Abstract
Patients with autoimmune diseases often present with olfactory impairment. The aim of the study was to assess the olfactory functions of female patients with fibromyalgia (FM) compared with patients with systemic sclerosis (SSc) and with healthy female controls. Olfactory functions were assessed in 24 patients with FM, 20 patients with SSc and 21 age-matched healthy controls. The sense of smell was evaluated using the Sniffin’ Sticks test including the three stages of smell: threshold, discrimination, and identification (TDI) of the different odors. The severity of fibromyalgia was assessed using the fibromyalgia impact questionnaire (FIQ). The short form 36 (SF-36) questionnaire was also completed in order to seek a relationship between the patients perception of quality of life and the different aspects of the smell sense. Depression was evaluated in both FM and SSc patients utilizing the Beck depression inventory-II (BDI-II) questionnaire. Patients with FM had significantly lower TDI smell scores compared with both SSc patients and healthy controls (p < 0.005, One-Way ANOVA). Hyposmia (defined as TDI scores below 30) were observed in 14 of 24 (42 %) patients with FM compared to 3 of 20 (15 %) patients with SSc and 1 of the healthy controls (4.3 %) (p < 0.02). FM patients had significantly lower thresholds of smell compared to both healthy controls and patients with SSc (p < 0.001), whereas for patients with SSc only the ability to discriminate between odors was impaired (p < 0.006). We could not detect any statistical correlation between smell abilities and clinical manifestation of SSc or the FIQ and SF-36 scores among FM patients. However the correlation between depression, defined by the BDI-II score, and the sense of smell differed between patients with FM and patients with SSc. As only among SSc patients a lower sense of smell correlated with a higher BDI-II score (p = 0.02). Our findings suggest that there is a decrease in the sense of smell both in FM and SSc patients compared with healthy controls. However these impairments differ between patients group and might represent different mechanisms that affect the sense of smell.
Similar content being viewed by others
Introduction
The sense of smell plays an important role in environment recognition. Olfaction is a complex process of the central nervous system (CNS) involving specific areas of the brain (e.g., the limbic system). Olfactory dysfunction has been confirmed in various neurological as well as psychiatric diseases, such as alzheimer’s disease (AD), down syndrome (DS), parkinson’s disease (PD), schizophrenia and depression [1–3]. Olfactory dysfunction has also been reported in neurologic autoimmune diseases such as multiple sclerosis and myasthenia gravis [4–6], and in various autoimmune diseases such as systemic lupus erythematosus (SLE) [3, 5, 7–18].
Fibromyalgia (FM) is a common cause of chronic, diffuse, musculoskeletal pain. It is a disease that affects muscles and soft tissue such as tendons and ligaments. This condition is not associated with genuine tissue inflammation and the etiology of the disorder remains poorly understood. FM patients report increased sensitivity to diverse stimuli among them also nociceptive input, which via different mechanisms converge to hypersensitize the central nervous system and in many manners are similar to patients with post-traumatic stress disorder, depression and other affective conditions [19–26]. Among other characteristics FM patients tend to report enhanced olfactory acuity [27]. However, not many studies have objectively assessed the olfactory sensitivity in FM patients and one recently published study reported slightly reduced odor identification with no significant differences in smell threshold or discrimination [28].
As a comparator rheumatic condition we chose patients with systemic sclerosis (SSc) since as patients with FM they also have a distressed profile with an increased risk for pain. These patients challenge the healthcare system with a myriad of complaints such as neuropathies, depression, anxiety, fatigue, neuropathic pain, pruritus, body image distress, sexual dysfunction, work disability requiring referrals to a behavioral health specialists and pain management [29–31]. Interestingly assessment of olfaction was never thoroughly investigated in these patients.
In this study we assessed the olfactory functions of female FM patients and compared it to female patients with a classical connective tissue disorder SSc and to healthy female controls. In addition we examined whether an association exists between smell characteristics and the severity of the fibromyalgia syndrome in these patients.
Patients and methods
Patients
Subjects were included in the study if they were above the age of 18 years of age and had a documented clinical diagnosis of FM or SSc according to the ACR criteria of both disorders [32, 33]. The study protocol was reviewed and approved by the ethics committee of our institutions.
