Abstract
Background/Objective
Children supported by extracorporeal membrane oxygenation (ECMO) are at risk of catastrophic neurologic injury and brain death. Timely determination of brain death is important for minimizing psychological distress for families, resource allocation, and organ donation. Reports of successful determination of brain death in pediatric patients supported by ECMO are limited. The determination of brain death by clinical criteria requires apnea testing, which has historically been viewed as challenging in patients supported by ECMO. We report eight pediatric patients who underwent a total of 14 brain death examinations, including apnea testing, while supported by veno-arterial ECMO (VA-ECMO), resulting in six cases of clinical determination of brain death.
Methods
We performed a retrospective review of the medical records of pediatric patients who underwent brain death examination while supported by VA-ECMO between 2010 and 2018 at a single tertiary care children’s hospital.
Results
Eight patients underwent brain death examination, including apnea testing, while supported by VA-ECMO. Six patients met criteria for brain death, while two had withdrawal of technical support after the first examination. During the majority of apnea tests (n = 13/14), the ECMO circuit was modified to achieve hypercarbia while maintaining oxygenation and hemodynamic stability. The sweep flow was decreased prior to apnea testing in ten brain death examinations, carbon dioxide was added to the circuit during three examinations, and ECMO pump flows were increased in response to hypotension during two examinations.
Conclusions
Clinical determination of brain death, including apnea testing, can be performed in pediatric patients supported by ECMO. The ECMO circuit can be effectively modified during apnea testing to achieve a timely rise in carbon dioxide while maintaining oxygenation and hemodynamic stability.
Similar content being viewed by others
Introduction
Extracorporeal membrane oxygenation (ECMO) provides extra-circulatory support to patients with acute, severe cardiac and/or pulmonary failure and is often deployed emergently in the form of extracorporeal cardiopulmonary resuscitation (ECPR) to treat cardiac arrest unresponsive to conventional CPR. ECPR is primarily used in the setting of in-hospital cardiac arrest, with survival rates ranging from 29 to 57% in children and neonates [1,2,3,4,5,6]. Based on data from the Extracorporeal Life Support Organization registry of over 170 ECMO centers worldwide, the number of patients receiving ECPR increased dramatically from 1992 to 2017 [7, 8]. Unfortunately, the use of ECPR is accompanied by a high risk of neurologic injury, due to both the precipitating event and complications related to ECMO [1, 9]. Barrett et al. [1] reported a 22% incidence of neurologic injury in children undergoing ECPR with 11% of these patients experiencing brain death; however, it is unknown how or whether these children underwent formal testing for brain death. Similarly, Thiagarajan et al. [7] reported that 21% of 295 adults treated with ECPR experienced brain death, and patients with brain death had earlier withdrawal of ECMO support.
The determination of brain death by clinical criteria requires apnea testing to demonstrate a failure of medullary respiratory centers. While this has historically been viewed as challenging in patients supported by ECMO given that ventilation and oxygenation are controlled by the ECMO circuit [10], case reports and small case series, primarily in adults, suggest that apnea testing is feasible in this population [11,12,13,14,15,16,17,18]. Three cases of apnea testing have also been reported in pediatric patients on ECMO [19]. A positive apnea test requires a rise in PaCO2 to greater than or equal to 60 torr and greater than or equal to 20 torr above baseline in the absence of respiratory effort, desaturation to less than 85%, and hemodynamic instability [20]. In the majority of previously reported cases, this is achieved by adjusting the ECMO sweep gas flow rate, which allows for a sufficient rise in PaCO2 to complete apnea testing. In patients supported by veno-arterial (VA) ECMO, venous blood is removed from the circulation, passed through the ECMO circuit, and then returned to the arterial system. As blood passes through the ECMO circuit, it comes into contact with a gas permeable membrane that allows for exchange of oxygen and carbon dioxide between the blood and an oxygenator. Removal of carbon dioxide via the ECMO circuit depends, in part, on the sweep gas flow rate; decreasing the sweep gas flow results in an increase in PaCO2. However, such changes come with the potential for complications of hypoxemia and hypotension [19].
