Abstract
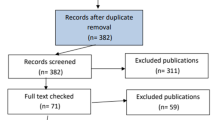
Successful treatment of Cushing syndrome causes transient or permanent adrenal insufficiency deriving from endogenous hypercortisolism-induced hypothalamus–pituitary–adrenal–axis suppression. We analyzed pre-treatment factors potentially affecting the duration of adrenal insufficiency. We conducted a retrospective analysis on patients successfully treated for Cushing disease (15 patients) who underwent transsphenoidal surgery, and nonmalignant primary adrenal Cushing syndrome (31 patients) who underwent unilateral adrenalectomy, divided into patients with overt primary adrenal Cushing syndrome (14 patients) and subclinical primary adrenal Cushing syndrome (17 patients). Epidemiological data, medical history, and hormonal parameters depending on the etiology of hypercortisolism were collected and compared to the duration of adrenal insufficiency. The median duration of follow-up after surgery for Cushing disease and primary adrenal Cushing syndrome was 70 and 48 months, respectively. In the Cushing disease group, the median duration of adrenal insufficiency after transsphenoidal surgery was 15 months: younger age at diagnosis and longer duration of signs and symptoms of hypercortisolism before diagnosis and surgery were associated with longer duration of adrenal insufficiency. The median duration of adrenal insufficiency was 6 months for subclinical primary adrenal Cushing syndrome and 18.5 months for overt primary adrenal Cushing syndrome. The biochemical severity of hypercortisolism, the grade of hypothalamus–pituitary–adrenal–axis suppression, and treatment with ketoconazole before surgery accounted for longer duration of adrenal insufficiency. In patients with Cushing disease, younger age and delayed diagnosis and treatment predict longer need for glucocorticoid replacement therapy after successful transsphenoidal surgery. In patients with primary adrenal Cushing syndrome, the severity of hypercortisolism plays a primary role in influencing the duration of adrenal insufficiency after unilateral adrenalectomy.





Similar content being viewed by others
References
J. Newell-Price, X. Bertagna, A.B. Grossman, L.K. Nieman, Cushing’s syndrome. Lancet 367(9522), 1605–1617 (2006). doi:10.1016/S0140-6736(06)68699-6
L.K. Nieman, B.M. Biller, J.W. Findling, J. Newell-Price, M.O. Savage, P.M. Stewart, V.M. Montori, The diagnosis of Cushing’s syndrome: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 93(5), 1526–1540 (2008). doi:10.1210/jc.2008-0125
C.M. Berr, G. Di Dalmazi, A. Osswald, K. Ritzel, M. Bidlingmaier, L.L. Geyer, M. Treitl, K. Hallfeldt, W. Rachinger, N. Reisch, R. Blaser, J. Schopohl, F. Beuschlein, M. Reincke, Time to recovery of adrenal function after curative surgery for Cushing’s syndrome depends on etiology. J. Clin. Endocrinol. Metab. 100(4), 1300–1308 (2015). doi:10.1210/jc.2014-3632
T. Deutschbein, M. Broecker-Preuss, M.F. Hartmann, R. Althoff, S.A. Wudy, K. Mann, S. Petersenn, Measurement of urinary free cortisol by current immunoassays: need for sex-dependent reference ranges to define hypercortisolism. Horm. Metab. Res. 43(10), 714–719 (2011). doi:10.1055/s-0031-1286297
S. Persichilli, J. Gervasoni, F. Iavarone, C. Zuppi, A simple liquid chromatography-tandem mass spectrometry method for urinary free cortisol analysis: suitable for routine purpose. Clin. Chem. Lab. Med. 48(10), 1433–1437 (2010). doi:10.1515/CCLM.2010.282
M. Sereg, A. Szappanos, J. Toke, K. Karlinger, K. Feldman, E. Kaszper, I. Varga, E. Glaz, K. Racz, M. Toth, Atherosclerotic risk factors and complications in patients with non-functioning adrenal adenomas treated with or without adrenalectomy: a long-term follow-up study. Eur. J. Endocrinol. 160(4), 647–655 (2009). doi:10.1530/EJE-08-0707