Olfactory assessment
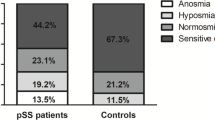
The assessment of olfactory functions was evaluated by using the three stages of the Sniffin’ Sticks kit (Burghart Medizintechnik, Wedel, Germany), which is based on a pen-like odor-dispensing device [17, 34]. In stage 1, threshold was assessed using n-butanol as a single odorant. Three sticks were presented to each subject in a randomized order, two contained solvent and the third contained the odorant at a certain dilution. The subject was then asked to identify the stick with the odorant. In stage 2, discrimination between two different odorants was assessed. The subject was presented with three pens; two contained the same odorant and one contained a different one. The subject was then asked to differentiate between pens. In stage 3, the ability of the subject to identify an odorant out of four options was assessed. The maximum score in each stage was 16 points, with a maximum possible total score of 48 points for the stages of threshold, discrimination, and identification (TDI) combined. Patients with a TDI score of >30 are considered to have normal olfaction (normosmia), patients with a score of 15–30 are considered to have decreased olfaction (hyposmia), and patients with a score of <15 are considered to have a loss of olfaction (anosmia) [17, 34].
Quality of life assessment
All patients completed the SF-36, which assesses functional status on eight descriptively named subscales: physical functioning, role limitations due to physical health problems, bodily pain, general health perceptions, energy and fatigue, social functioning, role limitations due to personal or emotional health problems and emotional well-being. The derivation of these subscales has been well described by Ware and Sherbourne [35]. Each has been shown to have high reliability and validity. They have been used in general population surveys and in a range of patient populations, including those with chronic fatigue syndrome and FM [36], scoring followed published guidelines, resulting in scale ranges from 0 to 100, with higher values representing better function.
Severity of fibromyalgia
The quality of life of the FM patients in this study was assessed using the fibromyalgia impact questionnaire (FIQ), a disease-specific questionnaire used for the evaluation of quality of life in patients with FM [37]. This questionnaire is composed of ten domains, the first consisting of ten sub-items or questions and the other nine of only one question each. The first domain contains questions concerning the capacity of the patient to perform certain routine activities. Responses range from 0, always able to perform the activity, to 3, never able to perform the activity. Item two refers to the number of days during which the patient felt well in the previous week and item three to the number of days on which the patient was unable to go to work because of the disease. Possible answers range from 0 to 7 for each item or domain. For domains 4–10, scores range from 0 to 10 in each. These final seven items are designed to collect data on the patient’s capacity to work and their perceptions of pain, fatigue, morning stiffness, mood, anxiety and depression. The data from the FIQ are arranged so that no more than ten points can be scored for any single item. Items 2 and 3 are considered inversely proportional; therefore, the maximum possible score in this questionnaire will generally be 100.
Depression scores
Both FM and SSc patients were assessed using the Beck depression inventory-II (BDI-II) questionnaire, a 21-item self-report instrument to assess the existence and severity of symptoms of depression [38, 39]. Participants are asked to rate how they have been feeling for the past 2 weeks and to score the questionnaire accordingly.
The BDI-II contains 21 questions, each answer being scored on a scale value of 0–3. The cutoffs used differ from the original: 0–13: minimal depression; 14–19: mild depression; 20–28: moderate depression; and 29–63: severe depression. Higher total scores indicate more severe depressive symptoms.
Statistical analysis
Normally distributed variables were summarized using the mean ± SD, and non-normally distributed variables by the median and range. Univariate comparisons between nominal variables were performed by Chi square test. For assessment of the correlation between two continuous variables, we used Pearson’s and Spearman’s correlation coefficient for normal and non-normal variables each when appropriate. p ≤ 0.05 were considered significant. All the statistical calculations were performed using SAS statistical software (SAS Institute, Cary, NC, USA).
Results
Two groups of patients were examined in this study. Twenty-four FM patients and twenty SSc patients the healthy control group was composed of 21 matched females. Ages ranged from 21 to 78 years. All subjects were female. Subjects with histories of head injuries, nasofacial operations, or active nasal-sinus or allergic diseases were excluded from the study. There was no significant difference between the age of the FM, SSc and control groups enrollees; 53.7 ± 12.1, 54 ± 14.5 and 47.5 ± 10 (mean ± SD) respectively (p > 0.05) (Table 1).
