Abstract
The aim of this study was to evaluate the effect of a six-month lifestyle intervention on ghrelin and asymmetrical dimethylarginine (ADMA) in obese Mexican adolescents. A total of 65 obese Mexican adolescents aged 10–16 years completed a six-month lifestyle intervention. Anthropometric and biochemical parameters were assessed at baseline and at six months. Twenty normal-weight adolescents were also evaluated at baseline. Insulin resistance (IR) was determined by the homeostasis model assessment of IR (HOMA-IR). Ghrelin and ADMA were determined by enzyme-linked immunosorbent assay. Obese adolescents presented significantly higher triglycerides, cholesterol, glucose, insulin, HOMA-IR, and ADMA levels, while ghrelin was significantly lower. The lifestyle intervention led to a significant improvement in HOMA-IR, ghrelin, and ADMA in the whole studied obese subjects. ADMA and ghrelin levels were associated with BMI and IR components. According to the value of HOMA-IR, the obese subjects were divided into subjects with or without IR, no difference in ghrelin and ADMA was observed in these two subgroups. After intervention, the obese with IR showed increased ghrelin and decreased ADMA, while the obese without IR only showed improvement in ghrelin. The multiple linear regression analysis revealed that the changes of systolic blood pressure were the only predictor for the changes of ghrelin in the obese with IR. Our study demonstrated the increase of ADMA and the decrease of ghrelin in obese adolescents. Lifestyle intervention improved insulin resistance, decreased ADMA, and increased ghrelin in obese subjects with IR although no significant weight loss was observed.
Similar content being viewed by others
Introduction
Ghrelin, a 28-amino acid peptide predominantly produced by the stomach, is expressed in many other central and peripheral tissues including hypothalamus, liver, kidney, pituitary gland, endocrine pancreas, and adipose tissue [1, 2]. Ghrelin is involved in the control of food intake and energy metabolism at central levels as well as at peripheral levels influencing the endocrine pancreatic function and glucose and lipid metabolism [3, 4]. In humans, circulating levels of ghrelin are increased in anorexia and cachexia, but are reduced in obesity [4–6]. Recently, ghrelin levels have been postulated to be related to insulin resistance [5, 7] although some other studies have not confirmed this relationship [8, 9].
Although the majority of the studies have demonstrated that ghrelin concentrations are decreased in obese subjects [4, 5, 10, 11], the effect of lifestyle intervention on ghrelin concentrations was reported controversially. Some studies have reported an increase in ghrelin concentrations [10, 12, 13], whereas other studies have found no change in ghrelin concentrations [11, 13–16].
The methylated l-arginine metabolite asymmetrical dimethyl-l-arginine (ADMA) is a competitive NO synthase antagonist. It has been speculated that the increased levels of ADMA could reduce NO formation and influence vascular function. The plasma concentrations of ADMA could therefore be used to monitor early changes in the l-arginine/NO metabolism and endothelial dysfunction. The increased ADMA concentrations have been described in hypercholesterolemia [17], hypertension [18], arterial occlusive disease [19], and type 2 diabetes [20].
Data of ADMA in childhood are very rare. ADMA may play a pathophysiologic role in hypertension, as elevated ADMA plasma levels were found in hypertensive children [21, 22]. Previous study has been proposed that ghrelin has a beneficial effect on vasculature [23], it is logical to speculate the association between the decreased ghrelin and increased ADMA in obese adolescents. The aims of this study were to (1) compare ADMA and ghrelin concentrations between obese and normal-weight children, (2) analyze the effect of six-month lifestyle intervention on ADMA and ghrelin levels, and (3) evaluate the relationships between ghrelin, ADMA, and insulin resistance.
Methods and subjects
Subjects
Obese adolescents were consecutively recruited in Hospital Infantíl de México Federico Gómez. Obesity was defined as body mass index (BMI) in excess of the 95 percentile according to age and sex (using the percentile charts of the Center for Disease Control and Prevention for the assessment of somatic development in children and adolescents) [24]. Normal-weight adolescents (10 < BMI < 85 percentile) were invited from obese subject’s friends including their classmates. Children with endocrine disorders, familial hyperlipidemia, hypertension, diabetes, and pharmacological treatment were excluded from the study. The study protocol was approved by the Committee for Ethics and Control of Hospital Infantil de México Federico Gómez. Parents and children were informed as to the nature and purpose of the study. Parents gave their written informed consent. Children gave their consent verbally.
