Abstract
Mitochondrial dysfunction and subsequent autophagy, which are common features in central nervous system (CNS) disorders, were found to contribute to neuronal cell injury after subarachnoid hemorrhage (SAH). (-)-Epigallocatechin-3-gallate (EGCG), the main biological active of tea catechin, is well known for its beneficial effects in the treatment of CNS diseases. Here, the ability of EGCG to rescue cellular injury and mitochondrial function following the improvement of autophagic flux after SAH was investigated. As expected, EGCG-protected mitochondrial function depended on the inhibition of cytosolic Ca2+ concentration ([Ca2+]i) influx via voltage-gated calcium channels (VGCCs) and, consequently, mitochondrial Ca2+ concentration ([Ca2+]m) overload via mitochondrial Ca2+ uniporter (MCU). The attenuated [Ca2+]i and [Ca2+]m levels observed in the EGCG-treated group likely lessened oxyhemoglobin (OxyHb)-induced mitochondrial dysfunction, including mitochondrial membrane potential depolarization, mitochondrial membrane permeability transition pore (mPTP) opening, reactive oxygen species (ROS), and cytochrosome c (cyt c) releasing. Subsequently, EGCG can restore the disrupted autophagy flux after SAH both at the initiation and formation stages by regulating Atg5, LC3B, and Becn-1 (Beclin-1) mRNA expressions. Thus, precondition EGCG resulted in autophagosomes and more autolysosomes compared with SAH group. As a result, EGCG pre-treatment increased the neurological score and decreased cell death. This study suggested that the mitochondrial dysfunction and abnormal autophagy flux synergistically contribute to SAH pathogenesis. Thus, EGCG can be regarded as a new pharmacological agent that targets both mitochondria and altered autophagy in SAH therapy.











Similar content being viewed by others
References
Hop JW, Rinkel GJ, Algra A, van Gijn J (1997) Case-fatality rates and functional outcome after subarachnoid hemorrhage: a systematic review. Stroke 28:660–664
Sehba FA, Hou J, Pluta RM, Zhang JH (2012) The importance of early brain injury after subarachnoid hemorrhage. Prog Neurobiol 97(1):14–37. doi:10.1016/j.pneurobio.2012.02.003
Sehba FA, Pluta RM, Zhang JH (2011) Metamorphosis of subarachnoid hemorrhage research: from delayed vasospasm to early brain injury. Mol Neurobiol 43:27–40. doi:10.1007/s12035-010-8155-z
Ayer RE, Zhang JH (2008) Oxidative stress in subarachnoid haemorrhage: significance in acute brain injury and vasospasm. Acta Neurochir Suppl 104:33–41
Hua Y, Keep RF, Hoff JT, Xi G (2008) Deferoxamine therapy for intracerebral hemorrhage. Acta Neurochir Suppl 105:3–6
Higuchi A, Yonemitsu K, Koreeda A, Tsunenari S (2003) Inhibitory activity of epigallocatechin gallate (EGCG) in paraquat-induced microsomal lipid peroxidation—a mechanism of protective effects of EGCG against paraquat toxicity. Toxicology 183:143–149
Ingall T, Asplund K, Mähönen M, Bonita R (2000) A multinational comparison of subarachnoid hemorrhage epidemiology in the WHO MONICA stroke study. Stroke 31(5):1054–1061
Liang W, Lee AH, Binns CW, Huang R, Hu D, Zhou Q (2009) Tea consumption and ischemic stroke risk: a case-control study in southern China. Stroke 40(7):2480–2485. doi:10.1161/STROKEAHA.109.548586
Yao C, Zhang J, Liu G, Chen F, Lin Y (2014) Neuroprotection by (-)-epigallocatechin-3-gallate in a rat model of stroke is mediated through inhibition of endoplasmic reticulum stress. Mol Med Rep 9(1):69–76. doi:10.3892/mmr.2013.1778
Hyung SJ, DeToma AS, Brender JR, Lee S, Vivekanandan S, Kochi A et al (2013) Insight into antiamyloidogenic properties of the green tea extract (-)-epigallocatechin-3-gallate toward metal-associated amyloid-β species. Proc Natl Acad Sci U S A 110(10):3743–3748. doi:10.1073/pnas.1220326110