Patients with FM and SSc had significantly lower smell scores compared to healthy controls (Table 1). Overall patients with FM had lower scores when compared to patients with SSc and healthy controls (p < 0.001, one-way ANOVA). Hyposmia (defined as TDI scores below 30) was observed significantly more often in patients with FM compared to enrollees of the groups, 14 of 24 (42 %) patients with FM compared to 3 of 20 (15 %) patients with SSc and 1 of the healthy controls (4.3 %) (p < 0.02).
Although patients with FM displayed diminished olfactory function in all examined parameters we could not determine any correlation between the TDI scores and fibromyalgia severity measured by either FIQ or SF-36.
FM patients had low scores of quality of life compared to expected values. In addition 47 % of the patients with FM according to the BDI-II score had depression of them 10 % had either moderate or severe forms [38]. Although the FIQ and the SF-36 closely correlated Pearson’s correlation of r −0.84, (p < 0.001), we could not detect among the FM patients any quantative correlation between their olfactory disorder to either the FIQ or to the BDI-II severity scores.
Patients with SSc had a total overall TDI score that was lower than the control group, but when examining the subcategories, only the ability to discriminate between odors was impaired, yet not reaching statistical significance (p = 0.06) (Table 2). A significant inverse correlation between the severity depression, defined by the BDI-II scores and the olfactory functions in patients with SSc (Pearson’s correlation of −0.5, p < 0.05) was detected.
Discussion
The importance of a smell threshold can be easily understood, since smell odorants are crucial to preserve health such as avoiding food that has spoiled or breathing leaks in a gas line. The smell function is the first to be impaired with age [40]. Olfaction dysfunction is considered to be a common finding in the general population. The prevalence is a matter of debate. An estimated rate of 1 % of the general population have anosmia (loss of smell), and 5–8 % suffer from hyposmia (reduced olfactory function) [41]. It is well known that the limbic system plays a major role in the perception of odor sensation as well as emotions recognition and conceptualization.
Association between olfaction and depression was first described in the rodent model, where bilateral destruction of the olfactory bulb altered serotonin and dopamine concentrations leading to a depression-like behavior [42, 43]. This association has been reported also in humans; patients with olfactory impairment or congenital anosmia are more likely to present with symptoms of depression [40, 44]. On the other side, depressed patients exhibit reduced olfactory threshold, identification and discrimination ability and following successful therapeutic therapy these parameters normalize [45–48].
In one study, a reduced olfactory sensitivity was reported in 14 patients with obsessive compulsive disorder and nine major depressive disorder patients. Treatment with antidepressant medication significantly improved olfactory function in these patients [49]. Another study suggested that depressive symptoms in healthy subjects are accompanied by olfactory deficits [50].
Several studies using neuroimaging, neuropathology and lesion analysis have associated olfaction with depression. It has for instance been demonstrated that the severity of depression correlates with an increased physiological activity as well as gray matter size reductions in the olfactory system of depressed patients [51–53]. Once again effective antidepressant treatment was shown to be associated with reduction in activity in this region [54].
Several studies conducted in patients with depression provide evidence of amygdala involvement. In one study, the core amygdala nuclei were measured in 20 patients with a history of depression. The results showed that depressed subjects had bilaterally reduced amygdala core nuclei volumes without significant differences in whole brain volumes [55]. Functional neuroimaging studies also show decreased blood flow and impaired function of the amygdala in depressed patients [51, 55, 56].
In a recent interesting study Croy et al. [57] studied olfactory functions in 27 female patients with depression at the beginning and at the end of anti-depressive therapy; they also measured chemosensory event related potentials and functional magnetic resonance imaging mapping olfactory capabilities. These patients exhibited reduced olfactory discrimination, prolonged latencies of the event-related potential and reduced activation in secondary olfactory structures (thalamus, insula, and left middle orbitofrontal). After therapy these parameters had normalized. An interesting association between pain and smell might arise from a recent finding regarding the SCN9A gene, which encodes the voltage-gated sodium channel Nav1.7. Several pain syndromes have been linked to different mutations in the SCN9A gene [58]. Weiss et al. [59] described a complete absence of odor detection in three patients with SCN9A loss-of-function mutations and concluded that Nav1.7 is an essential requirement for human olfaction. Nav1.7 staining was detected not in the olfactory epithelium but in individual glomeruli of the olfactory bulb [60].
