Abstract
Objective
The aim of this study was to assess the predictive value of neutrophil/lymphocyte and platelet/lymphocyte ratios for borderline, malignant ovarian tumors, and borderline cases with microinvasion.
Methods
Totally 275 women with sonographically detected ovarian tumor were enrolled for this study. All subjects underwent gynecological surgery via endoscopic or conventional approach and ovarian masses were all evaluated histopathologically by the same pathologist. All study population was divided into three groups as group with borderline tumors, benign tumors, or malignant tumors according to the histopathological diagnosis. Just before surgical intervention, a blood sample was obtained from each participant to analyze CA125 level, neutrophil, platelet, and lymphocyte count.
Results
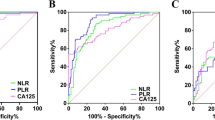
Neutrophil/lymphocyte ratio (AUC = 0.604, P = 0.02) was a significant predictor for malignant cases. Optimal cutoff value for the neutrophil/lymphocyte ratio was found to be 2.47 with 63.4 % sensitivity and 63.5 % specificity for malignancy prediction. Odds ratio of high neutrophil/lymphocyte ratio for malignancy risk was 2.5 (95 % CI 1.3–4.8, P = 0.004). Platelet/lymphocyte ratio (AUC = 0.621, P = 0.007) was a significant predictor for malignant cases. Platelet/lymphocyte ratio (AUC = 0.568, P = 0.05) was also predictive for cases without a benign mass. Optimal cutoff value for the platelet/lymphocyte ratio was found to be 144.3 with 54 % sensitivity and 59 % specificity for malignancy prediction. Odds ratio of high platelet/lymphocyte ratio for malignancy risk was 2.1 (95 % CI 1.1–3.8, P = 0.02).
Conclusion
Neutrophil/lymphocyte and platelet/lymphocyte ratios are predictors for malignant ovarian tumors but not borderline tumors even in case of microinvasion.



Similar content being viewed by others
References
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and can-cer. Cell. 2010;140(6):883–99.
O’Callaghan DS, O’Donnell D, O’Connell F, O’Byrne KJ. The role of inflammation in the pathogenesis of non-small cell lung cancer. J Thorac Oncol. 2010;5(12):2024–36.
Aggarwal BB, Vijayalekshmi RV, Sung B. Targeting inflammatory pathways for prevention and therapy of cancer: short-term friend, long-term foe. Clin Cancer Res. 2009;15(2):425–30.
Roxburgh CS, McMillan DC. Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol. 2010;6(1):149–63.
Viganó A, Bruera E, Jhangri GS, Newman SC, Fields AL, Suarez-Almazor ME. Clinical survival predictors in patients with advanced cancer. Arch Intern Med. 2000;160(6):861–8.
Li MX, Liu XM, Zhang XF, Zhang JF, Wang WL, Zhu Y, et al. Prognostic role of neutrophil-to-lymphocyte ratio in colorectal cancer: a systematic review and meta-analysis. Int J Cancer. 2014;134(10):2403–13.
Akın MN, Harmandar Kasap B, Uslu Yuvacı H. Neutrophil-to-lymphocyte ratio and platelet distribution in patients with endometrial cancer. J Obstet Gynaecol Res. 2015. doi:10.1111/jog.12723.
Yildirim M. Demir Cendek B, Filiz Avsar A. Differentiation between benign and malignant ovarian masses in the preoperative period using neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios. Mol Clin Oncol. 2015;3(2):317–21.
Karlsen MA, Sandhu N, Høgdall C, Christensen IJ, Nedergaard L, Lundvall L, et al. Evaluation of HE4, CA125, risk of ovarian malignancy algorithm (ROMA) and risk of malignancy index (RMI) as diagnostic tools of epithelial ovarian cancer in patients with a pelvic mass. Gynecol Oncol. 2012;127(2):379–83.
Bast RC Jr, Skates S, Lokshin A, Moore RG. Differential diagnosis of a pelvic mass: improved algorithms and novel biomarkers. Int J Gynecol Cancer. 2012;22(Suppl 1):S5–8.
Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001;357:539–45.
de Visser KE, Eichten A, Coussens LM. Paradoxical roles of the immune system during cancer development. Nat Rev Cancer. 2006;6:24–37.
Shappell HW, Riopel MA, Smith Sehdev AE, Ronnett BM, Kurman RJ. Diagnostic criteria and behavior of ovarian seromucinous (endocervical-type mucinous and mixed cell-type) tumors: atypical proliferative (borderline) tumors, intraepithelial, microinvasive, and invasive carcinomas. Am J Surg Pathol. 2002;26(12):1529–41.
Templeton AJ, McNamara MG, Šeruga B, Vera-Badillo FE, Aneja P, Ocaña A, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106(6):dju124. doi:10.1093/jnci/dju124.
Paramanathan A, Saxena A, Morris DL. A systematic review and meta-analysis on the impact of pre-operative neutrophil lymphocyte ratio on long term outcomes after curative intent resection of solid tumours. Surg Oncol. 2014;23(1):31–9.
Guthrie GJ, Charles KA, Roxburgh CS, Horgan PG, McMillan DC, Clarke SJ. The systemic inflammation-based neutrophil-lymphocyte ratio: experience in patients with cancer. Crit Rev Oncol Hematol. 2013;88(1):218–30.
Yildirim MA, Seckin KD, Togrul C, Baser E, Karsli MF, Gungor T, et al. HC. Roles of neutrophil/lymphocyte and platelet/lymphocyte ratios in the early diagnosis of malignant ovarian masses. Asian Pac J Cancer Prev. 2014;15(16):6881–5.
Topcu HO, Guzel AI, Ozer I, Kokanali MK, Gokturk U, Muftuoglu KH, et al. Comparison of neutrophil/lymphocyte and platelet/lymphocyte ratios for predicting malignant potential of suspicious ovarian masses in gynecology practice. Asian Pac J Cancer Prev. 2014;15(15):6239–41.
Asher V, Lee J, Innamaa A, Bali A. Preoperative platelet lymphocyte ratio as an independent prognostic marker in ovarian cancer. Clin Transl Oncol. 2011;13(7):499–503.
Szalayova G, James TA, Rincon M. A framework for the role of acute inflammation in tumor progression. Breast Cancer Res Treat. 2015;151(2):235–8.
Acknowledgments
We would like to thank all the patients and primary care physicians.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
Signed informed consent was obtained from all the participants.
This study complies with the latest Declaration of Helsinki for Researches involving Human Participants and/or Animals.
Rights and permissions
About this article
Cite this article
Polat, M., Senol, T., Ozkaya, E. et al. Neutrophil to lymphocyte and platelet to lymphocyte ratios increase in ovarian tumors in the presence of frank stromal invasion. Clin Transl Oncol 18, 457–463 (2016). https://doi.org/10.1007/s12094-015-1387-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-015-1387-7