Itoh T, Tabuchi M, Mizuguchi N, Imano M, Tsubaki M, Nishida S et al (2013) Neuroprotective effect of (-)-epigallocatechin-3-gallate in rats when administered pre- or post-traumatic brain injury. J Neural Transm 120(5):767–783. doi:10.1007/s00702-012-0918-4
Biasibetti R, Tramontina AC, Costa AP, Dutra MF, Quincozes-Santos A, Nardin P et al (2013) Green tea (-)epigallocatechin-3-gallate reverses oxidative stress and reduces acetylcholinesterase activity in a streptozotocin-induced model of dementia. Behav Brain Res 236(1):186–193. doi:10.1016/j.bbr.2012.08.039
Ranzato E, Magnelli V, Martinotti S, Waheed Z, Cain SM, Snutch TP et al (2014) Epigallocatechin-3-gallate elicits Ca2+ spike in MCF-7 breast cancer cells: essential role of Cav3.2 channels. Cell Calcium 56(4):285–295. doi:10.1016/j.ceca.2014.09.002
Nakagawa K, Miyazawa T (1997) Absorption and distribution of tea catechin, (-)-epigallocatechin-3-gallate, in the rat. J Nutr Sci Vitaminol 43(6):679–684
Zhang Y, Yang ND, Zhou F, Shen T, Duan T, Zhou J et al (2012) (-)-Epigallocatechin-3-gallate induces non-apoptotic cell death in human cancer cells via ROS-mediated lysosomal membrane permeabilization. PLoS One 7(10):e46749. doi:10.1371/journal.pone.0046749
Weng Z, Zhou P, Salminen WF, Yang X, Harrill AH, Cao Z et al (2014) Green tea epigallocatechin gallate binds to and inhibits respiratory complexes in swelling but not normal rat hepatic mitochondria. Biochem Biophys Res Commun 443(3):1097–1104. doi:10.1016/j.bbrc.2013.12.110
Mikutis G, Karakose H, Jaiswal R, LeGresley A, Islam T, Fernandez-Lahore M, Kuhnert N (2013) Phenolic promiscuity in the cell nucleus—epigallocatechingallate (EGCG) and theaflavin-3,3′-digallate from green and black tea bind to model cell nuclear structures including histone proteins, double stranded DNA and telomeric quadruplex DNA. Food Funct 4(2):328–337. doi:10.1039/c2fo30159h
Mo HZ, Chen Y, Huang LY, Zhang H, Li JX, Zhou WK (2013) Neuroprotecitve effect of tea polyphenols on oxyhemoglobin induced subarachnoid hemorrhage in mice. Oxidative Med Cell Longev 2013:743983. doi:10.1155/2013/743938
Tait SW, Green DR (2012) Mitochondria and cell signaling. J Cell Sci 125:807–815. doi:10.1242/jcs.099234
Soboll S (1995) Regulation of energy metabolism in liver. J Bioenerg Biomembr 27(6):571–582
Smith RA, Hartley RD, Cochemé HM, Murphy MP (2012) Mitochondrial pharmacology. Trends Pharmacol Sci 33:341–352. doi:10.1016/j.tips.2012.03.010
Martin TF, Grishanin RN (2003) PC12 cells as a model for studies of regulated secretion in neuronal and endocrine cells. Methods Cell Biol 71:267–286
Kang KS, Wen Y, Yamabe N, Fukui M, Bishop SC, Zhu BT (2010) Dual beneficial effects of (-)-epigallocatechin-3-gallate on levodopa methylation and hippocampal neurodegeneration: in vitro and in vivo studies. PLoS One 5(8):e11951. doi:10.1371/journal.pone.0011951
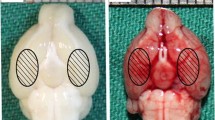
Huang LY, Wan J, Chen Y, Wang ZW, Hui L, Li Y et al (2013) Inhibitory effects of p38 inhibitor against mitochondrial dysfunction in the early brain injury after subarachnoid hemorrhage in mice. Brain Res 1517:133–140. doi:10.1016/j.brainres.2013.04.010
Garcia JH, Wagner S, Liu KF, Hu XJ (1995) Neurological deficit and extent of neuronal necrosis attributable to middle cerebral artery occlusion in rats. Statistical validation. Stroke 26(4):627–634, discussion 635
Kim HS, Montana V, Jang HJ, Parpura V, Kim JA (2013) Epigallocatechingallate (EGCG) stimulates autophagy in vascular endothelial cells: a potential role for reducing lipid accumulation. J Biol Chem 288(31):22693–22705. doi:10.1074/jbc.M113.477505