The aim of the present study was to assess olfactory functions among FM patients and to measure there association to various aspects of the FM construct. As controls we elected patients with SSc that present a classical connective tissue disorder with expected olfactory malfunction and healthy female controls.
We detected high rates of olfactory impairment among patients with FM. Fifteen of 24 fibromyalgia patients were found to have significantly reduced smell sensation while only 3 of 20 SSc patients had similar findings.
Many ties link the immune system with the olfaction; the immune and olfactory systems are both influenced by external stimuli of our close environment [5, 15, 16, 61]. Both systems discriminate between self and non-self and both are major histocompatibility complex (MHC) dependent [61].
Several studies have shown that odorants suppress immune reaction in mice. Inhaled odorants were shown to protect mast cell activation by blocking the induction of substance p or the stress induced activation of suppressor T lymphocytes. It has been demonstrated that when immunological function is impaired olfaction may be affected and vice versa. Several effects on the immune system have been found in olfactory bulbectomized animals, including changes in number and function of phagocytes and lymphocytes; increased leukocyte aggregation; increased levels of acute phase proteins; and enhanced nocturnal secretion of corticosterone. In general, an inflammatory pattern of response develops, with increased levels of serum interleukin (IL)-1β and prostaglandin E2, and decreased levels of IL-10 [43]. We have reported on altered smell perception in patients with SLE [17]. In these patients almost half had a decreased sense of smell and 10 % were found to be anosmic.
The hippocampus, located in the temporal lobe, is a structure intimately associated with olfaction Several studies have shown that patients with SLE had significant hippocampal atrophy that correlated with disease duration, total corticosteroid dose and greater number of CNS manifestations [62]. In another study we have demonstrated that injection of anti-P ribosomal antibodies (anti-P) directly to the brain ventricles of mice induced depressive manifestations. These findings significantly improved following treatment with fluoxetine and to a certain extent by their exposure to lemon odor [9, 10].
Surprisingly smell dysfunction has not been investigated in patients with SSc. In the past it had been olfactory dysfunction was regarded as an adverse event of penicillamine however since this medication is hardly used anymore, none of our patients was on this medication [63]. In this report we detected a high degree of depression among SSc patients reaching 30 %, interestingly in these patients we could detect an inverse correlation between this depressive symptoms and their smell scores.
In conclusion, in this study we have observed that the olfactory sense is impaired in female patients with FM and SSc. In patients with SSc this dysfunction was found to correlate with the severity of their concomitant depression.
References
Doty RL. Olfaction in Parkinson’s disease and related disorders. Neurobiol Dis. 2012;46:527–52.
Moberg PJ, Kamath V, Marchetto DM, Calkins ME, Doty RL, Hahn CG, Borgmann-Winter KE, Kohler CG, Gur RE, Turetsky BI. Meta-Analysis of olfactory function in schizophrenia, first-degree family members, and youths at-risk for psychosis. Schizophr Bull. 2013;40:50–9.
Ortega-Hernandez OD, Kivity S, Shoenfeld Y. Olfaction, psychiatric disorders and autoimmunity: is there a common genetic association? Autoimmunity. 2009;42:80–8.
Demarquay G, Ryvlin P, Royet JP. Olfaction and neurological diseases: a review of the literature. Rev Neurol (Paris). 2007;163:155–67.
Strous RD, Shoenfeld Y. To smell the immune system: olfaction, autoimmunity and brain involvement. Autoimmun Rev. 2006;6:54–60.
Leon-Sarmiento FE, Bayona EA, Bayona-Prieto J, Osman A, Doty RL. Profound olfactory dysfunction in myasthenia gravis. PLoS One. 2012;7:e45544.
Benkler M, Agmon-Levin N, Shoenfeld Y. Parkinson’s disease, autoimmunity, and olfaction. Int J Neurosci. 2009;119:2133–43.
Katzav A, Solodeev I, Brodsky O, Chapman J, Pick CG, Blank M, Zhang W, Reichlin M, Shoenfeld Y. Induction of autoimmune depression in mice by anti-ribosomal P antibodies via the limbic system. Arthritis Rheum. 2007;56:938–48.
Katzav A, Ben-Ziv T, Chapman J, Blank M, Reichlin M, Shoenfeld Y. Anti-P ribosomal antibodies induce defect in smell capability in a model of CNS-SLE (depression). J Autoimmun. 2008;31:393–8.
