Abstract
Background and Purpose
Dedicated stroke units are associated with improved patient outcomes after acute ischemic stroke in general. However, it is unknown whether the population of critically ill ischemic stroke patients admitted to the neurocritical care unit (NCCU) benefit from primary management by a specialized neurocritical care team (NCT). This study is intended to investigate such benefit.
Methods
A retrospective chart review in a large academic university hospital identified 400 patients with acute ischemic stroke admitted to the NCCU, from January 1997 to April 2000, aged 65 ± 14 years. We examined the short- and long-term outcomes of these patients before and after institution of a specialized NCT. We used logistic regression models to determine independent association between outcome and availability of NCT.
Results
The presence of a NCT was associated with a decreased length of NCCU stay (2.9 ± 2.0 vs. 3.7 ± 2.9 days, P < 0.01), decreased length of hospital stay (7.5 ± 4.7 vs. 9.9 ± 7.6, P < 0.001), and increased proportion of home discharges (47% vs. 36%, P < 0.05). The only independent predictor of in-hospital and long-term mortality was the underlying severity of disease as determined by the APACHE III score.
Conclusions
In critically ill acute ischemic stroke patients, institution of a dedicated NCT was associated with a reduction in resource utilization and improved patient outcomes at hospital discharge. Several factors including improved patient care protocols may explain this association.
Similar content being viewed by others
Acute ischemic stroke (AIS) patients in general, have better outcomes when admitted to a dedicated stroke unit [1, 2]. Likewise, data supports that critically ill neurology and neurosurgical patients in general may benefit from admission to specialized neurocritical care unit (NCCU) by reduction of in-hospital mortality and length of stay when treated by a full-time neurocritical care team (NCT) [3]. It has also been shown that patients with intracerebral hemorrhage may have better outcomes when they receive specialized care in the NCCU [4, 5]. Such improved outcome is most likely multifactorial and may reflect organizational differences and better management protocols in the NCCU. However, it is unknown whether critically ill AIS patients may also benefit from admission to the NCCU. This led the Brain Attack Coalition to recommend the availability of a specialized NCCU as an option for comprehensive stroke centers [6], which has created some controversy [7]. To address this issue we set out to investigate the relationship between the introduction of a specialized NCT and clinical outcomes of AIS patients requiring critical care. We studied a subset of patients with AIS from a previously published mixed cohort of 2,381 critically ill neurologic and neurosurgical patients [3]. The information presented here is more detailed and specific to AIS patients.
Subjects and Methods
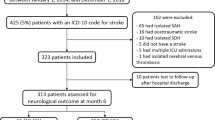
We identified AIS patients admitted to the NCCU at University Hospitals Case Medical Center in Cleveland from a prospectively collected database of ICU patients. We selected patients that met the following criteria: (1) age > 18 years, (2) clinical diagnosis of AIS supported by imaging studies, and (3) admitted from January 1997 to April 2000 to the NCCU. The date range included a 19-month period before and 20-month period after institution of a NCT. During the study period care of AIS patients was based on protocols set up by members of the Brain Attack Team. The only significant change during the study period was the availability of a specialized NCT in September 1998.
We identified 400 patients fulfilling the above criteria and performed a comprehensive review of both the prospectively maintained database and the medical records to obtain the following information: demographics, source of admission, prior functional status, National Institutes Health Stroke Score (NIHSS) and Acute Physiology, Age, Chronic Health Evaluation III score (APACHE III) on admission, reason for admission to the NCCU, vascular territory involved, likely stroke mechanism, Glasgow Coma Scale (GCS), need for mechanical ventilation, presence or absence of the neurocritical care team, hospital discharge disposition, and long-term mortality. We determined prior functional status using a modification of the Rankin Scale as previously reported [3, 8]. The APACHE III score is a validated tool for analysis of ICU patients that takes into account severity of underlying illness to estimate in-hospital mortality [9]. A higher admission score correlates closely with worse outcome. Reasons for admission to the NCCU included the following: unstable or fluctuating neurological status; blood pressure control after thrombolysis; airway protection; cerebral edema with risk of herniation; symptomatic hemorrhagic transformation defined as any hemorrhage seen on head CT with a worsening neurological examination; and others (e.g., various medical complications). Long-term mortality was defined as death at 1 year after stroke as per review of follow-up medical records, or the social security death index database. We obtained prior approval for this study from our institutional review board.