Chou CW, Huang WJ, Tien LT, Wang SJ (2007) (-)-Epigallocatechingallate, the most active polyphenolic catechin in green tea, presynaptically facilitates Ca2+-dependent glutamate release via activation of protein kinase C in rat cerebral cortex. Synapse 61(11):889–902
Kargacin ME, Emmett TL, Kargacin GJ (2011) Epigallocatechin-3-gallatehasdual, independent effects on the cardiac sarcoplasmic reticulum/endoplasmic reticulum Ca2+ ATPase. J Muscle Res Cell Motil 32:89–98. doi:10.1007/s10974-011-9256-7
Soler F, Asensio MC, Fernandez-Belda F (2012) Inhibition of the intracellular Ca(2+) transporter SERCA (sarco-endoplasmic reticulum Ca(2+)-ATPase) by the natural polyphenol epigallocatechin-3-gallate. J Bioenerg Biomembr 44(5):597–605. doi:10.1007/s10863-012-9462-z
Shi X, Fu Y, Liao D, Chen Y, Liu J (2014) Alterations of voltage-dependent calcium channel currents in basilar artery smooth muscle cells at early stage of subarachnoid hemorrhage in a rabbit model. PLoS One 9(1):e84129. doi:10.1371/journal.pone.0084129
Oliviero F, Sfriso P, Scanu A, Fiocco U, Spinella P, Punzi L (2013) Epigallocatechin-3-gallate reduces inflammation induced by calcium pyrophosphate crystals in vitro. Front Pharmacol 4:51. doi:10.3389/fphar.2013.00051
Yan H, Zhang D, Hao S, Li K, Hang CH (2015) Role of mitochondrial calcium uniporter in early brain injury after experimental subarachnoid hemorrhage. Mol Neurobiol 52(3):1637–1647. doi:10.1007/s12035-014-8942-z
Hausenloy D, Wynne A, Duchen M, Yellon D (2004) Transient mitochondrial permeability transition pore opening mediates preconditioning-induced protection. Circulation 109(14):1714–1717
Chen H, Liu C, Yin J, Chen Z, Xu J, Wang D et al (2015) Mitochondrial cyclophilin D as a potential therapeutic target for ischemia-induced facial palsy in rats. Cell Mol Neurobiol 35(7):931–941. doi:10.1007/s10571-015-0188-4
Wu CC, Bratton SB (2013) Regulation of the intrinsic apoptosis pathway by reactive oxygen species. Antioxid Redox Signal 19(6):546–558. doi:10.1089/ars
Shao A, Wang Z, Wu H, Dong X, Li Y, Tu S et al (2014) Enhancement of autophagy by histone deacetylase inhibitor trichostatin A ameliorates neuronal apoptosis after subarachnoid hemorrhage in rats. Mol Neurobiol in press
Liu Y, Li J, Wang Z, Yu Z, Chen G (2014) Attenuation of early brain injury and learning deficits following experimental subarachoid hemorrhage secondary to cystatin C: possible involvement of the autophagy pathway. Mol Neurobiol 49(2):1043–1054. doi:10.1007/s12035-013-8579-3
Jing CH, Wang L, Liu PP, Wu C, Ruan D, Chen G (2012) Autophagy activation is associated with neuroprotection against apoptosis via a mitochondrial pathway in a rat model of subarachnoid hemorrhage. Neuroscience 213:144–153. doi:10.1016/j.neuroscience.2012.03.055
Wang Z, Shi XY, Yin J, Zuo G, Zhang J, Chen G (2012) Role of autophagy in early brain injury after experimental subarachnoid hemorrhage. J Mol Neurosci 46:192–202. doi:10.1007/s12031-011-9575-6
Carloni S, Buonocore G, Balduini W (2008) Protective role of autophagy in neonatal hypoxia-ischemia induced brain injury. Neurobiol Dis 32:329–339. doi:10.1016/j.nbd.2008.07.022
Wen YD, Sheng R, Zhang LS, Han R, Zhang X, Zhang XD et al (2008) Neuronal injury in rat model of permanent focal cerebral ischemia is associated with activation of autophagic and lysosomal pathways. Autophagy 4(6):762–769
Lee JY, He Y, Sagher O, Keep R, Hua Y, Xi G (2009) Activated autophagy pathway in experimental subarachnoid hemorrhage. Brain Res 1287:126–135. doi:10.1016/j.brainres.2009.06.028