Katzav A, Ben-Ziv T, Blank M, Pick CG, Shoenfeld Y, Chapman J. Antibody-specific behavioral effects: Intracerebroventricular injection of antiphospholipid antibodies induces hyperactive behavior while anti-ribosomal-P antibodies induces depression and smell deficits in mice. J Neuroimmunol. 2014;272:10–15.
Kivity S, Ortega-Hernandez OD, Shoenfeld Y. Olfaction—a window to the mind. Isr Med Assoc J. 2009;11:238–43.
Kivity S, Tsarfaty G, Agmon-Levin N, Blank M, Manor D, Konen E, Chapman J, Reichlin M, Wasson C, Shoenfeld Y, Kushnir T. Abnormal olfactory function demonstrated by manganese-enhanced MRI in mice with experimental neuropsychiatric lupus. Ann N Y Acad Sci. 2010;1193:70–7.
Moscavitch SD, Szyper-Kravitz M, Shoenfeld Y. Smell: integrating neurodegeneration and autoimmunity-a personal view. Acta Reumatol Port. 2009;34:190–6.
Moscavitch SD, Szyper-Kravitz M, Shoenfeld Y. Autoimmune pathology accounts for common manifestations in a wide range of neuro-psychiatric disorders: the olfactory and immune system interrelationship. Clin Immunol. 2009;130:235–43.
Perricone C, Agmon-Levin N, Shoenfeld N, de Carolis C, Guarino MD, Gigliucci G, Milana I, Novelli L, Valesini G, Perricone R, Shoenfeld Y. Evidence of impaired sense of smell in hereditary angioedema. Allergy. 2011;66:149–54.
Perricone C, Shoenfeld N, Agmon-Levin N, de Carolis C, Perricone R, Shoenfeld Y. Smell and autoimmunity: a comprehensive review. Clin Rev Allergy Immunol. 2013;45:87–96.
Shoenfeld N, Agmon-Levin N, Flitman-Katzevman I, Paran D, Katz BS, Kivity S, Langevitz P, Zandman-Goddard G, Shoenfeld Y. The sense of smell in systemic lupus erythematosus. Arthritis Rheum. 2009;60:1484–7.
Shoenfeld Y. To smell autoimmunity: anti-P-ribosomal autoantibodies, depression, and the olfactory system. J Autoimmun. 2007;28:165–9.
Ablin JN, Amital H, Ehrenfeld M, Aloush V, Elkayam O, Langevitz P, Mevorach D, Mader R, Sachar T, Amital D, Buskila D. Guidelines for the diagnosis and treatment of the fibromyalgia syndrome. Harefuah 2013;152:742–7, 751, 750.
Amital D, Fostick L, Polliack ML, Segev S, Zohar J, Rubinow A, Amital H. Posttraumatic stress disorder, tenderness, and fibromyalgia syndrome: are they different entities? J Psychosom Res. 2006;61:663–9.
Amital D, Herskovitz C, Fostick L, Silberman A, Doron Y, Zohar J, Itsekson A, Zolti M, Rubinow A, Amital H. The premenstrual syndrome and fibromyalgia–similarities and common features. Clin Rev Allergy Immunol. 2010;38:107–15.
Amital H, Ablin J, Aloush V, Hauser W, Buskila D. The first Israeli fibromyalgia congress, February 2013. Isr Med Assoc J. 2013;15:789–92.
Fitzcharles MA, Shir Y, Ablin JN, Buskila D, Amital H, Henningsen P, Hauser W. Classification and clinical diagnosis of fibromyalgia syndrome: recommendations of recent evidence-based interdisciplinary guidelines. Evid Based Complement Alternat Med. 2013;2013:528952.
Grodman I, Buskila D, Arnson Y, Altaman A, Amital D, Amital H. Understanding fibromyalgia and its resultant disability. Isr Med Assoc J. 2011;13:769–72.
Milstein R, Amital D, Arnson Y, Amital H. Retraumatization eliciting the presentation of fibromyalgia. Isr Med Assoc J. 2013;15:123–4.
Vishne T, Fostick L, Silberman A, Kupchick M, Rubinow A, Amital H, Amital D. Fibromyalgia among major depression disorder females compared to males. Rheumatol Int. 2008;28:831–6.
