Abstract
Background
Traumatic brain injury (TBI) causes substantial morbidity and mortality in US children. Post-traumatic seizures (PTS) occur in 11–42% of children with severe TBI and are associated with unfavorable outcome. Electroencephalographic (EEG) monitoring may be used to detect PTS and antiepileptic drugs (AEDs) may be used to treat PTS, but national rates of EEG and AED use are not known. The purpose of this study was to describe the frequency and timing of EEG and AED use in children hospitalized after severe TBI.
Methods
Retrospective cohort study of 2165 children at 30 hospitals in a probabilistically linked dataset from the National Trauma Data Bank (NTDB) and the Pediatric Health Information Systems (PHIS) database, 2007–2010. We included children (age <18 years old at admission) with linked NTDB and PHIS records, severe (Emergency Department [ED] Glasgow Coma Scale [GCS] <8) TBI, hospital length of stay >24 h, and non-missing disposition. The primary outcomes were EEG and AED use.
Results
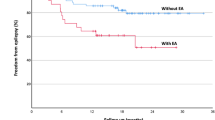
Overall, 31.8% of the cohort had EEG monitoring. Of those, 21.8% were monitored on the first hospital day. The median duration of EEG monitoring was 2.0 (IQR 1.0, 4.0) days. AEDs were prescribed to 52.0% of the cohort, of whom 61.8% received an AED on the first hospital day. The median duration of AED use was 8.0 (IQR 4.0, 17.0) days. EEG monitoring and AED use were more frequent in children with known risk factors for PTS. EEG monitoring and AED use were not related to hospital TBI volume.
Conclusion
EEG use is relatively uncommon in children with severe TBI, but AEDs are frequently prescribed. EEG monitoring and AED use are more common in children with known risk factors for PTS.



Similar content being viewed by others
References
Langlois JA, Rutland-Brown W, Thomas KE. The incidence of traumatic brain injury among children in the united states: differences by race. J Head Trauma Rehabil. 2005;20:229–38.
Faul M, Likang X, Wald M, Coronado V. Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths 2002–2006. Atlanta (GA): National Center for Injury Prevention; Control, Centers for Disease Control; Prevention, U.S. Department of Health; Human Services; 2010. https://www.cdc.gov/traumaticbraininjury/pdf/blue_book.pdf.
Shaklai S, Peretz R, Spasser R, Simantov M, Groswasser Z. Long-term functional outcome after moderate-to-severe paediatric traumatic brain injury. Brain Inj. 2014;28:915–21.
Chiaretti A, Piastra M, Pulitanò S, Pietrini D, De Rosa G, Barbaro R, et al. Prognostic factors and outcome of children with severe head injury: an 8-year experience. Childs Nerv Syst. 2002;18:129–36.
Arndt DH, Lerner JT, Matsumoto JH, Madikians A, Yudovin S, Valino H, et al. Subclinical early posttraumatic seizures detected by continuous eEG monitoring in a consecutive pediatric cohort. Epilepsia. 2013;54:1780–8.
Liesemer K, Bratton SL, Zebrack CM, Brockmeyer D, Statler KD. Early post-traumatic seizures in moderate to severe pediatric traumatic brain injury: rates, risk factors, and clinical features. J Neurotrauma. 2011;28:755–62.
Emanuelson I, Uvebrant P. Occurrence of epilepsy during the first 10 years after traumatic brain injury acquired in childhood up to the age of 18 years in the south western swedish population-based series. Brain Inj. 2009;23:612–6.
Arndt DH, Goodkin HP, Giza CC. Early posttraumatic seizures in the pediatric population. J Child Neurol. 2016;31:46–56.
Ostahowski PJ, Kannan N, Wainwright MS, Qiu Q, Mink RB, Groner JI, et al. Variation in seizure prophylaxis in severe pediatric traumatic brain injury. J Neurosurg Pediatr. 2016;3:1–8.