Timely determination of brain death is important for minimizing psychological distress for families, resource allocation, and organ donation; thus, establishing reliable means of determining brain death in children on ECMO is of critical importance. We report our experience with 14 brain death examinations, including apnea testing, performed on eight pediatric patients on VA-ECMO, resulting in clinical determination of brain death in six patients. This represents the largest series to date of brain death examination in pediatric patients supported by ECMO. In addition, we describe a protocol for apnea testing for pediatric patients supported by ECMO, including techniques for addressing complications that may arise during testing.
Methods
We performed a retrospective review of the medical records of patients who underwent brain death examination while supported by VA-ECMO between 2010 and 2018 at a free-standing tertiary children’s hospital. Patients were identified from a prospective Neurocritical Care database, which comprises patients in the cardiac and pediatric intensive care units but not the neonatal intensive care unit. The electronic medical record was reviewed for demographic information, clinical characteristics, and details of the brain death examination. A standardized approach to brain death determination was developed in 2009 by our institution’s Neurocritical Care Program and updated in 2011 with the publication of guidelines for the determination of brain death in infants and children by the Society of Critical Care Medicine, the American Academy of Pediatrics, and the Child Neurology Society [20]. Patient assessment and apnea testing is performed in accordance with published guidelines [20], and a checklist is used to ensure that the examination is done consistently and safely (Supplementary Figure 1). Patients must meet the following prerequisite criteria: irreversible coma; absence of severe acid/base, electrolyte, or endocrine abnormality; temperature ≥ 35 °C; blood pressure in an acceptable range for age; absence of central nervous system (CNS) depressant medication effects; absence of neuromuscular blockade; and absence of spontaneous respirations. While it is not specifically included in our institutional checklist, train of four testing is recommended to determine the absence of neuromuscular blockade for patients who receive a neuromuscular blocking agent within 48 h prior to brain death examination. Neuroimaging that explains patient’s coma is preferred but is not an absolute requirement. Patients must demonstrate the absence of response to noxious stimulation of all four extremities, the absence of response to noxious stimulation of the supraorbital nerve, temporomandibular joint, or nasal passage, and the absence of all brainstem reflexes (pupillary, corneal, oculocephalic, oculovestibular, cough, and gag). Apnea testing is performed in a standardized fashion with requirements for a rise in PaCO2 to greater than or equal to 60 torr and greater than or equal to 20 torr above baseline. Two brain death examinations are performed, with the first examination performed no earlier than 24 h after CPR or other severe brain injury, and the second performed at least 12 h after the first. The interval between examinations may be shortened if ancillary testing (electroencephalogram (EEG) demonstrating electrocerebral silence or radionuclide cerebral blood flow study or conventional angiogram demonstrating the absence of cerebral perfusion) is consistent with brain death. However, a second neurologic examination is still required and should be completed in temporal proximity to the ancillary test. Ancillary testing is also required when any component of the examination or apnea testing cannot be completed, if there is uncertainty about the results of the neurologic examination, or if a medication effect may be present. Our institutional guidelines do not specifically address the determination of brain death for patients supported by ECMO, and thus, approaches to the apnea test in this cohort are variable. Descriptive statistics were used as needed. All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Research Ethics Board of Children’s National Medical Center and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Consent was not required.
Results
One hundred and ninety seven patients were supported by VA-ECMO in the cardiac and pediatric intensive care units between 2010 and 2018, 157 of whom had acquired or congenital heart disease and 40 who required ECMO support for non-cardiac diagnoses. Sixty-two of the patients with acquired or congenital heart disease and 16 of the patients with non-cardiac diagnoses died while supported by ECMO. Eight patients underwent brain death examination, including apnea testing, while supported by VA-ECMO during the study period. Six patients met criteria for brain death, while two had withdrawal of technical support after the first brain death examination. For the six patients who met criteria for brain death, the results of the first and second brain death examination did not differ.