Wilbarger JL, Cook DB. Multisensory hypersensitivity in women with fibromyalgia: implications for well being and intervention. Arch Phys Med Rehabil. 2011;92:653–6.
Lotsch J, Kraetsch HG, Wendler J, Hummel T. Self-ratings of higher olfactory acuity contrast with reduced olfactory test results of fibromyalgia patients. Int J Psychophysiol. 2012;86:182–6.
Malcarne VL, Fox RS, Mills SD, Gholizadeh S. Psychosocial aspects of systemic sclerosis. Curr Opin Rheumatol. 2013;25:707–13.
Merz EL, Malcarne VL, Assassi S, Nair DK, Graham TA, Yellman BP, Estrada YMR, Mayes MD. Biopsychosocial typologies of pain in a cohort of patients with systemic sclerosis. Arthritis Care Res (Hoboken). 2014;66:567–74.
Milette K, Hudson M, Korner A, Baron M, Thombs BD. Sleep disturbances in systemic sclerosis: evidence for the role of gastrointestinal symptoms, pain and pruritus. Rheumatology (Oxford). 2013;52:1715–20.
van den Hoogen F, Khanna D, Fransen J, Johnson SR, Baron M, Tyndall A, Matucci-Cerinic M, Naden RP, Medsger TA Jr, Carreira PE, Riemekasten G, Clements PJ, Denton CP, Distler O, Allanore Y, Furst DE, Gabrielli A, Mayes MD, van Laar JM, Seibold JR, Czirjak L, Steen VD, Inanc M, Kowal-Bielecka O, Muller-Ladner U, Valentini G, Veale DJ, Vonk MC, Walker UA, Chung L, Collier DH, Ellen CM, Fessler BJ, Guiducci S, Herrick A, Hsu VM, Jimenez S, Kahaleh B, Merkel PA, Sierakowski S, Silver RM, Simms RW, Varga J, Pope JE. Classification criteria for systemic sclerosis: an American college of rheumatology/European league against rheumatism collaborative initiative. Ann Rheum Dis. 2013;72:1747–55.
Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, Tugwell P, Campbell SM, Abeles M, Clark P. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. report of the multicenter criteria committee. Arthritis Rheum. 1990;33:160–72.
Hummel T, Sekinger B, Wolf SR, Pauli E, Kobal G. ‘Sniffin’ sticks’: olfactory performance assessed by the combined testing of odor identification, odor discrimination and olfactory threshold. Chem Senses. 1997;22:39–52.
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
Neumann L, Berzak A, Buskila D. Measuring health status in Israeli patients with fibromyalgia syndrome and widespread pain and healthy individuals: utility of the short form 36-item health survey (SF-36). Semin Arthritis Rheum. 2000;29:400–8.
Burckhardt CS, Clark SR, Bennett RM. The fibromyalgia impact questionnaire: development and validation. J Rheumatol. 1991;18:728–33.
Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck depression inventories-IA and -II in psychiatric outpatients. J Pers Assess. 1996;67:588–97.
Shean G, Baldwin G. Sensitivity and specificity of depression questionnaires in a college-age sample. J Genet Psychol. 2008;169:281–8.
Deems DA, Doty RL, Settle RG, Moore-Gillon V, Shaman P, Mester AF, Kimmelman CP, Brightman VJ, Snow JB Jr. Smell and taste disorders, a study of 750 patients from the University of pennsylvania Smell and Taste Center. Arch Otolaryngol Head Neck Surg. 1991;117:519–28.
Mombaerts P. Love at first smell—the 2004 nobel prize in physiology or medicine. N Engl J Med. 2004;351:2579–80.
Masini CV, Holmes PV, Freeman KG, Maki AC, Edwards GL. Dopamine overflow is increased in olfactory bulbectomized rats: an in vivo microdialysis study. Physiol Behav. 2004;81:111–9.
Song C, Leonard BE. The olfactory bulbectomised rat as a model of depression. Neurosci Biobehav Rev. 2005;29:627–47.
Temmel AF, Quint C, Schickinger-Fischer B, Klimek L, Stoller E, Hummel T. Characteristics of olfactory disorders in relation to major causes of olfactory loss. Arch Otolaryngol Head Neck Surg. 2002;128:635–41.
Atanasova B, El-Hage W, Chabanet C, Gaillard P, Belzung C, Camus V. Olfactory anhedonia and negative olfactory alliesthesia in depressed patients. Psychiatry Res. 2010;176:190–6.