M. Terzolo, S. Bovio, A. Pia, P.A. Conton, G. Reimondo, C. Dall’Asta, D. Bemporad, A. Angeli, G. Opocher, M. Mannelli, B. Ambrosi, F. Mantero, Midnight serum cortisol as a marker of increased cardiovascular risk in patients with a clinically inapparent adrenal adenoma. Eur. J. Endocrinol. 153(2), 307–315 (2005). doi:10.1530/eje.1.01959
I. Chiodini, Clinical review: diagnosis and treatment of subclinical hypercortisolism. J. Clin. Endocrinol. Metab. 96(5), 1223–1236 (2011). doi:10.1210/jc.2010-2722
F. Esposito, J.R. Dusick, P. Cohan, P. Moftakhar, D. McArthur, C. Wang, R.S. Swerdloff, D.F. Kelly, Clinical review: early morning cortisol levels as a predictor of remission after transsphenoidal surgery for Cushing’s disease. J. Clin. Endocrinol. Metab. 91(1), 7–13 (2006). doi:10.1210/jc.2005-1204
G. Di Dalmazi, C.M. Berr, M. Fassnacht, F. Beuschlein, M. Reincke, Adrenal function after adrenalectomy for subclinical hypercortisolism and Cushing’s syndrome: a systematic review of the literature. J. Clin. Endocrinol. Metab. 99(8), 2637–2645 (2014). doi:10.1210/jc.2014-1401
P.A. Fitzgerald, D.C. Aron, J.W. Findling, R.M. Brooks, C.B. Wilson, P.H. Forsham, J.B. Tyrrell, Cushing’s disease: transient secondary adrenal insufficiency after selective removal of pituitary microadenomas; evidence for a pituitary origin. J. Clin. Endocrinol. Metab. 54(2), 413–422 (1982). doi:10.1210/jcem-54-2-413
A.R. Hermus, G.F. Pieters, G.J. Pesman, E. Meijer, A.G. Smals, T.J. Benraad, P.W. Kloppenborg, Coexistence of hypothalamic and pituitary failure after successful pituitary surgery in Cushing’s disease?. J. Endocrinol. Invest. 10(4), 365–369 (1987). doi:10.1007/BF03348149
J. Flitsch, D.K. Ludecke, U.J. Knappe, W. Saeger, Correlates of long-term hypocortisolism after transsphenoidal microsurgery for Cushing’s disease. Exp. Clin. Endocrinol. Diabetes 107(3), 183–189 (1999). doi:10.1055/s-0029-1212095
M. Lodish, S.V. Dunn, N. Sinaii, M.F. Keil, C.A. Stratakis, Recovery of the hypothalamic-pituitary-adrenal axis in children and adolescents after surgical cure of Cushing’s disease. J. Clin. Endocrinol. Metab. 97(5), 1483–1491 (2012). doi:10.1210/jc.2011-2325
D. Bochicchio, M. Losa, M. Buchfelder, Factors influencing the immediate and late outcome of Cushing’s disease treated by transsphenoidal surgery: a retrospective study by the European Cushing’s disease survey group. J. Clin. Endocrinol. Metab. 80(11), 3114–3120 (1995). doi:10.1210/jcem.80.11.7593411
N. Sonino, M. Zielezny, G.A. Fava, F. Fallo, M. Boscaro, Risk factors and long-term outcome in pituitary-dependent Cushing’s disease. J. Clin. Endocrinol. Metab. 81(7), 2647–2652 (1996). doi:10.1210/jcem.81.7.8675592
S.H. Roerink, M.A. Wagenmakers, J.W. Smit, E.F. van Rossum, R.T. Netea-Maier, T.S. Plantinga, A.R. Hermus, Glucocorticoid receptor polymorphisms modulate cardiometabolic risk factors in patients in long-term remission of Cushing’s syndrome. Endocrine (2016). doi:10.1007/s12020-016-0883-z
O. Ragnarsson, C.A. Glad, P. Berglund, R. Bergthorsdottir, D.N. Eder, G. Johannsson, Common genetic variants in the glucocorticoid receptor and the 11beta-hydroxysteroid dehydrogenase type 1 genes influence long-term cognitive impairments in patients with Cushing’s syndrome in remission. J. Clin. Endocrinol. Metab. 99(9), E1803–1807 (2014). doi:10.1210/jc.2014-1906
L. Trementino, G. Appolloni, C. Concettoni, M. Cardinaletti, M. Boscaro, G. Arnaldi, Association of glucocorticoid receptor polymorphism A3669G with decreased risk of developing diabetes in patients with Cushing’s syndrome. Eur. J. Endocrinol. 166(1), 35–42 (2012). doi:10.1530/EJE-11-0722
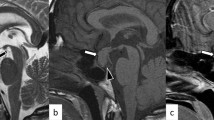
M.P. Ricciato, V. Di Donna, G. Perotti, A. Pontecorvi, R. Bellantone, S.M. Corsello, The role of adrenal scintigraphy in the diagnosis of subclinical Cushing’s syndrome and the prediction of post-surgical hypoadrenalism. World J. Surg. 38(6), 1328–1335 (2014). doi:10.1007/s00268-014-2482-6