Overview of the protocol
All participants for the study were asked to fill out a questionnaire concerning their eating and exercise habits. Body weight was measured with only minimal clothing (in underwear) to the nearest 0.1 kg using a calibrated balance scale. Height was measured to the nearest centimeter using a rigid stadiometer. BMI was calculated as body weight in kilograms divided by the square of height in meters. As the mean ages in the obese and control groups were matched, the standard deviation scores (SDS)-BMI were not calculated. Blood pressure was measured according to the guidelines of the National High Blood Pressure Education Program. Systolic and diastolic blood pressures were measured twice at the right arm after a 10-min rest in the supine position using a calibrated sphygmomanometer and then averaged. Heart rate was measured by finding the pulse of the body in triplicate expressed as beats/minute. Waist circumference was measured at a level midway between the lower rib margin and iliac crest with the tape all around the body in horizontal position.
For analysis, 10 mL of blood was taken from the left cubital vein, which was a morning sample taken before breakfast (from 8:00 am to 9:00 am), after an overnight 12-h fast. The serum for ADMA analysis was frozen and kept at a temperature of −70 °C until analysis was performed. The active ghrelin molecule is extremely unstable in serum/plasma and should be rigorously protected during blood sample collection. For maximum protection, enough AEBSF was added to serum to a final concentration of 1 mg/mL. The blood was allowed to clot at room temperature for 30 min and then centrifuge. The serum were acidified with HCl to a final concentration of 0.05 N and frozen and kept at a temperature of −70 °C until analysis was performed.
The concentrations of glucose, cholesterol, and triglyceride were measured by standard enzymatic assay in our hospital’s central laboratory using standard laboratory instruments (Dimension-RXL, Dade, Behring, Germany). The concentration of insulin was determined by solid-phase, two-site chemiluminescent immunometric assay (Immulite, Diagnostic Products Corp., Los Angeles, CA, USA). The serum concentration of ADMA was determined by enzyme-linked immunosorbent assay (ELISA; Enzo Lif Sciences, Germany). The concentrations of ghrelin were measured with commercially available ELISA kits (Linco Research, USA). Insulin resistance was calculated by homeostasis model assessment: resistance (HOMA-IR) = [insulin (milliunits per liter) × glucose (millimoles per liter)]/22.5. A HOMA-IR value of 3.4 was chosen as the cutoff point to define IR. As suggested, this value corresponds to the 90th percentile of a population of healthy children; beyond it, HOMA-IR becomes a cardiovascular risk factor [25].
For all obese subjects, the protocol was repeated at 6-month intervals. The normal-weight subjects were studied only at baseline.
Lifestyle intervention
Of the total 90 obese subjects recruited, 65 subjects completed 6 months of followup with 25 losses (27.8 %). Several subjects did not continue the protocol for unspecified reasons and could not be reached for followup; several subjects were not able to continue because they changed address and lived far away from the hospital. Therefore, the baseline values of only 65 subjects, who completed intervention, were presented and compared with normal-weight healthy subjects.
All the participants with obesity attended a 24-week lifestyle intervention program, which was directed by a registered nutritionist and under the medical supervision of a physician. Compliance with the lifestyle changes was achieved by a combination of good dietary practices, physical activity, behavioral counseling (in consultation with a clinical psychologist), and active involvement of the family. During the course, participants received diet instruction and physical training once a week.
The parents of the adolescents participated in 4 intensive lifestyle support sessions (once a week in the first month), then 1 monthly 15-minute individual telephone session. These sessions focused on lifestyle knowledge and skills including the following: family-focused healthy eating with specific core food serve recommendations, monitoring, label reading, snacks, modifying recipes, being active in a variety of ways, roles and responsibilities around eating, managing appetite, self-esteem, and teasing [26].
The main aim of obesity treatment is to achieve an ideal weight for a given height and at the same time insuring the required supply of nutrients to avoid interfering with growth. Moderate obesity requires nutritional intervention with a low-calorie diet calculated on the basis of age and aimed at maintaining body weight while not impairing growth, thus achieving a decrease in BMI. Severe obesity may require restriction of the diet to 20 % of the diet recommended for a healthy age- and sex-matched child. The nutrition counseling was based on healthy food selections, emphasizing reduced carbohydrate and fat consumption. The objectives were to reduce dietary fat, as well as sugar-based carbonated drink intake, together with increase in vegetables and fruits with rich fiber.
