Abstract
Background
Although the incidence of subdural hematoma (SDH) has increased in the US in the last decade, limited prospective data exist examining risk factors for poor outcome.
Methods
A prospective, observational study of consecutive SDH patients was conducted from 7/2008 to 11/2011. Baseline clinical data, hospital and surgical course, complications, and imaging data were compared between those with good versus poor 3-month outcomes (modified Rankin Scores [mRS] 0–3 vs. 4–6). A multivariable logistic regression model was constructed to identify independent predictors of poor outcome.
Results
116 SDH patients (18 acute, 56 mixed acute/subacute/chronic, 42 subacute/chronic) were included. At 3 months, 61 (53 %) patients had good outcomes (mRS 0–3) while 55 (47 %) were severely disabled or dead (mRS 4–6). Of those who underwent surgical evacuation, 54/94 (57 %) had good outcomes compared to 7/22 (32 %) who did not (p = 0.030). Patients with mixed acuity or subacute/chronic SDH had significantly better 3-month mRS with surgery (median mRS 1 versus 5 without surgery, p = 0.002) compared to those with only acute SDH (p = 0.494). In multivariable analysis, premorbid mRS, age, admission Glasgow Coma Score, history of smoking, and fever were independent predictors of poor 3-month outcome (all p < 0.05; area under the curve 0.90), while SDH evacuation tended to improve outcomes (adjusted OR 3.90, 95 % CI 0.96–18.9, p = 0.057).
Conclusions
Nearly 50 % of SDH patients were dead or moderate-severely disabled at 3 months. Older age, poor baseline, poor admission neurological status, history of smoking, and fever during hospitalization predicted poor outcomes, while surgical evacuation was associated with improved outcomes among those with mixed acuity or chronic/subacute SDH.
Similar content being viewed by others
Introduction
Subdural hematoma (SDH) represents a common form of intracranial bleeding that is increasing in prevalence and cost across the US [1]. The mortality rates associated with SDH range from 30 to 50 % depending on the acuity of the blood and patient comorbidities [2–6]. Between 1993 and 2007, nationwide, the number of hospital admissions and average cost per admission for SDH increased by 39 and 60 %, respectively, although in-hospital mortality over that period decreased from 15 to 12 % [1].
Despite the increasing utilization of healthcare resources and decreasing mortality, it remains less clear whether functional recovery has improved over the last decade [7]. There is a paucity of data examining the influence of baseline clinical characteristics and events of hospitalization on long-term functional recovery. This prospective, observational study was therefore conducted to identify independent predictors of poor 3-month functional outcome in a SDH population.
Methods
Study Population
A prospective study of consecutive SDH patients presenting to a tertiary, level II trauma center Neuroscience Intensive Care Unit between July 2008 and November 2011 was conducted. Criteria for inclusion in the study were defined as follows: aged ≥18 years, diagnosis of SDH based on admission CT scan data, and consent to participate in 3-month follow-up interviews. Patients without follow-up data available or those who underwent withdrawal of life-sustaining therapy during hospitalization were subsequently excluded from analysis. The study was approved by the local Institutional Review Board (IRB). All patients or their surrogates were consented for participation in this study.
Routine Clinical Care
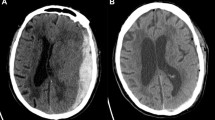
All patients underwent admission head CT and a follow-up stability scan 6 h after the initial head CT. An immediate postoperative head CT was performed on all patients who underwent SDH evacuation. The decision to pursue surgical intervention, and the type of surgery performed, was made by the neurosurgical team after assessing the patient’s clinical and radiographic findings and consulting with the family. Surgical intervention was guided by the Brain Trauma Foundation guidelines for SDH management [7–9]. Subdural evacuation was indicated in patients with SDH >10 mm in thickness or midline shift >5 mm on head CT, regardless of Glasgow Coma Score (GCS). Comatose patients who did not meet these radiographic parameters, but who experienced a GCS deterioration of ≥2 points or who presented with asymmetric or fixed and dilated pupils, or had an ICP ≥20 mmHg also were considered for surgical intervention. Patients with acute SDH routinely underwent craniotomy or craniectomy if surgery was indicated, while those with chronic SDH typically underwent burr hole drainage. Patients with subacute or mixed subacute and chronic SDH underwent burr hole or craniotomy at the discretion of the treating neurosurgeon. All patients who underwent craniotomy or burr hole drainage had a drain left in place postoperatively, which was removed at the discretion of the neurosurgical team. Bedside SDH drainage was not performed. All patients received prophylactic antiepileptics for 7 days following SDH onset or for 7 days following craniotomy (whichever was longer). Patients with clinical or radiographic evidence of elevated intracranial pressure (ICP) routinely received osmotic therapy and ICP monitoring.
