Abstract
Background
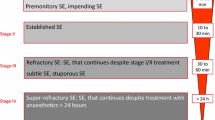
As part of the development of the Neurocritical Care Society (NCS) Status Epilepticus (SE) Guidelines, the NCS SE Writing Committee conducted an international survey of SE experts.
Methods
The survey consisted of three patient vignettes (case 1, an adult; case 2, an adolescent; case 3, a child) and questions regarding treatment. The questions for each case focused on initial and sequential therapy as well as when to use continuous intravenous (cIV) therapy and for what duration. Responses were obtained from 60/120 (50%) of those surveyed.
Results
This survey reveals that there is expert consensus for using intravenous lorazepam for the emergent (first-line) therapy of SE in children and adults. For urgent (second-line) therapy, the most common agents chosen were phenytoin/fosphenytoin, valproate sodium, and levetiracetam; these choices varied by the patient age in the case scenarios. Physicians who care for adult patients chose cIV therapy for RSE, especially midazolam and propofol, rather than a standard AED sooner than those who care for children; and in children, there is a reluctance to choose propofol. Pentobarbital was chosen later in the therapy for all ages.
Conclusion
There is close agreement between the recently published NCS guideline for SE and this survey of experts in the treatment of SE.
Similar content being viewed by others
References
Lowenstein DH, Bleck T, Macdonald RL. It’s time to revise the definition of status epilepticus. Epilepsia. 1999;40(1):120–2.
Brophy GB, Bell R, Alldredge A, Bleck TP, Claassen J, LaRoche SM, Riviello JJ Jr, Shutter L, Sperling MR, Treiman DM, Vespa PM, Neurocritical Care Society Status Epilepticus Guideline Writing Committee. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17:3–23.
Bleck TP. Refractory status epilepticus. Curr Opin Crit Care. 2005;11(2):117–20.
Treiman DM, Meyers PD, Walton NY, Collins JF, Colling C, Rowan AJ, Handforth A, Faught E, Calabrese VP, Uthman BM, et al. A comparison of four treatments for generalized convulsive status epilepticus. Veterans Affairs Status Epilepticus Cooperative Study Group. N Engl J Med. 1998;339(12):792–8.
Cornfield DN, Tegtmeyer K, Nelson MD, Milla CE, Sweeney M. Continuous propofol infusion in 142 critically ill children. Pediatrics. 2002;110(6):1177–81.
Kinoshita H, Nakagawa E, Iwasaki Y, Hanaoka S, Sugai K. Pentobarbital therapy for status epilepticus in children: timing of tapering. Pediatr Neurol. 1995;13(2):164–8.
Holtkamp M, Othman J, Buchheim K, Meierkord M. Predictors and prognosis for refractory status epilepticus treated in a neurological intensive care unit. J Neurol Neurosurg Psychiatry. 2005;76(4):534–9.
Sakuma H. Acute encephalitis with refractory, repetitive partial seizures. Brain Dev. 2009;31(7):510–4.
Sahin M, Menache C, Holmes GL, Riviello JJ. Outcome of severe refractory status epilepticus in children. Epilepsia. 2001;42(11):1461–7.
Sahin M, Menache CC, Holmes GL, Riviello JJ. Outcome of acute symptomatic refractory status epilepticus in children. Neurology. 2003;61(3):398–401.
Kramer U, Shorer Z, Ben-Zeev B, Lerman-Sagie T, Goldberg-Stern H, Lahat E. Severe refractory status epilepticus owing to presumed encephalitis. J Child Neurol. 2005;20(3):184–7.
Mikaeloff Y, Jambaque I, Hertz-Pannier L, Zamfirescu A, Adamsbaum C, Plouin P, Dulac O, Chiron C. Devastating epileptic encephalopathy in school-aged children (DESC): a pseudo encephalitis. Epilepsy Res. 2006;69(1):67–79.
Baxter P, Clarke A, Cross H, Harding B, Hicks E, Livingston J, Surtees R. Idiopathic catastrophic epileptic encephalopathy presenting with acute onset intractable status. Seizure. 2003;12(6):379–87.
Wilder-Smith EP, Lim EC, Teoh HL, Sharma VK, Tan JJ, Chan BP, Ong BK. The NORSE (new-onset refractory status epilepticus) syndrome: defining a disease entity. Ann Acad Med Singapore. 2005;34(7):417–20.
van Baalen A, Hausler M, Boor R, Rohr A, Sperner J, Kurlemann G, Panzer A, Stephani U, Kluger G. Febrile infection-related epilepsy syndrome (FIRES): a nonencephalitic encephalopathy in childhood. Epilepsia. 2010;51(7):1323–8.
Kramer U, Chi CS, Lin KL, Specchio N, Sahin M, Olson H, Nabbout R, Kluger G, Lin JJ, van Baalen A. Febrile infection-related epilepsy syndrome (FIRES): pathogenesis, treatment, and outcome: a multicenter study on 77 children. Epilepsia. 2011;52(11):1956–65.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Riviello, J.J., Claassen, J., LaRoche, S.M. et al. Treatment of Status Epilepticus: An International Survey of Experts. Neurocrit Care 18, 193–200 (2013). https://doi.org/10.1007/s12028-012-9790-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-012-9790-1