Kurz JE, Poloyac SM, Abend NS, Fabio A, Bell MJ, Wainwright MS, et al. Variation in anticonvulsant selection and electroencephalographic monitoring following severe traumatic brain injury in children-understanding resource availability in sites participating in a comparative effectiveness study. Pediatr Crit Care Med. 2016;17:649–57.
Bennett TD, Riva-Cambrin J, Keenan HT, Korgenski EK, Bratton SL. Variation in intracranial pressure monitoring and outcomes in pediatric traumatic brain injury. Arch Pediatr Adolesc Med. 2012;166:641–7.
Bennett TD, Statler KD, Korgenski EK, Bratton SL. Osmolar therapy in pediatric traumatic brain injury. Crit Care Med. 2012;40:208–15.
Dean NP, Boslaugh S, Adelson PD, Pineda JA, Leonard JR. Physician agreement with evidence-based recommendations for the treatment of severe traumatic brain injury in children. J Neurosurg. 2007;107:387–91.
Van Cleve W, Kernic MA, Ellenbogen RG, Wang J, Zatzick DF, Bell MJ, et al.: National variability in intracranial pressure monitoring and craniotomy for children with moderate to severe traumatic brain injury. Neurosurgery 2013; 73:746–52; discussion 752; quiz 752.
Bennett TD, Dean JM, Keenan HT, McGlincy MH, Thomas AM, Cook LJ. Linked records of children with traumatic brain injury. probabilistic linkage without use of protected health information. Methods Inf Med. 2015;54:328–37.
American College of Surgeons Committee on Trauma: National Trauma Data Bank Research Data Set user manual, admission year 2009. Chicago, IL.
Gerber JS, Newland JG, Coffin SE, Hall M, Thurm C, Prasad PA, et al. Variability in antibiotic use at children’s hospitals. Pediatrics. 2010;126:1067–73.
Bratton SL, Newth CJ, Zuppa AF, Moler FW, Meert KL, Berg RA, et al. Critical care for pediatric asthma: wide care variability and challenges for study. Pediatr Crit Care Med. 2012;13:407–14.
Conway PH, Keren R. Factors associated with variability in outcomes for children hospitalized with urinary tract infection. J Pediatr. 2009;154:789–96.
Slonim AD, Khandelwal S, He J, Hall M, Stockwell DC, Turenne WM, et al. Characteristics associated with pediatric inpatient death. Pediatrics. 2010;125:1208–16.
Kee VR, Gilchrist B, Granner MA, Sarrazin NR, Carnahan RM. A systematic review of validated methods for identifying seizures, convulsions, or epilepsy using administrative and claims data. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 1):183–93.
Bennett KS, DeWitt PE, Harlaar N, Bennett TD. Seizures in children with severe traumatic brain injury. Pediatr Crit Care Med. 2016. doi:10.1097/PCC.0000000000000948.
Tri-Analytics Inc. and The Johns Hopkins University: ICDMAP-90 software user’s guide. 1997.
Centers for Disease Control and Prevention: Recommended framework for presenting injury mortality data. MMWR 1997; 46.
Barell V, Aharonson-Daniel L, Fingerhut LA, Mackenzie EJ, Ziv A, Boyko V, et al. An introduction to the barell body region by nature of injury diagnosis matrix. Inj Prev. 2002;8:91–6.
Ong LC, Dhillon MK, Selladurai BM, Maimunah A, Lye MS. Early post-traumatic seizures in children: clinical and radiological aspects of injury. J Paediatr Child Health. 1996;32:173–6.
Ratan SK, Kulshreshtha R, Pandey RM. Predictors of posttraumatic convulsions in head-injured children. Pediatr Neurosurg. 1999;30:127–31.
Core R. Team: R: a language and environment for statistical computing. Vienna: R Foundation for Statistical, Computing; 2014.
Halekoh U, Højsgaard S, Yan J. The r package geepack for generalized estimating equations. J Stat Softw. 2006;15:1–11.
Therneau TM. Survival: a package for survival analysis in R. https://cran.r-project.org/web/packages/survival/survival.pdf. Accessed 18 Nov 2016.