Patient Assessments
Admission demographic data, including medical history and premorbid functional status, were collected from the patient or surrogate upon admission. Admission clinical status was assessed using the GCS [10], National Institute of Health Stroke Scale (NIHSS) [11], and Acute Physiology and Chronic Health Evaluation II Acute Physiology Score (APACHE II APS) [12]. Premorbid functional status was assessed using the modified Rankin scale (mRS) [13] and Barthel Index [14]. Admission CT scans were assessed by one of the two neurointensivists (EG, JF) for the following: SDH location, maximum SDH thickness, SDH volume [15], chronicity of blood (categorized as 1-acute blood only; 2-mixed acute, subacute, and/or chronic blood; or 3-subacute and/or chronic blood without any acute blood component), midline shift, and the presence of edema. Details of the hospital course including medical treatments, procedures, and complications were prospectively recorded. SDH reaccumulation was coded in patients who underwent surgery only if there was a radiographic increase in SDH volume comparing the immediate postoperative CT to a subsequent head CT. SDH expansion was coded if there was a radiographic increase in SDH volume on follow-up head CT. The primary functional outcome was the modified Rankin Score at 3 months, dichotomized as good (mRS 0–3) versus poor (mRS 4–6). The Barthel Index of independent activities of daily living was also assessed as a secondary functional outcome measure. The Barthel Index was not scored in patients who died.
Statistical Analyses
Baseline demographic data, admission clinical status, radiographic characteristics, surgical characteristics, events of hospitalization, and medical complications were compared between patients with good (mRS 0–3) versus poor (mRS 4–6) outcome using either the chi square or Mann–Whitney U tests. Barthel scores were dichotomized at the median and assessed as good (Barthel Index >95) versus poor (Barthel Index ≤95). All statistically significant univariate variables (p < 0.05) were included in a forward, stepwise multivariable logistic regression model to identify independent predictors of poor functional outcome. SDH acuity (acute blood present versus absent on admission CT), admission GCS, and surgical evacuation were forced into the model as variables identified a priori as predictors of outcome. When a high degree of collinearity between variables existed (correlation >0.8), only one variable was selected for inclusion in the multivariable model. A p value less than 0.05 was considered significant. Analysis was conducted using SPSS v21 and JMP Pro10 software.