Pause BM, Miranda A, Goder R, Aldenhoff JB, Ferstl R. Reduced olfactory performance in patients with major depression. J Psychiatr Res. 2001;35:271–7.
Pause BM, Raack N, Sojka B, Goder R, Aldenhoff JB, Ferstl R. Convergent and divergent effects of odors and emotions in depression. Psychophysiology. 2003;40:209–25.
Pause BM, Hellmann G, Goder R, Aldenhoff JB, Ferstl R. Increased processing speed for emotionally negative odors in schizophrenia. Int J Psychophysiol. 2008;70:16–22.
Gross-Isseroff R, Luca-Haimovici K, Sasson Y, Kindler S, Kotler M, Zohar J. Olfactory sensitivity in major depressive disorder and obsessive compulsive disorder. Biol Psychiatry. 1994;35:798–802.
Pollatos O, Albrecht J, Kopietz R, Linn J, Schoepf V, Kleemann AM, Schreder T, Schandry R, Wiesmann M. Reduced olfactory sensitivity in subjects with depressive symptoms. J Affect Disord. 2007;102:101–8.
Drevets WC. Prefrontal cortical-amygdalar metabolism in major depression. Ann N Y Acad Sci. 1999;877:614–37.
Drevets WC, Bogers W, Raichle ME. Functional anatomical correlates of antidepressant drug treatment assessed using PET measures of regional glucose metabolism. Eur Neuropsychopharmacol. 2002;12:527–44.
Wagner G, Koch K, Schachtzabel C, Reichenbach JR, Sauer H, Schlosser RG. Enhanced rostral anterior cingulate cortex activation during cognitive control is related to orbitofrontal volume reduction in unipolar depression. J Psychiatry Neurosci. 2008;33:199–208.
Drevets WC. Orbitofrontal cortex function and structure in depression. Ann N Y Acad Sci. 2007;1121:499–527.
Sheline YI, Gado MH, Price JL. Amygdala core nuclei volumes are decreased in recurrent major depression. NeuroReport. 1998;9:2023–8.
Whalen PJ, Shin LM, Somerville LH, McLean AA, Kim H. Functional neuroimaging studies of the amygdala in depression. Semin Clin Neuropsychiatry. 2002;7:234–42.
Croy I, Symmank A, Schellong J, Hummel C, Gerber J, Joraschky P, Hummel T. Olfaction as a marker for depression in humans. J Affect Disord. 2014;160:80–6.
Cox JJ, Sheynin J, Shorer Z, Reimann F, Nicholas AK, Zubovic L, Baralle M, Wraige E, Manor E, Levy J, Woods CG, Parvari R. Congenital insensitivity to pain: novel SCN9A missense and in-frame deletion mutations. Hum Mutat. 2010;31:E1670–86.
Weiss J, Pyrski M, Jacobi E, Bufe B, Willnecker V, Schick B, Zizzari P, Gossage SJ, Greer CA, Leinders-Zufall T, Woods CG, Wood JN, Zufall F. Loss-of-function mutations in sodium channel Nav1.7 cause anosmia. Nature. 2011;472:186–90.
Zufall F, Pyrski M, Weiss J, Leinders-Zufall T. Link between pain and olfaction in an inherited sodium channelopathy. Arch Neurol. 2012;69:1119–23.
Doherty PC. On the nose: shared themes for the sensory and immune self. Nat Immunol. 2003;4:1043–5.
Appenzeller S, Carnevalle AD, Li LM, Costallat LT, Cendes F. Hippocampal atrophy in systemic lupus erythematosus. Ann Rheum Dis. 2006;65:1585–9.
Keiser HR, Henkin RI, Bartter FC, Sjoerdsma A. Loss of taste during therapy with penicillamine. JAMA. 1968;203:381–3.
Author information
Authors and Affiliations
Corresponding author
Additional information
Howard Amital and Nancy Agmon-Levin have contributed equally to this study.
Rights and permissions
About this article
Cite this article
Amital, H., Agmon-Levin, N., Shoenfeld, N. et al. Olfactory impairment in patients with the fibromyalgia syndrome and systemic sclerosis. Immunol Res 60, 201–207 (2014). https://doi.org/10.1007/s12026-014-8573-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12026-014-8573-5