Abstract
Background
Perihematomal edema (PHE) expansion rate may predict functional outcome following spontaneous intracerebral hemorrhage (ICH). We hypothesized that the effect of PHE expansion rate on outcome is greater for deep versus lobar ICH.
Methods
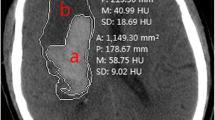
Subjects (n = 115) were retrospectively identified from a prospective ICH cohort enrolled from 2000 to 2013. Inclusion criteria were age ≥ 18 years, spontaneous supratentorial ICH, and known onset time. Exclusion criteria were primary intraventricular hemorrhage (IVH), trauma, subsequent surgery, or warfarin-related ICH. ICH and PHE volumes were measured from CT scans and used to calculate expansion rates. Logistic regression assessed the association between PHE expansion rates and 90-day mortality or poor functional outcome (modified Rankin Scale > 2). Odds ratios are per 0.04 mL/h.
Results
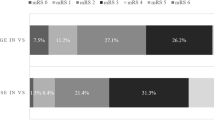
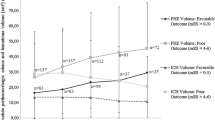
PHE expansion rate from baseline to 24 h (PHE24) was associated with mortality for deep (p = 0.03, OR 1.13[1.02–1.26]) and lobar ICH (p = 0.02, OR 1.03[1.00–1.06]) in unadjusted regression and in models adjusted for age (deep p = 0.02, OR 1.15[1.02–1.28]; lobar p = 0.03, OR 1.03[1.00–1.06]), Glasgow Coma Scale (deep p = 0.03, OR 1.13[1.01–1.27]; lobar p = 0.02, OR 1.03[1.01–1.06]), or time to baseline CT (deep p = 0.046, OR 1.12[1.00–1.25]; lobar p = 0.047, OR 1.03[1.00–1.06]). PHE expansion rate from baseline to 72 h (PHE72) was associated with mRS > 2 for deep ICH in models that were unadjusted (p = 0.02, OR 4.04[1.25–13.04]) or adjusted for ICH volume (p = 0.02, OR 4.3[1.25–14.98]), age (p = 0.03, OR 5.4[1.21–24.11]), GCS (p = 0.02, OR 4.19[1.2–14.55]), or time to first CT (p = 0.03, OR 4.02[1.19–13.56]).
Conclusions
PHE72 was associated with poor functional outcomes after deep ICH, whereas PHE24 was associated with mortality for deep and lobar ICH.
Similar content being viewed by others
References
Qureshi AI, Mendelow AD, Hanley DF. Intracerebral haemorrhage. Lancet. 2009;373(9675):1632–44.
van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol. 2010;9(2):167–76.
Broderick J, Connolly S, Feldmann E, et al. Guidelines for the management of spontaneous intracerebral hemorrhage in adults 2007 update: a guideline from the American Heart Association/American Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group. Stroke. 2007;38(6):2001–23.
Keep RF, Hua Y, Xi G. Intracerebral haemorrhage: mechanisms of injury and therapeutic targets. Lancet Neurol. 2012;11(8):720–31.
Parry-Jones AR, Wang X, Sato S, et al. Edema extension distance outcome measure for phase II clinical trials targeting edema after intracerebral hemorrhage. Stroke. 2015;46(6):e137–40.
Selim M, Sheth KN. Perihematoma edema: A potential translational target in intracerebral hemorrhage? Transl Stroke Res. 2015;6(2):104–6.
Urday S, Kimberly WT, Beslow LA, et al. Targeting secondary injury in intracerebral haemorrhage—perihaematomal oedema. Nat Rev Neurol. 2015;11(2):111–22.
Arima H, Wang JG, Huang Y, et al. Significance of perihematomal edema in acute intracerebral hemorrhage The INTERACT trial. Neurology. 2009;73(23):1963–8.
Balami JS, Buchan AM. Complications of intracerebral haemorrhage. Lancet Neurol. 2012;11(1):101–18.
Urday S, Beslow LA, Goldstein DW, et al. Measurement of perihematomal edema in intracerebral hemorrhage. Stroke. 2015;46(4):1116–9.
Urday S, Beslow LA, Dai F, et al. Rate of perihematomal edema expansion predicts outcome after intracerebral hemorrhage. Crit Care Med. 2016;44(4):790–7.
Rost NS, Smith EE, Chang Y, et al. Prediction of functional outcome in patients with primary intracerebral hemorrhage the FUNC score. Stroke. 2008;39(8):2304–9.
Sreekrishnan A, Dearborn JL, Greer DM, et al. Intracerebral hemorrhage location and functional outcomes of patients: a systematic literature review and meta-analysis. Neurocrit Care. 2016;1–8. doi:10.1007/s12028-016-0276-4.