Results
Over the study period, 134 SDH patients were enrolled and 116 patients were eligible for analysis following the exclusion of eight patients (6.0 %) for loss of follow-up and 10 patients (7.5 %) who underwent withdrawal of life-sustaining therapy during hospitalization. The median age was 74 years (range 25–96) and 55 % were male. Of 116 patients, 18 (16 %) had acute SDH only; 56 (48 %) had mixed acute, subacute, and/or chronic SDH; and 42 (36 %) had subacute and/or chronic SDH without any acute hemorrhage component. Bilateral SDH occurred in 50 (43 %) patients and the median SDH volume was 113 ml (range 1–263 mL). Surgical SDH evacuation was performed in 94 (81 %) patients (75 [80 %] craniotomy, 19 [20 %] burr hole). Surgery was more likely to occur in patients with better admission neurological and physiological status; however, surgery was also more common in those with more severe radiographic features including higher SDH volume and greater midline shift (Table 1). The median number of surgeries was 1 (range 0–4). The final follow-up CT was obtained in a median of 23 days (range 1–147) from the postoperative scan or from the admission head CT (if no surgery was performed). The median percent reduction in SDH volume from the admission head CT to the final postoperative head CT was 60 % (range 0–100 %) in those who underwent SDH evacuation, while the median spontaneous percent reduction in SDH volume without surgery was 10 % (range 0–100). Postoperative reaccumulation of SDH occurred in 56 of 94 (60 %) patients and re-evacuation occurred in 7 of 94 (7 %). The median volume of reaccumulation postoperatively was 8.5 ml (range 0–160.5). Of those who underwent burr hole drainage, 13 of 18 (68 %) had reaccumulation compared to 40 of 75 (53 %) of those who underwent craniotomy (p = 0.244). SDH expansion occurred in 7 of 22 (32 %) of those who did not undergo surgical evacuation.
Excluding those who underwent withdrawal of life-sustaining therapy, in-hospital death occurred in 8 (6.9 %) patients. Sixty-one patients (52.6 %) experienced good 3-month functional outcome (mRS 0–3), while 55 patients (47.4 %) had poor outcomes (mRS 4-6). Overall mortality at 3 months was 22 %, while severe disability (mRS 4–5) was observed in another 26 % of patients. The median Barthel activities of daily living index score at 3 months was 95 (range 0–100). Overall, 12 of 18 (67 %) patients with only acute SDH were dead or severely disabled at 3 months compared to 28 of 56 (50 %) patients with mixed acuity SDH and 15 of 42 (36 %) patients with subacute and/or chronic SDH without any acute component (p = 0.077 across all 3 groups). There was no difference in rates of death or mRS 4-6 between those with mixed acuity or chronic/subacute SDH without an acute component; however, those with only acute SDH were significantly more likely to be dead or severely disabled (mRS 4–6) at 3 months compared to those with subacute/chronic SDH and no acute hemorrhage component (p = 0.027). Similarly, the median 3-month Barthel Index for those with acute-only SDH was 62.5 (range 5–100) compared to 100 (range 0–100) in those with mixed acuity SDH and 100 (range 0–100) in those with subacute and/or chronic SDH (p = 0.398 across all three groups). The association of radiographic SDH acuity with 3-month mortality, mRS, and Barthel Index outcomes is shown in Fig. 1.
Mortality and functional outcome (modified Rankin Score [mRS] and Barthel Index) at 3 months based on the radiographic acuity of subdural hematoma. Poor Barthel Index defined as score below the median value (<95). Asterisk indicates a significant difference for 3-month mRS between the acute-only SDH group and the subacute/chronic SDH group (p = 0.027)
Differences in the baseline demographics, medical history, admission clinical and radiographic characteristics, surgical characteristics, hospital course, and medical complications among those with good versus poor 3-month mRS are reported in Table 2. Older age, a history of smoking, and medical comorbidities including hypertension, diabetes mellitus, kidney disease, anemia, and dementia were significantly associated with poor 3-month mRS outcome in univariate analysis (all p < 0.05). Worse admission neurological, clinical, and premorbid functional status were also associated with poor 3-month mRS outcome scores (all p < 0.05). Conversely, surgical SDH evacuation was associated with good functional outcome.
The median 3-month mRS was 2 (range 0–6) for those who underwent surgery compared to 5 (range 0–6, p = 0.001) for those who did not, and 54 of 94 (57 %) patients who underwent surgery had mRS 0-3 at 3 months compared to 7 of 22 (32 %) who did not (p = 0.030). The median Barthel was 100 (range 0–100) in those who underwent evacuation compared to 85 (range 55–100, p = 0.642) in those who did not. Patients with mixed acuity or subacute/chronic SDH had significantly better 3-month mRS with surgery (median mRS 1 [range 0–6] vs. 5 [range 0–6] without surgery, p = 0.002). There was no significant improvement in outcome with surgery in those with purely acute blood (p = 0.494); however, only 18 patients had acute-only SDH. Figure 2 shows the 3-month mRS for each SDH acuity subtype stratified by those who did or did not undergo surgical SDH evacuation.