Zhou J, Farah BL, Sinha RA, Wu Y, Singh BK, Bay BH et al (2014) Epigallocatechin-3-gallate (EGCG), a green tea polyphenol, stimulates hepatic autophagy and lipid clearance. PLoS One 9:e87161. doi:10.1371/journal.pone.0087161
Gu HF, Nie YX, Tong QZ, Tang YL, Zeng Y, Jing KQ et al (2014) Epigallocatechin-3-gallate attenuates impairment of learning and memory in chronic unpredictable mild stress-treated rats by restoring hippocampal autophagic flux. PLoS One 9(11):e112683. doi:10.1371/journal.pone.0112683
Sarkar C, Zhao Z, Aungst S, Sabirzhanov B, Faden AI, Lipinski MM (2014) Impaired autophagy flux is associated with neuronal cell death after traumatic brain injury. Autophagy 10(12):2208–2222. doi:10.4161/15548627.2014.981787
Mizushima N, Yoshimori T, Ohsumi Y (2011) The role of ATG proteins in autophagosome formation. Annu Rev Cell Dev Biol 27:107–132. doi:10.1146/annurev-cellbio-092910-154005
Wang Y, Gao AJ, Xu X, Dang BQ, You WC, Li HY et al (2015) The neuroprotection of lysosomotropic agents in experimental subarachnoid hemorrhage probably involving the apoptosis pathway triggering by cathepsins via chelating intralysosomal iron. Mol Neurobiol 52(1):64–77. doi:10.1007/s12035-014-8846-y
Kosacka J, Kern M, Klöting N, Paeschke S, Rudich A, Haim Y et al (2015) Autophagy in adipose tissue of patients with obesity and type 2 diabetes. Mol Cell Endocrinol 409:21–32. doi:10.1016/j.mce.2015.03.015
Williams A, Sarkar S, Cuddon P, Ttofi EK, Saiki S, Siddiqi FH et al (2008) Novel targetsfor Huntington’s disease in an mTOR-independent autophagy pathway. Nat Chem Biol 4(5):295–305. doi:10.1038/nchembio.79
Fleming A, Noda T, Yoshimori T, Rubinsztein DC (2011) Chemical modulators of autophagy as biological probes and potential therapeutics. Nat Chem Biol 7(1):9–17. doi:10.1038/nchembio.500
Vidal RL, Matus S, Bargsted L, Hetz C (2014) Targeting autophagy in neurodegenerative diseases. Trends Pharmacol Sci 35(11):583–591. doi:10.1016/j.tips.2014.09.002
Büttner S, Broeskamp F, Sommer C, Markaki M, Habernig L, Alavian-Ghavanini A et al (2014) Spermidine protects against α-synuclein neurotoxicity. Cell Cycle 13(24):3903–3908. doi:10.4161/15384101.2014.973309
Jeong JK, Moon MH, Bae BC, Lee YJ, Seol JW, Kang HS et al (2012) Autophagy induced by resveratrol prevents human prion protein-mediated neurotoxicity. Neurosci Res 73(2):99–105. doi:10.1016/j.neures.2012.03.005
Jiang TF, Zhang YJ, Zhou HY, Wang HM, Tian LP, Liu J et al (2013) Curcumin ameliorates the neurodegenerative pathology in A53T α-synuclein cell model of Parkinson’s disease through the downregulation of mTOR/p70S6K signaling and the recovery of macroautophagy. J Neuroimmune Pharmacol 8(1):356–369. doi:10.1007/s11481-012-9431-7
Wu Y, Li X, Zhu JX, Xie W, Le W, Fan Z et al (2011) Resveratrol-activated AMPK/SIRT1/autophagy in cellular models of Parkinson’s disease. Neurosignals 19(3):163–174. doi:10.1159/000328516
Martinez-Vicente M (2015) Autophagy in neurodegenerative diseases: from pathogenic dysfunction to therapeutic modulation. Semin Cell Dev Biol. doi:10.1016/j.semcdb.2015.03.005
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Funding
This work is supported by the National Nature Sciences Foundation of China (No. 31200519) and Natural Science Foundation of Henan (No. 132300410339).
Rights and permissions
About this article
Cite this article
Chen, Y., Huang, L., Zhang, H. et al. Reduction in Autophagy by (-)-Epigallocatechin-3-Gallate (EGCG): a Potential Mechanism of Prevention of Mitochondrial Dysfunction After Subarachnoid Hemorrhage. Mol Neurobiol 54, 392–405 (2017). https://doi.org/10.1007/s12035-015-9629-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-015-9629-9