Chiaretti A, De Benedictis R, Polidori G, Piastra M, Iannelli A, Di Rocco C. Early post-traumatic seizures in children with head injury. Childs Nerv Syst. 2000;16:862–6.
Arango JI, Deibert CP, Brown D, Bell M, Dvorchik I, Adelson PD. Posttraumatic seizures in children with severe traumatic brain injury. Childs Nerv Syst. 2012;28:1925–9.
Ateş O, Ondül S, Onal C, Büyükkiraz M, Somay H, Cayli SR, et al. Post-traumatic early epilepsy in pediatric age group with emphasis on influential factors. Childs Nerv Syst. 2006;22:279–84.
Goldstein JL, Leonhardt D, Kmytyuk N, Kim F, Wang D, Wainwright MS. Abnormal neuroimaging is associated with early in-hospital seizures in pediatric abusive head trauma. Neurocrit Care. 2011;15:63–9.
Barlow KM, Spowart JJ, Minns RA. Early posttraumatic seizures in non-accidental head injury: relation to outcome. Dev Med Child Neurol. 2000;42:591–4.
O’Neill BR, Handler MH, Tong S, Chapman KE. Incidence of seizures on continuous EEG monitoring following traumatic brain injury in children. J Neurosurg Pediatr. 2015;16:167–76.
Herman ST, Abend NS, Bleck TP, Chapman KE, Drislane FW, Emerson RG, et al. Consensus statement on continuous eEG in critically ill adults and children, part I: indications. J Clin Neurophysiol. 2015;32:87–95.
Adelson PD, Bratton SL, Carney NA, Chesnut RM, Coudray HE du, Goldstein B, et al.: Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents. Chapter 19. The role of anti-seizure prophylaxis following severe pediatric traumatic brain injury. Pediatr Crit Care Med 2003; 4:S72–5.
Kochanek PM, Carney N, Adelson PD, Ashwal S, Bell MJ, Bratton S, et al. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents–second edition. Pediatr Crit Care Med. 2012;13(Suppl 1):S1–82.
Sundararajan K, Milne D, Edwards S, Chapman MJ, Shakib S. Anti-seizure prophylaxis in critically ill patients with traumatic brain injury in an intensive care unit. Anaesth Intensive Care. 2015;43:646–51.
Kaindl AM, Asimiadou S, Manthey D, Hagen MVD, Turski L, Ikonomidou C. Antiepileptic drugs and the developing brain. Cell Mol Life Sci. 2006;63:399–413.
Olney JW, Young C, Wozniak DF, Jevtovic-Todorovic V, Ikonomidou C. Do pediatric drugs cause developing neurons to commit suicide? Trends Pharmacol Sci. 2004;25:135–9.
Kruer RM, Harris LH, Goodwin H, Kornbluth J, Thomas KP, Slater LA, et al.: Changing trends in the use of seizure prophylaxis after traumatic brain injury: a shift from phenytoin to levetiracetam. J Crit Care 2013; 28:883.e9–883.13.
Browning M, Shear DA, Bramlett HM, Dixon CE, Mondello S, Schmid KE, et al. Levetiracetam treatment in traumatic brain injury: operation brain trauma therapy. J Neurotrauma. 2016;33:581–94.
Szaflarski JP, Sangha KS, Lindsell CJ, Shutter LA. Prospective, randomized, single-blinded comparative trial of intravenous levetiracetam versus phenytoin for seizure prophylaxis. Neurocrit Care. 2010;12:165–72.
Acknowledgements
This work was supported by the Eunice Kennedy Shriver National Institute for Child Health and Human Development at the National Institutes of Health (Grant K23HD074620 to TB).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ruzas, C.M., DeWitt, P.E., Bennett, K.S. et al. EEG Monitoring and Antiepileptic Drugs in Children with Severe TBI. Neurocrit Care 26, 256–266 (2017). https://doi.org/10.1007/s12028-016-0329-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-016-0329-8