The NCCU was established in 1994, and consists of a ten-bed unit that houses all neurology and neurosurgical patients requiring critical care. The dynamics of the NCCU before and after the availability of the NCT was published previously but we will summarize it here [3]. Conventionally, a general neurology team in conjunction with the brain attack team managed ischemic stroke patients admitted to the NCCU, with various medical and surgical consultative teams employed depending on the specific needs of the patient. This has been called low-intensity staffing [10]. In September 1998, we instituted a specialized NCT, led by full-time neurointensivists, available 24 h and 7 days per week. This has been termed high-intensity staffing [10]. In addition to management of neurocritical care issues, the neurointensivists manage all general critical care issues including pulmonary, cardiac, renal, gastrointestinal and hematological conditions. The team also consists of neurocritical care fellows, rotating residents, specialized neurocritical care nurses, nutritionists, speech, physical and occupational therapists. An intensive educational program regarding specific neurocritical care issues was established including daily didactics for medical house staff and weekly lectures for NCCU nurses. The neurointensivist conducts daily rounds to address active neurological and medical conditions, enforces admission and discharge criteria, creates and manages ICU protocols related to ventilator management, deep venous thromboembolism and gastrointestinal prophylaxis, infection control, nutrition, and institutes specific neuroprotective measures related to body temperature, blood glucose, and blood pressure.
Statistical Analysis
We classified patients into two groups for analysis: before and after availability of the NCT. We performed univariate analyses using the t-test, the Mann–Whitney U-test, or chi-square test as appropriate. The Kolmogorov–Smirnov test was performed to determine normality of different variables. We performed logistic regression analyses to determine relationships between patient characteristics and other covariates on in-hospital and long-term mortality. We also built logistic regression models to investigate the association between several covariates and length of stay (LOS). Because LOS data was not normally distributed we performed a log transformation. The transformed data met the assumption of normality after examining the distribution of residuals. We estimated the magnitude of impact of each independent covariate on LOS by using the regression coefficients from these models as we have previously reported [3]. We also investigated possible interactions and colinearity between the covariates in all the models used and found none. Significance was defined as P-value <0.05. All analyses were conducted with JMP (SAS Institute, Cary, NC) and NCSS 2000 (Kaysville, UT) statistical software.
Results
We identified 400 AIS patients that met eligibility criteria. Most of them were men and their mean age was 65 ± 14 years. We present in Table 1 the main characteristics of the patients according to group assignment. The group that was cared for by the NCT had a significantly decreased NCCU and hospital LOS, and an increased proportion of patients discharged to home. Patients were also significantly younger in this group. There were no other significant differences in the main clinical features between the two groups. The majority of the patients was independent prior to AIS, and was admitted via the emergency department with fluctuating neurological symptoms. The most commonly involved vascular territory was the middle cerebral artery and the most common likely AIS mechanism was embolic. The most prevalent AIS risk factors (not shown on Table 1) included hypertension (45%), atrial fibrillation (38%), diabetes mellitus (36%), coronary artery disease (15%), prior stroke (11%), and heart failure (5.6%). There was no difference between the groups in terms of presence of risk factors.
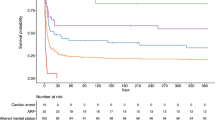
There was no significant difference in in-hospital and long-term (1 year) mortality in patients managed conventionally versus by the NCT. In fact the only predictor of mortality was severity of underlying disease as determined by the APACHE III score. For in-hospital mortality the odds ratio (OR) was 1.08 with confidence intervals (CI) 1.06–1.2 (P < 0.001), and for long-term mortality was 1.07 (CI 1.05–1.09, P < 0.001). Despite the fact that those AIS patients that required mechanical ventilation represented <20% of the total, their mortality was >70% (22/31 and 27/37 in the before and after groups, respectively). The most common probable cause of death was withdrawal of support followed by brain death.