Presenting Features and Neurologic Injury
Demographic and clinical characteristics are presented in Tables 1 and 2. The median age was four (range 1.9–17) years. Four patients had congenital heart disease, two had acquired heart disease, and two had multi-system disease. Five patients required emergent cannulation to ECMO during ECPR with a median time from the start of cardiac arrest to the start of ECMO flow of 65 (range 45–120) minutes. Four of the patients requiring emergent cannulation to ECMO had a post-arrest head computed tomography (CT) scan showing diffuse cerebral edema with herniation consistent with severe hypoxic ischemic injury, while the fifth had a body habitus that precluded use of our portable CT scanner. The remaining three patients in our cohort were noted to have abnormal pupils (one with bilateral fixed and dilated pupils, one with a unilateral fixed and dilated pupil, and one with a unilateral minimally reactive pupil) on neurologic examination 1–9 days after ECMO initiation. This prompted head CT which was notable for cerebral infarcts (n = 1), diffuse cerebral edema (n = 3), and/or herniation (n = 3). Clinical histories included one patient with septic shock, another with out-of-hospital cardiac arrest and acute respiratory distress syndrome, and a third who failed to separate from cardiopulmonary bypass after placement of a right ventricle to pulmonary artery conduit and takedown of a Blalock–Taussig shunt.
Brain Death Examination
Brain death testing was performed a median of 2.5 (IQR 2–3.75) days after initiation of ECMO, with a median interval between examinations of 18 (IQR 15–18.75) hours (Table 2). All patients met prerequisite criteria for brain death examination (irreversible coma; absence of severe acid/base, electrolyte, or endocrine abnormality; temperature ≥ 35 °C; blood pressure in an acceptable range for age; absence of CNS depressant medication effects; absence of neuromuscular blockade; and absence of spontaneous respirations) (Table 2). All patients had an absence of response to noxious stimulation of all four extremities, an absence of response to noxious stimulation of the supraorbital nerve, temporomandibular joint, or nasal passage, and an absence of all brainstem reflexes (pupillary, corneal, oculocephalic, oculovestibular, cough, and gag). The single patient in our cohort who had an interval of less than 12 h between brain death examinations had an electroencephalogram revealing electrocerebral silence. No patient had ancillary cerebral blood flow testing.
Apnea Testing
Blood gas and ECMO parameters during apnea testing are presented in Tables 3 and 4. Prior to initiation of apnea testing, ECMO flows ranged from 34.6 to 118.2 mL/kg/min (median 76 mL/kg/min; IQR 47.5–106.9 mL/kg/min). All patients were mechanically ventilated prior to apnea testing with ventilator FiO2 ranging from 40 to 100% and ECMO blender FiO2 ranging from 30 to 100%. Blood gases obtained prior to apnea testing revealed a median pH of 7.36 (IQR 7.33–7.41) with median PaCO2 45.3 (IQR 40.8–52.1) torr and median PaO2 302.6 (IQR 212.4–430.6) torr. The median duration of apnea testing was 14.5 (IQR 12.25–24.25) min. This may represent an overestimate as in a subset of cases it was not clear from the electronic medical record whether the initial blood gas was drawn prior to the clinical examination or after the clinical examination immediately prior to the apnea test.
All but one patient was pre-oxygenated via the ventilator with 100% FiO2 for greater than 10 min prior to apnea testing. During 12/14 apnea tests, oxygen was provided; when described, this was via a self-inflating bag with the patient valve open and positive end expiratory pressure (PEEP) set to 5–10 cmH2O or via a flow-inflating bag with 100% oxygen and PEEP set to 5–10 cmH2O. It was not noted whether oxygen was provided via the lungs for the remaining two apnea tests.
Adjustments were made to the ECMO circuit during 13/14 apnea tests to maximize the efficiency of testing and to mitigate complications. Sweep gases were decreased at the start of ten apnea tests to permit a rise in PaCO2. During three apnea tests, carbon dioxide was added to the ECMO circuit to promote a rise in PaCO2, including during two of the tests during which sweep gases were not decreased. ECMO blender FiO2 was increased during seven apnea tests to ensure adequate oxygenation. ECMO flows were increased in two cases, from 34.8 to 36.7 mL/kg/min in one case and from 84.2 to 87.5 mL/kg/min in another case, to correct for development of hypotension. The median nadir SpO2 during apnea testing was 99.5% (IQR 96.8–100%). In two cases, an oxygen saturation of less than 85% was recorded. In neither case was the patient hypoxemic based on blood gas analysis, nor was either patient hypotensive during apnea testing. Blood gases obtained at the conclusion of apnea testing revealed a median pH of 7.2 (IQR 7.18–7.21) with median PaCO2 71.6 (IQR 68.7–80.5) torr and median PaO2 342 (IQR 105–449.3) torr. In one case, the final blood gas could not be retrieved from the electronic medical record; however, the brain death note described a final PaCO2 ≥ 20 torr above baseline and ≥ 60 torr. It is possible that bedside arterial blood gas analyses were obtained and used but were not entered into the electronic medical record.