Simard JM, Kent TA, Chen M, Tarasov KV, Gerzanich V. Brain oedema in focal ischaemia: molecular pathophysiology and theoretical implications. Lancet Neurol. 2007;6(3):258–68.
Qureshi W, Soliman EZ, Solomon SD, et al. Risk factors for atrial fibrillation in patients with normal versus dilated left atria (from the Atherosclerosis Risk in Communities [ARIC] study). Am J Cardiol. 2014;114(9):1368–72.
Hammond F, Malec J, Buschbacher R, Nick T. Handbook for clinical research: design, statistics, and implementation. New York, NY: Demos Medical Publishing; 2015.
Broderick JP, Brott TG, Duldner JE, Tomsick T, Huster G. Volume of intracerebral hemorrhage. A powerful and easy-to-use predictor of 30-day mortality. Stroke. 1993;24(7):987–93.
Davis SM, Broderick J, Hennerici M, et al. Hematoma growth is a determinant of mortality and poor outcome after intracerebral hemorrhage. Neurology. 2006;66(8):1175–81.
Dowlatshahi D, Demchuk AM, Flaherty ML, Ali M, Lyden PL, Smith EE. Defining hematoma expansion in intracerebral hemorrhage: relationship with patient outcomes. Neurology. 2011;76(14):1238–44.
Flaherty ML, Haverbusch M, Sekar P, et al. Long-term mortality after intracerebral hemorrhage. Neurology. 2006;66(8):1182–6.
Falcone GJ, Biffi A, Brouwers H, et al. Predictors of hematoma volume in deep and lobar supratentorial intracerebral hemorrhage. JAMA Neurol. 2013;70(8):988–94.
Xi G, Keep RF, Hoff JT. Pathophysiology of brain edema formation. Neurosurg Clin N Am. 2002;13(3):371–83.
Venkatasubramanian C, Mlynash M, Finley-Caulfield A, et al. Natural history of perihematomal edema following intracerebral hemorrhage measured by serial magnetic resonance imaging. Stroke J Cereb Circ. 2011;42(1):73–80.
McCarron MO, McCarron P, Alberts MJ. Location characteristics of early perihaematomal oedema. J Neurol Neurosurg Psychiatry. 2006;77(3):378–80.
Hallevi H, Dar NS, Barreto AD, et al. The IVH Score: a novel tool for estimating intraventricular hemorrhage volume: clinical and research implications. Crit Care Med. 2009;37(3):969.
Vemmos KN, Tsivgoulis G, Spengos K, et al. Association between 24-h blood pressure monitoring variables and brain oedema in patients with hyperacute stroke. J Hypertens. 2003;21(11):2167–73.
Nakamura T, Keep RF, Hua Y, Hoff JT, Xi G. Oxidative DNA injury after experimental intracerebral hemorrhage. Brain Res. 2005;1039(1–2):30–6.
Wang X, Michaelis EK. Selective neuronal vulnerability to oxidative stress in the brain. Front Aging Neurosci. 2010;2(12):12–25.
Thrane AS, Thrane VR, Nedergaard M. Drowning stars: reassessing the role of astrocytes in brain edema. Trends Neurosci. 2014;37(11):620–8.
Kahle KT, Staley KJ, Nahed BV, et al. Roles of the cation–chloride cotransporters in neurological disease. Nat Clin Pract Neurol. 2008;4(9):490–503.
Mayer SA, Brun NC, Begtrup K, et al. Efficacy and safety of recombinant activated factor VII for acute intracerebral hemorrhage. N Engl J Med. 2008;358(20):2127–37.
Pandey AS, Xi G. Intracerebral hemorrhage: a multimodality approach to improving outcome. Transl Stroke Res. 2014;5(3):313–5.
Murthy SB, Moradiya Y, Dawson J, et al. Perihematomal edema and functional outcomes in intracerebral hemorrhage influence of hematoma volume and location. Stroke. 2015;46(11):3088–92.
Hemphill JC, Bonovich DC, Besmertis L, Manley GT, Johnston SC. The ICH Score a simple, reliable grading scale for intracerebral hemorrhage. Stroke. 2001;32(4):891–7.
Funding
Research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the NIH. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the NIH (Grants T35HL007649 and HL082517; Mr. Grunwald and Dr. Simard). This work was also supported by the NIH (Grants R01AG26484 and 5R01NS059727; Drs. Greenberg and Rosand and Mses. Ayres and Vashkevich), National Institute of Neurological Disorders and Stroke (Grants NS060801 and NS061808, Dr. Simard), and American Heart Association (Grant 16SDG27250236, Dr. Shi).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Grunwald, Z., Beslow, L.A., Urday, S. et al. Perihematomal Edema Expansion Rates and Patient Outcomes in Deep and Lobar Intracerebral Hemorrhage. Neurocrit Care 26, 205–212 (2017). https://doi.org/10.1007/s12028-016-0321-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-016-0321-3