The results for the LOS models are presented in Tables 2 and 3. Determinants of increased NCCU LOS included stroke severity as determined by the NIHSS, and symptomatic hemorrhagic transformation. For the hospital LOS severity of stroke as per the NIHSS, and being moderately disabled prior to admission were independently associated with increased resource utilization. The availability of the NCT was associated with decreased both NCCU and hospital LOS. Other important predictor for reduced hospital LOS was admission via the emergency department.
Discussion
The aim of our study was to explore the relationship between a specialized NCT and outcomes AIS patients requiring admission to the NCCU. To our knowledge, there are no previous reports in the literature on this specific topic. This study suggests that the institution of a NCT is associated with improved patient outcomes. There was also an association between NCT and improved resource utilization as determined by decreased NCCU and hospital LOS. Reasons for this association are not clear but some of the possible explanations for decreased NCCU LOS may include more efficient patient care protocols and enforcing admission and discharge criteria. Additionally, prevention and management of common post-stroke complications such as aspiration and ventilator-associated pneumonia, deep-venous thrombosis and gastrointestinal ulcers, as well as institution of neuroprotective measures including normothermia, normoglycemia and blood pressure management, and management of cerebral edema and brain herniation likely plays an important role in improving outcomes. We also found that significantly more patients were discharged to home. One can only speculate, but most likely careful attention to the myriad factors that may result in secondary deterioration after stroke explains this finding. Our findings also confirm that AIS patients requiring mechanical ventilation have a high mortality rate [11]. We can add that the addition of a NCT was not associated with improved outcome in this group of AIS patients.
The current literature supports a beneficial relationship between the presence of a specialized critical care team and enhanced patient outcomes. For example, Diringer et al. in an analysis of 36,986 patients from 42 intensive care units (ICU) found that critically ill patients with intracranial hemorrhage (ICH) managed in a NCCU staffed by a neurointensivist had better outcomes than those admitted to a general ICU [4]. Similarly, Mirksi et al. reported in ICH patients improved cost of care and outcomes after institution of a NCCU with a dedicated neurointensivist [7]. We also previously reported that neurology and neurosurgical patients in general admitted to a NCCU, had significantly reduced in-hospital mortality and length of stay after institution of a NCT [3].
The beneficial effect of an ICU team on outcomes extends to other specific populations of critically ill ICU patients. Pronovost et al. reported that patients post-abdominal aortic surgery benefited by having an ICU physician conduct daily rounds; in hospitals without a dedicated ICU physician conducting rounds there was a threefold increased in-hospital mortality [12]. Varelas et al. in a multivariate analysis reported that the implementation of a neurointensivist to help manage head-trauma patients in the NCCU was associated with a 51% reduction in NCCU mortality rate (P = 0.01), 12% shorter hospital LOS (P = 0.026), and 57% greater chance of discharge to home (P = 0.009) [13].
Regarding AIS patients there is abundant data to support their management in dedicated stroke units [14–17]. The Brain Attack Coalition issued consensus statements regarding primary and comprehensive stroke centers. They cited “grade 1A” evidence in their recommendation that a dedicated stroke unit be a mandatory element of both primary and comprehensive stroke centers [6, 16]. Additionally, they recommended that a comprehensive stroke center have an ICU available for AIS. These recommendations are welcomed. However, there is disagreement on several key issues. First, they stated that “a dedicated neurosciences ICU, although desirable, is not required…” Second, regarding the staffing of the ICU they stated that “formal training as a neurointensivist, although preferred, is not a requirement.” Our data give support to the sentiments expressed by Hemphill et al. that a NCCU should be mandatory, rather than optional [7].
Our study has several limitations. First, it is a retrospective analysis, and thus we can only say that there is an association between the neuro-ICU team and improved outcomes, but cannot prove a cause and effect relationship. Also, retrospective analyses by nature may be subject to bias inherent to this study type. However, much of the data, including the in-hospital and long-term mortality, severity of illness scores, and admission source was obtained from a prospectively collected database. It is doubtful that a randomized trial of this type will ever be done given the abundant cumulating evidence of the efficacy of critical care specialists on patient outcomes in specific areas as previously discussed. Another limitation is based on the temporal trends in patient populations that occur over time. However, the time period studied, 39 months is relatively short, and we did not observe significant variation in the baseline characteristics of the patients. Finally, although we determined long-term mortality for patients, we did not determine long-term quality of life, which may be more important in this specific patient population. However, we did observe higher proportion of discharges to home, which generally implies a better functional status.