Discussion
We found that determination of brain death could be made in pediatric patients on ECMO. In the majority of examinations (n = 13/14), the ECMO circuit was modified during apnea testing. The sweep flow was decreased prior to apnea testing in ten examinations, carbon dioxide was added to the circuit during three examinations, and ECMO pump flows were increased in response to hypotension during two examinations.
As reported previously [11,12,13,14, 16,17,18,19] and demonstrated in our cohort of pediatric patients, decreasing the sweep gas flow rate can serve as an effective means of increasing carbon dioxide to a level sufficient for successful apnea testing. In a subset of patients, however, decreasing the sweep gas flow rate may be insufficient to permit an adequate rise in PaCO2 as PaCO2 also depends on the rate of blood flow through the ECMO circuit, intrinsic cardiac output, the degree of lung injury, and the metabolic rate. Furthermore, decreasing the sweep gas flow rate may contribute to hypoxemia. In such cases, the ECMO circuit can be used to introduce carbon dioxide into the blood prior to its return to the arterial circulation. This approach has been described previously in a single adult patient [15] and was utilized during three of the apnea tests in our cohort. In one patient, sweep gas flow rates were held constant during both apnea tests and carbon dioxide was added to the blood flowing through the circuit. In another case, the sweep gas flow rate was decreased and the carbon dioxide sweep was increased. Of note, a subset of the apnea tests in our cohort took a prolonged period of time, consistent with prior reports in pediatric patients [19]. The addition of carbon dioxide to the blood flowing through the circuit may allow for a faster rise in PaCO2, thereby decreasing the duration of apnea testing and mitigating potential complications related to hypoxemia. Although not seen in our cohort, administering carbon dioxide through the ECMO circuit may precipitate hypotension given that carbon dioxide is a direct vasodilator.
Two of the patients in our series developed hypotension during apnea testing, unrelated to the addition of carbon dioxide to the ECMO circuit. Hemodynamic instability is a known potential complication of apnea testing and can impact the ability to successfully complete apnea testing, regardless of whether a patient is supported by ECMO. In both of the patients who experienced hypotension during apnea testing in our cohort, minor adjustments to the ECMO flow were sufficient to rapidly correct the hemodynamic instability. While this has been proposed as a means of supporting the circulation during apnea testing on ECMO, to our knowledge, this has not been previously reported. Giani et al. [17] reported a need for fluid boluses and/or vasoactive drug therapy during 13% of apnea tests performed on 169 patients, including 25 on VA-ECMO; ECMO flows were not adjusted in the subset of patients with hypotension on ECMO. Jarrah et al. [19] also described refractory hypotension in a pediatric patient undergoing apnea testing on VA-ECMO; again, ECMO flows were not adjusted to correct for hypotension.
Two of the patients in our series had recorded oxygen saturations of less than 85% during apnea testing. Neither patient was hypoxemic based on blood gas analysis. In fact, in one patient the PaO2 increased during apnea testing, concomitant with an increase in the ECMO blender FiO2, while in the other patient, the PaO2 decreased minimally during apnea testing despite an increase in the ECMO blender FiO2. Neither patient developed hypotension during apnea testing. Given that apnea testing was successfully completed in these children, it is possible that these were transient decreases in SpO2 that corrected either spontaneously or with adjustments to the ECMO circuit. Finally, it is possible that the SpO2 recordings in these children were unreliable due to peripheral vasoconstriction and a lack of adequate pulsatile flow or to technical issues related to the pulse oximeter. Given the retrospective nature of our study, it is impossible to distinguish between these possibilities.