Multivariable logistic regression analysis identified five independent predictors of poor 3-month mRS: age, admission GCS, premorbid mRS, fever during hospitalization >38.3 C, and a history of smoking (model receiver operating characteristic area under the curve 0.90, Table 3). Acute blood on admission CT did not independently predict poor functional outcome (p = 0.750), adjusting for other variables. Similarly, surgical evacuation was not significantly associated with better outcome (p = 0.057), adjusting for age, premorbid status, admission neurological status, and SDH acuity, among other factors. The model predicted poor functional outcome with a sensitivity of 88 %, specificity of 75 %, positive predictive value of 74 %, negative predictive value of 88 %, and accuracy of 77 %.
Discussion
This study is one of the first, to our knowledge, to present prospective, long-term, 3-month functional outcomes among consecutive patients with subacute and chronic SDH. Additionally, our study is one of the few to include SDH patients who did not undergo a surgical intervention. This allowed us to observe the association of SDH evacuation on functional outcomes though we cannot make any conclusive statements about the efficacy of surgery, since this was not a randomized trial. A further strength of this study is that our outcomes are not confounded by withdrawal of life-sustaining therapy (since these patients were excluded), which limits the interpretation of other studies assessing mortality as a primary outcome [16, 17]. In a retrospective review of 216 SDH patients at our institution from 2001 to 2008, the in-hospital mortality rate among a similarly diverse group of SDH acuities was 13 % (including those who underwent withdrawal), and poor discharge disposition (to a nursing home, hospice, or subacute rehabilitation center) occurred in 20 % [7]. Prospectively, the observed in-hospital mortality rate of 6.9 % (increasing to 15.5 % if patients undergoing withdrawal of care are included) is consistent with our retrospective data and nationally published rates [1]. Additionally, in the current study, nearly half of all patients with SDH experienced either death (22 %) or severe disability (26 %) at 3 months, excluding those patients for whom life-sustaining therapy was withdrawn or withheld during hospitalization. Others have retrospectively observed poor 3-month outcomes (mRS 3–6) in 28 % of patients with chronic SDH; however, patients with extremely poor baseline mRS scores of five or patients with evidence of subacute or mixed chronicity blood were not enrolled in this study [18]. In a small Chinese cohort study of traumatic SDH, quality of life scores measured 4–7 years after injury revealed lower levels of physical, emotional, and social functioning when compared to population controls [19].
Overall, age, poor premorbid functional status, and poor admission neurological status were independent predictors of poor 3-month functional outcome, along with a history of smoking and fever during hospitalization. Others have also found that age, severity of injury, and admission neurological status are primary factors predicting outcome following traumatic brain injury with acute SDH [2, 20]. Similar predictors appear in a retrospective study of nontraumatic SDH patients [18]. A small, retrospective chart review study identified variables associated with discharge home following “nontraumatic” SDH including GCS score, mRS score, and surgical intervention [21].
Our findings of fever during hospitalization and a history of smoking as independent predictors of poor functional outcome are novel. Fever following subdural hemorrhage is less commonly reported than with other types of intracranial hemorrhage, such as subarachnoid hemorrhage or intracerebral hemorrhage, where fever is associated with worse functional and neurological outcomes [22]. In general, any elevation of brain temperature following cerebral insult has been associated with marked worsening in clinical status in neurocritically ill populations, whether through ischemic or metabolic injury [23] or derangements of intracranial volume homeostasis [24]. Furthermore, fever has been associated with higher mortality rates and longer hospital length of stay among neurocritically ill patients, even after adjusting for other factors [25]. Because body temperature can be controlled with advanced cooling devices, fever may be a modifiable risk factor that warrants further study.