References
Jorgensen HS, Nakayama H, Raaschou HO, Larsen K, Hubbe P, Olsen TS. The effect of a stroke unit: reductions in mortality, discharge rate to nursing home, length of hospital stay, and cost. A community-based study. Stroke 1995;26:1178–82.
Sulter G, Elting JW, Langedijk M, Maurits NM, De Keyser J. Admitting acute ischemic stroke patients to a stroke care monitoring unit versus a conventional stroke unit: a randomized pilot study. Stroke 2003;34:101–4.
Suarez JI, Zaidat OO, Suri MF, Feen ES, Lynch G, Hickman J, Georgiadis A, Selman WR. Length of stay and mortality in neurocritically ill patients: impact of a specialized neurocritical care team. Crit Care Med 2004;32:2311–7.
Diringer MN, Edwards DF. Admission to a neurologic/neurosurgical intensive care unit is associated with reduced mortality rate after intracerebral hemorrhage. Crit Care Med 2001;29:635–40.
Mirski MA, Chang CW, Cowan R. Impact of a neuroscience intensive care unit on neurosurgical patient outcomes and cost of care: evidence-based support for an intensivist-directed specialty ICU model of care. J Neurosurg Anesthesiol 2001;13:83–92.
Alberts MJ, Latchaw RE, Selman WR, Shephard T, Hadley MN, Brass LM, Koroshetz W, Marler JR, Booss J, Zorowitz RD, Croft JB, Magnis E, Mulligan D, Jagoda A, O’Connor R, Cawley CM, Connors JJ, Rose-DeRenzy JA, Emr M, Warren M, Walker MD. Recommendations for comprehensive stroke centers: a consensus statement from the brain attack coalition. Stroke 2005;36:1597–616.
Hemphill JC III, Bleck T, Carhuapoma JR, Chang C, Diringer M, Geocadin R, Mayer S, Samuels O, Vespa P. Is neurointensive care really optional for comprehensive stroke care? Stroke 2005;36:2344–5.
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1988;19:604–7.
Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, Sirio CA, Murphy DJ, Lotring T, Damiano A, Harrell FE Jr. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest 1991;100:1619–36.
Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA 2002;288:2151–62.
Holloway RG, Benesch CG, Burgin WS, Zentner JB. Prognosis and decision making in severe stroke. JAMA 2005;294:725–33.
Pronovost PJ, Jenckes MW, Dorman T, Garrett E, Breslow MJ, Rosenfeld BA, Lipsett PA, Bass E. Organizational characteristics of intensive care units related to outcomes of abdominal aortic surgery. JAMA 1999;14:1310–7.
Varelas PN, Eastwood D, Yun HJ, Spanaki MV, Hacein Bey L, Kessaris C, Gennarelli TA. Impact of a neurointensivist on outcomes in patients with head trauma treated in a neurosciences intensive care unit. J Neurosurg 2006;104:713–9.
Collaborative systematic review of the randomised trials of organised inpatient (stroke unit) care after stroke. Stroke unit trialists’ collaboration. BMJ 1997;314:1151–9.
Langhorne P, Dennis MS. Stroke units: the next 10 years. Lancet 2004;363:834–5.
Alberts MJ, Hademenos G, Latchaw RE, Jagoda A, Marler JR, Mayberg MR, Starke RD, Todd HW, Viste KM, Girgus M, Shephard T, Emr M, Shwayder P, Walker MD. Recommendations for the establishment of primary stroke centers. Brain attack coalition. JAMA 2000;283:3102–9.
Launois R, Giroud M, Megnigbeto AC, Le Lay K, Presente G, Mahagne MH, Durand I, Gaudin AF. Estimating the cost-effectiveness of stroke units in France compared with conventional care. Stroke 2004;35:770–5.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bershad, E.M., Feen, E.S., Hernandez, O.H. et al. Impact of a Specialized Neurointensive Care Team on Outcomes of Critically Ill Acute Ischemic Stroke Patients. Neurocrit Care 9, 287–292 (2008). https://doi.org/10.1007/s12028-008-9051-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-008-9051-5