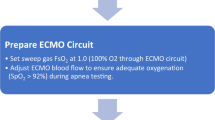
Based on previously reported cases and our experience with brain death testing in patients supported by ECMO, we propose a technique for apnea testing in pediatric patients supported by ECMO as detailed in Fig. 1. Consideration can be given to pre-oxygenation with 100% FiO2 followed by use of a self- or flow-inflating bag or a T-piece oxygen delivery system, as is standard for apnea testing regardless of whether or not a patient is supported by ECMO. Given that oxygen is provided by the ECMO circuit, this may only be necessary in patients with low ECMO flows at risk of intrapulmonary shunting. We then recommend decreasing sweep gas flow rates to allow for a rise in PaCO2. In cases in which the rise in PaCO2 is prolonged or in which concerns related to the potential development of hypoxemia limit the duration of apnea testing, carbon dioxide can be added to the circuit to safely promote a more rapid rise in PaCO2. In cases in which hemodynamic instability develops despite the above measures, the ECMO flow rate can be increased slightly to offset any decrease in blood pressure.
It is of note that in the six patients who met criteria for brain death, the results of the first and second brain death examinations did not differ. Given the high risk of thrombotic, hemorrhagic, and other complications associated with ECMO use, it is worth considering whether a shortened interval with concomitant ancillary testing should be encouraged in pediatric patients supported by ECMO.
Although we describe the largest series of apnea testing in pediatric patients supported by ECMO, our study remains limited by the small number of patients in our cohort. Our study is also limited by the retrospective nature of our study design. Although cases were collected prospectively, the retrospective nature of our data review meant that not all data points were available for every patient in our cohort. Moreover, all of our data come from a single center and may not be generalizable to other pediatric centers.
Conclusions
The clinical determination of brain death for patients supported by ECMO is technically challenging. We show here that clinical determination of brain death, including apnea testing, can be performed in pediatric patients supported by ECMO. We also present a technique for apnea testing that allows for adequate oxygenation, hemodynamic stability, and a sufficient rise in PaCO2, thereby enabling the safe and effective diagnosis of brain death in children supported by VA-ECMO.
References
Barrett CS, Bratton SL, Salvin JW, Laussen PC, Rycus PT, Thiagarajan RR. Neurological injury after extracorporeal membrane oxygenation use to aid pediatric cardiopulmonary resuscitation. Pediatr Crit Care Med. 2009;10:445–51.
Polimenakos AC, Wojtyla P, Smith PJ, et al. Post-cardiotomy extracorporeal cardiopulmonary resuscitation in neonates with complex single ventricle: analysis of outcomes. Eur J Cardiothorac Surg. 2011;40:1396–405.
Sivarajan VB, Best D, Brizard CP, Shekerdemian LS, d’Udekem Y, Butt W. Duration of resuscitation prior to rescue extracorporeal membrane oxygenation impacts outcome in children with heart disease. Intensive Care Med. 2011;37:853–60.
Joffe AR, Lequier L, Robertson CM. Pediatric outcomes after extracorporeal membrane oxygenation for cardiac disease and for cardiac arrest: a review. ASAIO J. 2012;58:297–310.
McMullan DM, Thiagarajan RR, Smith KM, Rycus PT, Brogan TV. Extracorporeal cardiopulmonary resuscitation outcomes in term and premature neonates. Pediatr Crit Care Med. 2014;15:e9–16.
Garcia Guerra G, Zorzela L, Robertson CM, et al. Survival and neurocognitive outcomes in pediatric extracorporeal-cardiopulmonary resuscitation. Resuscitation. 2015;96:208–13.
Thiagarajan RR, Brogan TV, Scheurer MA, Laussen PC, Rycus PT, Bratton SL. Extracorporeal membrane oxygenation to support cardiopulmonary resuscitation in adults. Ann Thorac Surg. 2009;87:778–85.
Extracorporeal Life Support Organization. ECLS registry report: international summary. https://www.elso.org/Portals/0/Files/Reports/2017/International%20Summary%20January%202017.pdf. Accessed 14 Aug 2018.