Smoking represents one of the major modifiable risk factors for other types of intracranial hemorrhage [26, 27]. Although the correlation of smoking with worse functional outcome after SDH may be a reflection of the lower health scores often seen with these patients, the fact that it was an independent predictor of outcome in our model may suggest a possible association between smoking and poor recovery after brain injury.
Across all subtypes of SDH, patients undergoing surgical evacuation experienced better 3-month functional outcomes compared to those who did not, although the results were nonsignificant. Stratifying by SDH acuity, however, surgery was associated with improved functional outcome in cases of mixed acuity or subacute/chronic SDH (p = 0.002), while no significant difference was observed in patients with purely acute blood (p = 0.494). However, the number of patients with purely acute SDH was small (n = 18); and this study was not powered to evaluate the effect of surgery in this subpopulation. Similarly, our multivariable model revealed that the absence of surgical intervention was nonsignificantly associated (p = 0.057) with poor 3-month functional outcome, after adjusting for other factors. As this was an observational study, we cannot draw definitive conclusions about the efficacy of surgical intervention. The use of larger, multicenter observational studies with propensity score matching, or randomized trials of SDH evacuation are warranted to more rigorously evaluate the impact of surgery on outcome.
Other groups have also been unable to show improved outcomes following evacuation of acute SDH. In one study of acute traumatic SDH, decompressive craniectomy failed to demonstrate a favorable benefit on neurological outcome at 1 year [28]. Surgical management of SDH in patients over 70 years of age provided significant improvement in neurological status but did not appear to result in any improvements to functional status [29]. A retrospective review of 1427 patients with acute SDH demonstrated functional independence at discharge in areas of expression, feeding, and locomotion for 92, 81, and 43 %, respectively. Overall in-hospital mortality was 16 % for this cohort, but there was no significant difference between surgically evacuated and non-evacuated groups [30].
There are even fewer data addressing outcomes in patients with chronic SDH who undergo evacuation. In one study, craniotomy was not only associated with higher complication rates, if pursued as the initial line of treatment, but was also found to be superior to minimally invasive procedures for managing SDH recurrence [31]. Within our cohort, although surgical evacuation was univariately associated with better functional outcome, it was not found to be a significant predictor after adjusting for other factors. Furthermore, it is possible that fewer patients in our poor outcome group underwent hematoma evacuation due to reasons related to poor surgical candidacy or early hospital death.
We observed high rates of SDH reaccumulation in those who underwent surgery (60 %) compared to reported rates of 3–76 % [5, 18, 31–40]. However, we were very aggressive in coding reaccumulation, such that even 1 ml increase in SDH volume on follow-up CT was coded as a recurrence, while most studies report recurrence as reaccumulation requiring evacuation. Indeed, the median volume of recurrent SDH postoperatively was only 8.5 mL. Furthermore, only 7 % of our cohort required re-evacuation, which is similar to the reported literature [18, 36, 41]. Overall, after accounting for postoperative reaccumulation, there was still a 60 % reduction in SDH volume with surgery compared to a 10 % spontaneous reduction in SDH volume that occurred without surgery.
Our observation that long-term prognosis appears worse with higher acuity of blood on initial admission head CT is consistent with other studies on mortality and outcome in acute SDH. A multicenter study of 360 patients with severe traumatic brain injury and acute SDH evaluated 6-month functional recovery using the Glasgow Outcome Scale (1–3 vs. 4–5). Overall in-hospital mortality was 46.7 %, unfavorable 6-month outcomes occurred in 18.6 % of patients, and favorable outcome occurred in 32.2 % [20]. Older cohort studies of patients with acute SDH report mortality rates of 60 % and functional recovery in 38 % of patients at 3 months [2]. Although mortality rates are lower in the more recent studies, more patients are left with poor long-term functional recovery; and the rates of good outcomes have not changed in decades. These findings have been corroborated with nationwide data demonstrating decreased in-hospital mortality rates from 15 to 12 % from 1998 to 2007 but increased unsatisfactory discharge disposition from 17 to 20 % [1].
