Abstract
Background
A study performed in Hong Kong of catheter angiography after ICH found a high rate of structural lesions in patients 45 years of age or younger, without a history of hypertension, or with lobar hemorrhage. We hypothesized that a clinical decision rule based on these Hong Kong criteria would reliably identify patients who require MRI after ICH.
Methods
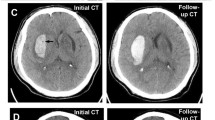
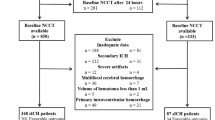
We identified all patients admitted with ICH to our medical center during a 5-year period who underwent brain MRI. Patients were excluded if the history revealed an obvious cause of ICH. Two study neurologists independently adjudicated whether MRI revealed the cause of ICH. We devised a rule recommending MRI if patients met one or more Hong Kong criteria, and calculated the proportion of patients with diagnostic MRI studies who would have been identified by this rule. We also examined the performance of a modified rule using age ≤ 55 years.
Results
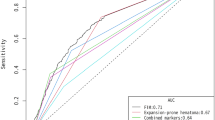
The original Hong Kong rule applied to 102 of the 148 patients in our cohort (69%), and would have recommended MRI in 25 of 27 patients with diagnostic MRI studies (93%, 95% CI 76–99%). The modified rule applied to 110 patients (74%), and would have recommended MRI in all 27 patients with diagnostic MRI studies (100%, 95% CI 91–100%).
Conclusions
A rule based on simple clinical criteria may be useful for stratifying the yield of MRI after ICH. If validated in further studies, such a rule could reduce the number of unnecessary MRI studies after ICH, leading to more cost-effective care.
Similar content being viewed by others
References
Fang J, Alderman MH, Keenan NL, Croft JB. Declining US stroke hospitalization since 1997: National Hospital Discharge Survey, 1988–2004. Neuroepidemiology. 2007;29:243–9.
Counsell C, Boonyakarnkul S, Dennis M, et al. Primary intracerebral haemorrhage in the Oxfordshire Community Stroke Project, 2. Prognosis. Cerebrovasc Dis. 1995;5:26–34.
Broderick JP, Adams HP, Barsan W Jr, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke. 1999;30:905–15.
Zhu XL, Chan MS, Poon WS. Spontaneous intracranial hemorrhage: which patients need diagnostic cerebral angiography? A prospective study of 206 cases and review of the literature. Stroke. 1997;28:1406–9.
Wakai S, Kumakura N, Nagai M. Lobar intracerebral hemorrhage. A clinical, radiographic, and pathological study of 29 consecutive operated cases with negative angiography. J Neurosurg. 1992;76:231–8.
The International Stroke Trial (IST): a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435 patients with acute ischaemic stroke. International Stroke Trial Collaborative Group. Lancet. 1997;349:1569–81.
Cosgrove GR, Leblanc R, Meagher-Villemure K, Ethier R. Cerebral amyloid angiopathy. Neurology. 1985;35:625–31.
Morgenstern LB, Hemphill JC III, Anderson C, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2010;41:2108–29.
Wijman CA, Venkatasubramanian C, Bruins S, Fischbein N, Schwartz N. Utility of early MRI in the diagnosis and management of acute spontaneous intracerebral hemorrhage. Cerebrovasc Dis. 2010;30:456–63.
Dylewski DA, Demchuk AM, Morgenstern LB. Utility of magnetic resonance imaging in acute intracerebral hemorrhage. J Neuroimaging. 2000;10:78–83.
Singer OC, Sitzer M, de Rochemont R, Neumann-Haefelin T. Practical limitations of acute stroke MRI due to patient-related problems. Neurology. 2004;62:1848–9.
Clarke JL, Johnston SC, Farrant M, Bernstein R, Tong D, Hemphill JC III. External validation of the ICH score. Neurocrit Care. 2004;1:53–60.
Zahuranec DB, Gonzales NR, Brown DL, et al. Presentation of intracerebral haemorrhage in a community. J Neurol Neurosurg Psychiatr. 2006;77:340–4.
Cordonnier C, Klijn CJ, van Beijnum J, Al-Shahi Salman R. Radiological investigation of spontaneous intracerebral hemorrhage: systematic review and trinational survey. Stroke. 2010;41:685–90.
Acknowledgment
This research was funded by the Department of Neurology, University of California, San Francisco.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kamel, H., Navi, B.B. & Hemphill, J.C. A Rule to Identify Patients Who Require Magnetic Resonance Imaging After Intracerebral Hemorrhage. Neurocrit Care 18, 59–63 (2013). https://doi.org/10.1007/s12028-011-9607-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-011-9607-7