Rollins MD, Hubbard A, Zabrocki L, Barnhart DC, Bratton SL. Extracorporeal membrane oxygenation cannulation trends for pediatric respiratory failure and central nervous system injury. J Pediatr Surg. 2012;47:68–75.
Muralidharan R, Mateen FJ, Shinohara RT, Schears GJ, Wijdicks EF. The challenges with brain death determination in adult patients on extracorporeal membrane oxygenation. Neurocrit Care. 2011;14:423–6.
Goswami S, Evans A, Das B, Prager K, Sladen RN, Wagener G. Determination of brain death by apnea test adapted to extracorporeal cardiopulmonary resuscitation. J Cardiothorac Vasc Anesth. 2013;27:312–4.
Smilevitch P, Lonjaret L, Fourcade O, Geeraerts T. Apnea test for brain death determination in a patient on extracorporeal membrane oxygenation. Neurocrit Care. 2013;19:215–7.
Hoskote SS, Fugate JE, Wijdicks EF. Performance of an apnea test for brain death determination in a patient receiving venoarterial extracorporeal membrane oxygenation. J Cardiothorac Vasc Anesth. 2014;28:1027–9.
Iannuzzi M, Marra A, De Robertis E, Servillo G. Apnea test for brain death diagnosis in a patient on extracorporeal membrane oxygenation. J Anesth Crit Care Open Access. 2014;1:00020.
Pirat A, Komurcu O, Yener G, Arslan G. Apnea testing for diagnosing brain death during extracorporeal membrane oxygenation. J Cardiothorac Vasc Anesth. 2014;28:e8–9.
Shah V, Lazaridis C. Apnea testing on extracorporeal membrane oxygenation: case report and literature review. J Crit Care. 2015;30:784–6.
Giani M, Scaravilli V, Colombo SM, et al. Apnea test during brain death assessment in mechanically ventilated and ECMO patients. Intensive Care Med. 2016;42:72–81.
Talahma M, Degeorgia M. Apnea testing for the determination of brain death in patients supported by extracorporeal membrane oxygenation. J Neurol Res. 2016;6:28–34.
Jarrah RJ, Ajizian SJ, Agarwal S, Copus SC, Nakagawa TA. Developing a standard method for apnea testing in the determination of brain death for patients on extracorporeal membrane oxygenation: a pediatric case series. Pediatr Crit Care Med. 2014;15:e38–43.
Nakagawa TA, Ashwal S, Mathur M, et al. Guidelines for the determination of brain death in infants and children: an update of the 1987 task force recommendations. Crit Care Med. 2011;39:2139–55.
Haque IU, Zaritsky AL. Analysis of the evidence for the lower limit of systolic and mean arterial pressure in children. Ped Crit Care Med. 2007;8:138–44.
Funding
The study was carried out without financial support.
Author information
Authors and Affiliations
Contributions
DBH made substantial contributions to conception and design, acquisition of data, and analysis and interpretation of data; drafting the article and revising of article for important intellectual content; and final approval of the version to be published. VK made substantial contributions to conception and design and acquisition of data; drafting the article; and final approval of the version to be published. NPD and JTB III made substantial contributions to conception and design; revising of article for important intellectual content; and final approval of the version to be published. JLC made substantial contributions to conception and design, acquisition of data, and analysis and interpretation of data; drafting the article and revising of article for important intellectual content; and final approval of the version to be published. Authorship requirements have been met, and the final manuscript was approved by all authors. The manuscript has not been published elsewhere and is not under consideration by another journal.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have potential conflict of interest.
Ethical Approval/Informed Consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Research Ethics Board of Children’s National Medical Center and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Consent was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Figure 1
Children’s National Medical Center brain death checklist (DOC 82 kb)
Rights and permissions
About this article
Cite this article
Harrar, D.B., Kukreti, V., Dean, N.P. et al. Clinical Determination of Brain Death in Children Supported by Extracorporeal Membrane Oxygenation. Neurocrit Care 31, 304–311 (2019). https://doi.org/10.1007/s12028-019-00700-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-019-00700-z