Certain limitations of the study should be mentioned. As a single-center study, the findings presented here may not be generalizable to other institutions with varying patient populations or clinical practices. Our study protocol included all patients admitted to the neurological intensive care unit with primary SDH, including those with subacute or chronic SDH. Therefore, while the study population was likely to carry a better prognosis when compared to cohorts comprised of only acute traumatic SDH, the cohort was also selected from patients with the highest severity of illness necessitating close intensive care unit (ICU) observation. Second, though two radiographic assessments were performed in all patients (at admission and a 6-h stability scan), there was not a protocolized follow-up head CT. Therefore, residual SDH volumes may vary based on when imaging was performed. Finally, because this was an observational study, we were not able to control for selection bias in terms of which patients were offered surgical intervention; however, we did adjust for factors associated with the decision to pursue surgery in multivariable analysis.
Conclusions
Factors associated with poor functional outcome after ICU admission for SDH include older age, worse admission neurological status, worse premorbid functional status, fever during hospitalization, and a history of smoking. Our data suggest that surgical evacuation was associated with improved outcomes, with the greatest benefits observed in mixed acuity or chronic/subacute SDH, although the study was not statistically powered to conclusively determine the impact of surgery. Larger cohort studies with propensity score matching or randomized studies of SDH evacuation in patients where there is clinical equipoise regarding the utility of surgery are necessary to assess the impact of surgical evacuation on long-term prognosis. Identifying those patient characteristics or events where intervention is most likely to result in improved functional recovery has important implications for patient care beyond the immediate hospitalization period. Although national data indicate that in-hospital mortality continues to decline, long-term functional recovery remains poor with nearly 50 % of patients dead or moderate-severely disabled at 3 months.
References
Frontera JA, Egorova N, Moskowitz AJ. National trend in prevalence, cost, and discharge disposition after subdural hematoma from 1998–2007. Crit Care Med. 2011;39(7):1619–25. doi:10.1097/CCM.0b013e3182186ed6.
Koç RK, Akdemir H, Oktem IS, Meral M, Menkü A. Acute subdural hematoma: outcome and outcome prediction. Neurosurg Rev. 1997;20(4):239–44.
Yanaka K, Kamezaki T, Yamada T, Takano S, Meguro K, Nose T. Acute subdural hematoma–prediction of outcome with a linear discriminant function. Neurol Med Chir (Tokyo). 1993;33(8):552–8.
Zumkeller M, Behrmann R, Heissler HE, Dietz H. Computed tomographic criteria and survival rate for patients with acute subdural hematoma. Neurosurgery. 1996;39(4):708–12 discussion 712–713.
Weigel R, Schmiedek P, Krauss JK. Outcome of contemporary surgery for chronic subdural haematoma: evidence based review. J Neurol Neurosurg Psychiatry. 2003;74(7):937–43. doi:10.1136/jnnp.74.7.937.
Miranda LB, Braxton E, Hobbs J, Quigley MR. Chronic subdural hematoma in the elderly: not a benign disease. J Neurosurg. 2011;114(1):72–6. doi:10.3171/2010.8.JNS10298.
Frontera JA, de los Reyes K, Gordon E, et al. Trend in outcome and financial impact of subdural hemorrhage. Neurocrit Care. 2011;14(2):260–6. doi:10.1007/s12028-010-9418-2.
Bullock MR, Povlishock JT. Guidelines for the management of severe traumatic brain injury. Editor’s Commentary. J Neurotrauma. 2007;24(Suppl 1):2. doi:10.1089/neu.2007.9998.
Bullock MR, Chesnut R, Ghajar J, et al. Surgical management of acute subdural hematomas. Neurosurgery. 2006;58(3 Suppl):S16–24 discussion Si–iv.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2(7872):81–4.
Brott T, Adams HP, Olinger CP, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke J Cereb Circ. 1989;20(7):864–70.
Hartley C, Cozens A, Mendelow AD, Stevenson JC. The Apache II scoring system in neurosurgical patients: a comparison with simple Glasgow coma scoring. Br J Neurosurg. 1995;9(2):179–87.
