328–33.
Azoulay D, Maggi U, Lim C, Malek A, Compagnon P, Salloum C, et al. Liver resection using total vascular exclusion of the liver preserving the caval flow, in situ hypothermic portal perfusion and temporary porta-caval shunt: a new technique for central tumors. Hepatobiliary Surg Nutr. 2014;3(3):149–53.
Díaz-Rubio EG. Biomarkers and anti-EGFR therapies for KRAS wild-type tumors in metastatic colorectal cancer patients. An R Acad Nac Med. 2009;126(2):243–57 (discussion 258–62).
Siena S, Sartore-Bianchi A, di Nicolantonio F, Balfour J, Bardelli A. Biomarkers predicting clinical outcome of epidermal growth factor receptor-targeted therapy in metastatic colorectal cancer. J Natl Cancer Inst. 2009;101(19):1308–24.
László L. Predictive and prognostic factors in the complex treatment of patients with colorectal cancer. Magy Onkol. 2010;54(4):383–94.
Poston GJ, Adam R, Alberts S, Curley S, Figueras J, Haller D, et al. OncoSurge: a strategy for improving resectability with curative intent in metastatic colorectal cancer. J Clin Oncol. 2005;23(28):7125–34.
Eker B, Ozaslan E, Karaca H, Berk V, Bozkurt O, Inanc M, et al. Factors affecting prognosis in metastatic colorectal cancer patients. Asian Pac J Cancer Prev. 2015;16(7):3015–21.
Kuo IM, Huang SF, Chiang JM, Yeh CY, Chan KM, Chen JS, et al. Clinical features and prognosis in hepatectomy for colorectal cancer with centrally located liver metastasis. World J Surg Oncol. 2015;13(1):92.
Frankel TL, d’Angelica MI. Hepatic resection for colorectal metastases. J Surg Oncol. 2014;109(1):2–7.
Brouquet A, Nordlinger B. Neoadjuvant therapy of colorectal liver metastases: lessons learned from clinical trials. J Surg Oncol. 2010;102(8):932–6.
Adam R, Lucidi V, Bismuth H. Hepatic colorectal metastases: methods of improving resectability. Surg Clin North Am. 2004;84(2):659–71.
Nuzzo G, Giordano M, Giuliante F, Lopez-Ben S, Albiol M, Figueras J. Complex liver resection for hepatic tumours involving the inferior vena cava. Eur J Surg Oncol. 2011;37(11):921–7.
Malde DJ, Khan A, Prasad KR, Toogood GJ, Lodge JA. Inferior vena cava resection with hepatectomy: challenging but justified. HPB (Oxford). 2011;13(11):802–10.
Russell MC. Complications following hepatectomy. Surg Oncol Clin N Am. 2015;24(1):73–96.
Floyd J, Mirza I, Sachs B, Perry MC. Hepatotoxicity of chemotherapy. Semin Oncol. 2006;33(1):50–67.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Ethical approval
This study has been approved by the ethics committee of Hospital Universitari Doctor Josep Trueta de Girona in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Codony, C., López-Ben, S., Albiol, M. et al. Extreme liver surgery as treatment of liver tumors involving the hepatocaval confluence. Clin Transl Oncol 18, 1131–1139 (2016). https://doi.org/10.1007/s12094-016-1495-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-016-1495-z