L.M. Fig, M.D. Gross, B. Shapiro, D.A. Ehrmann, J.E. Freitas, D.E. Schteingart, G.M. Glazer, I.R. Francis, Adrenal localization in the adrenocorticotropic hormone-independent Cushing syndrome. Ann. Intern. Med. 109(7), 547–553 (1988)
D. Rubello, C. Bui, D. Casara, M.D. Gross, L.M. Fig, B. Shapiro, Functional scintigraphy of the adrenal gland. Eur. J. Endocrinol. 147(1), 13–28 (2002)
A.M. Avram, L.M. Fig, M.D. Gross, Adrenal gland scintigraphy. Semin. Nucl. Med. 36(3), 212–227 (2006). doi:10.1053/j.semnuclmed.2006.03.004
F. Donadio, V. Morelli, A.S. Salcuni, C. Eller-Vainicher, M. Carletto, M. Castellani, L. Dellavedova, A. Scillitani, P. Beck-Peccoz, I. Chiodini, Role of adrenal gland scintigraphy in patients with subclinical hypercortisolism and incidentally discovered adrenal mass. J. Endocrinol. Invest. 32(7), 576–580 (2009). doi:10.3275/6360
G. Di Dalmazi, R. Pasquali, F. Beuschlein, M. Reincke, Subclinical hypercortisolism: a state, a syndrome, or a disease?. Eur. J. Endocrinol. 173(4), M61–71 (2015). doi:10.1530/EJE-15-0272
J. Newell-Price, P. Trainer, L. Perry, J. Wass, A. Grossman, M. Besser, A single sleeping midnight cortisol has 100% sensitivity for the diagnosis of Cushing’s syndrome. Clin. Endocrinol. 43(5), 545–550 (1995)
F. Pecori Giraldi, A.G. Ambrogio, M. De Martin, L.M. Fatti, M. Scacchi, F. Cavagnini, Specificity of first-line tests for the diagnosis of Cushing’s syndrome: assessment in a large series. J. Clin. Endocrinol. Metab. 92(11), 4123–4129 (2007). doi:10.1210/jc.2007-0596
J. Shen, M. Sun, B. Zhou, J. Yan, Nonconformity in the clinical practice guidelines for subclinical Cushing’s syndrome: which guidelines are trustworthy?. Eur. J. Endocrinol. 171(4), 421–431 (2014). doi:10.1530/EJE-14-0345
M. Terzolo, A. Stigliano, I. Chiodini, P. Loli, L. Furlani, G. Arnaldi, G. Reimondo, A. Pia, V. Toscano, M. Zini, G. Borretta, E. Papini, P. Garofalo, B. Allolio, B. Dupas, F. Mantero, A. Tabarin, Italian Association of Clinical, E.: AME position statement on adrenal incidentaloma. Eur. J. Endocrinol. 164(6), 851–870 (2011). doi:10.1530/EJE-10-1147
C. Eller-Vainicher, V. Morelli, A.S. Salcuni, M. Torlontano, F. Coletti, L. Iorio, A. Cuttitta, A. Ambrosio, L. Vicentini, V. Carnevale, P. Beck-Peccoz, M. Arosio, B. Ambrosi, A. Scillitani, I. Chiodini, Post-surgical hypocortisolism after removal of an adrenal incidentaloma: is it predictable by an accurate endocrinological work-up before surgery?. Eur. J. Endocrinol. 162(1), 91–99 (2010). doi:10.1530/EJE-09-0775
S. Kidambi, H. Raff, J.W. Findling, Limitations of nocturnal salivary cortisol and urine free cortisol in the diagnosis of mild Cushing’s syndrome. Eur. J. Endocrinol. 157(6), 725–731 (2007). doi:10.1530/EJE-07-0424
K.I. Alexandraki, A.B. Grossman, Is urinary free cortisol of value in the diagnosis of Cushing’s syndrome?. Curr. Opin. Endocrinol. Diabetes Obes. 18(4), 259–263 (2011). doi:10.1097/MED.0b013e3283487193
N. Krone, B.A. Hughes, G.G. Lavery, P.M. Stewart, W. Arlt, C.H. Shackleton, Gas chromatography/mass spectrometry (GC/MS) remains a pre-eminent discovery tool in clinical steroid investigations even in the era of fast liquid chromatography tandem mass spectrometry (LC/MS/MS). J. Steroid Biochem. Mol. Biol. 121(3-5), 496–504 (2010). doi:10.1016/j.jsbmb.2010.04.010
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Prete, A., Paragliola, R.M., Bottiglieri, F. et al. Factors predicting the duration of adrenal insufficiency in patients successfully treated for Cushing disease and nonmalignant primary adrenal Cushing syndrome. Endocrine 55, 969–980 (2017). https://doi.org/10.1007/s12020-016-1007-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-016-1007-5