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke J Cereb Circ. 1988;19(5):604–7.
Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61–5.
Gebel JM, Sila CA, Sloan MA, et al. Comparison of the ABC/2 estimation technique to computer-assisted volumetric analysis of intraparenchymal and subdural hematomas complicating the GUSTO-1 trial. Stroke J Cereb Circ. 1998;29(9):1799–801.
Frontera JA, Curtis JR, Nelson JE, et al. Integrating palliative care into the care of neurocritically ill patients: a report from the improving palliative care in the ICU Project Advisory Board and the Center to Advance Palliative Care. Crit Care Med. 2015;43(9):1964–77. doi:10.1097/CCM.0000000000001131.
Weimer J, Nowacki A, Gordon E, Frontera J. Withdrawal of life-sustaining therapy in patients with intracranial hemorrhage: self-fulfilling prophecy or accurate prediction of outcome? Crit Care Med (in press).
Leroy H-A, Aboukaïs R, Reyns N, et al. Predictors of functional outcomes and recurrence of chronic subdural hematomas. J Clin Neurosci. 2015;22(12):1895–900. doi:10.1016/j.jocn.2015.03.064.
Wong GKC, Leung BYL, So SSM, Lam SW, Poon WS. Long-term quality of life outcome (SF-36) in traumatic acute subdural hematoma patients. Acta Neurochir (Wien). 2011;153(1):107–8. doi:10.1007/s00701-010-0855-7.
Leitgeb J, Mauritz W, Brazinova A, et al. Outcome after severe brain trauma due to acute subdural hematoma. J Neurosurg. 2012;117(2):324–33. doi:10.3171/2012.4.JNS111448.
Schneck MJ, Maheswaran M, Leurgans S. Predictors of outcomes after nontraumatic subdural hematoma. J Stroke Cerebrovasc Dis. 2004;13(5):192–5. doi:10.1016/j.jstrokecerebrovasdis.2004.08.003.
Todd MM, Hindman BJ, Clarke WR, et al. Perioperative fever and outcome in surgical patients with aneurysmal subarachnoid hemorrhage. Neurosurgery. 2009;64(5):897–908. doi:10.1227/01.NEU.0000341903.11527.2F discussion 908.
Ginsberg MD, Busto R. Combating hyperthermia in acute stroke: a significant clinical concern. Stroke J Cereb Circ. 1998;29(2):529–34.
Rossi S, Zanier ER, Mauri I, Columbo A, Stocchetti N. Brain temperature, body core temperature, and intracranial pressure in acute cerebral damage. J Neurol Neurosurg Psychiatry. 2001;71(4):448–54.
Diringer MN, Reaven NL, Funk SE, Uman GC. Elevated body temperature independently contributes to increased length of stay in neurologic intensive care unit patients. Crit Care Med. 2004;32(7):1489–95.
Feldmann E, Broderick JP, Kernan WN, et al. Major risk factors for intracerebral hemorrhage in the young are modifiable. Stroke J Cereb Circ. 2005;36(9):1881–5. doi:10.1161/01.STR.0000177480.62341.6b.
Andreasen TH, Bartek J, Andresen M, Springborg JB, Romner B. Modifiable risk factors for aneurysmal subarachnoid hemorrhage. Stroke. 2013;44(12):3607–12. doi:10.1161/STROKEAHA.113.001575.
Wong GKC, Hung Y-W, Chong C, et al. Assessing the neurological outcome of traumatic acute subdural hematoma patients with and without primary decompressive craniectomies. Acta Neurochir Suppl. 2010;106:235–7. doi:10.1007/978-3-211-98811-4_44.
Mulligan P, Raore B, Liu S, Olson JJ. Neurological and functional outcomes of subdural hematoma evacuation in patients over 70 years of age. J Neurosci Rural Pract. 2013;4(3):250–6. doi:10.4103/0976-3147.118760.
Ryan CG, Thompson RE, Temkin NR, Crane PK, Ellenbogen RG, Elmore JG. Acute traumatic subdural hematoma: current mortality and functional outcomes in adult patients at a Level I trauma center. J Trauma Acute Care Surg. 2012;73(5):1348–54. doi:10.1097/TA.0b013e31826fcb30.
Almenawer SA, Farrokhyar F, Hong C, et al. Chronic subdural hematoma management: a systematic review and meta-analysis of 34,829 patients. Ann Surg. 2014;259(3):449–57. doi:10.1097/SLA.0000000000000255.
Taussky P, Fandino J, Landolt H. Number of burr holes as independent predictor of postoperative recurrence in chronic subdural haematoma. Br J Neurosurg. 2008;22(2):279–82. doi:10.1080/02688690701818885.
Pont LMB, Dammers R, Schouten JW, Lingsma HF, Dirven CMF. Clinical factors associated with outcome in chronic subdural hematoma: a retrospective cohort study of patients on preoperative corticosteroid therapy. Neurosurgery. 2012;70(4):873–80. doi:10.1227/NEU.0b013e31823672ad discussion 880.
Yamamoto H, Hirashima Y, Hamada H, Hayashi N, Origasa H, Endo S. Independent predictors of recurrence of chronic subdural hematoma: results of multivariate analysis performed using a logistic regression model. J Neurosurg. 2003;98(6):1217–21. doi:10.3171/jns.2003.98.6.1217.
Mori K, Maeda M. Surgical treatment of chronic subdural hematoma in 500 consecutive cases: clinical characteristics, surgical outcome, complications, and recurrence rate. Neurol Med Chir (Tokyo). 2001;41(8):371–81.
Santarius T, Kirkpatrick PJ, Ganesan D, et al. Use of drains versus no drains after burr-hole evacuation of chronic subdural haematoma: a randomised controlled trial. Lancet Lond Engl. 2009;374(9695):1067–73. doi:10.1016/S0140-6736(09)61115-6.
Abouzari M, Rashidi A, Rezaii J, et al. The role of postoperative patient posture in the recurrence of traumatic chronic subdural hematoma after burr-hole surgery. Neurosurgery. 2007;61(4):794–7. doi:10.1227/01.NEU.0000298908.94129.67 discussion 797.
Chon K-H, Lee J-M, Koh E-J, Choi H-Y. Independent predictors for recurrence of chronic subdural hematoma. Acta Neurochir (Wien). 2012;154(9):1541–8. doi:10.1007/s00701-012-1399-9.
Tahsim-Oglou Y, Beseoglu K, Hänggi D, Stummer W, Steiger H-J. Factors predicting recurrence of chronic subdural haematoma: the influence of intraoperative irrigation and low-molecular-weight heparin thromboprophylaxis. Acta Neurochir (Wien). 2012;154(6):1063–7. doi:10.1007/s00701-012-1334-0 discussion 1068.
Gelabert-González M, Iglesias-Pais M, García-Allut A, Martínez-Rumbo R. Chronic subdural haematoma: surgical treatment and outcome in 1000 cases. Clin Neurol Neurosurg. 2005;107(3):223–9. doi:10.1016/j.clineuro.2004.09.015.
Oh H-J, Lee K-S, Shim J-J, Yoon S-M, Yun I-G, Bae H-G. Postoperative course and recurrence of chronic subdural hematoma. J Korean Neurosurg Soc. 2010;48(6):518–23. doi:10.3340/jkns.2010.48.6.518.
Author contribution
JM Weimer was responsible for data analysis and writing the paper. E Gordon was responsible for data collection and review of the manuscript. JA Frontera was responsible for study design, data collection, data analysis, editing, and reviewing the manuscript. JA Frontera had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Disclosures
The authors have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Weimer, J.M., Gordon, E. & Frontera, J.A. Predictors of Functional Outcome After Subdural Hematoma: A Prospective Study. Neurocrit Care 26, 70–79 (2017). https://doi.org/10.1007/s12028-016-0279-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-016-0279-1