The subjects were advised to perform brisk walking for 30 min daily during the first two weeks. Thereafter, the duration of activity was progressively increased to one hour by the third week. Participants were also encouraged to undertake moderate–intense physical activity (cycling, jogging, and swimming) at least 5 times per week in addition to the daily walking.
Statistical analysis
Statistical analysis was performed by means of the computer program SPSS 17.0. The unpaired Student’s t test and the Mann–Whitney U test were used for variables normally distributed or not normally distributed, respectively. The data are presented as means with standard deviations. Baseline and post-intervention values were compared by the paired t test or the Wilcoxon signed ranks test variables with distributions significantly deviating from normal. Correlation between new and traditional risk factors at baseline in the whole study groups was analyzed by Pearson. Reduced multiple linear regression model was performed in obese with IR. Changes of variables after intervention (Δ) = values after 6-month intervention − values at baseline. All P value resulted from 2-side statistical tests and <0.05 was considered statistically significant.
Results
General characteristics of the study population at baseline
The physical characteristics and the main laboratory variables in the study groups are shown in Table 1. Compared with normal-weight adolescents, obese adolescents had significantly higher levels of weight, BMI, diastolic blood pressure, higher levels of glucose, triglycerides, total cholesterol, insulin, and HOMA-IR. It showed that obese group presented significantly higher levels of ADMA and lower levels of ghrelin in comparison with normal-weight subjects (Table 1).
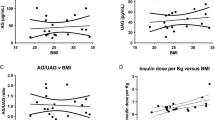
Correlation among variables in all participants at baseline
Pearson analysis was performed in all studied subjects at baseline. The values of ADMA associated significantly with BMI, glucose, insulin, and HOMA (Table 2). Ghrelin associated with weight, BMI, glucose, insulin, and HOMA in negative way (Table 2). Ghrelin values also associated negatively with systolic and diastolic blood pressure (r = −0.26, P = 0.032 and r = −0.25, P = 0.036, respectively).
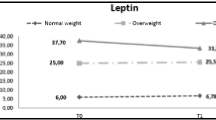
Effect of six-month lifestyle intervention in all obese adolescents
After six-months of lifestyle intervention, although no significant weight loss was observed in the studied obese adolescents, the obese subjects displayed slight but significant drops in glucose, insulin, and HOMA-IR with respect to baseline levels. Circulating concentrations of ADMA showed significant decreases after 6-month intervention. The levels of ghrelin were increased significantly after intervention. No changes in triglycerides and total cholesterol were observed after intervention (Table 1).
The characteristics of the obese with or without IR at baseline and after intervention
According to the value of HOMA-IR, the obese adolescents were divided into two subgroups: obese with insulin resistance (HOMA ≥ 3.4, n = 21, 32.3 %) and the obese without insulin resistance (HOMA < 3.4, n = 44, 67.7 %). The obese with IR showed higher DBP, triglycerides, glucose, insulin, and HOMA compared with those without IR at baseline. No statistical difference in ghrelin and ADMA was observed in these two obese subgroups at baseline although the levels of ghrelin in the obese with IR showed numerically lower than that in the group without IR (Table 3).
After six-month lifestyle intervention, the obese with IR showed improvement in insulin and HOMA-IR, significant increase in ghrelin and diminish in ADMA. In the obese without IR, the levels of ghrelin were also observed increased significantly; however, no change in ADMA was observed after 6-month intervention (Table 3).
The correlation between the changes in ADMA or ghrelin and the changes in others variables in obese adolescents
Pearson analysis was performed to evaluate the correlation between changes in ADMA or ghrelin and changes in anthropometric parameters, metabolic profile, and HOMA-IR in the obese with IR or without IR. It demonstrated that the change of ghrelin was associated negatively with BMI, systolic blood pressure, and diastolic blood pressure in the obese with IR (Table 4). In the obese without IR, the only association observed was changes between in ghrelin and in heart rate. No significant correlation was displayed between changes in ADMA and in ghrelin (Table 4).
The reduced multiple linear regression analysis was performed in the obese with IR. In this analysis, the changes in ghrelin were verified as dependent variable and changes in BMI, SBP, or DBP as independent variables. As a result, the changes in ghrelin sustained dependence on changes in SBP significantly (P = 0.022). The changes in BMI, SBP, and DBP contributed to 43.7 % of the variance in changes in ghrelin (Table 5).
Discussion
To our knowledge, this is the first study assessing the impact of lifestyle intervention on ghrelin and ADMA in obese Mexican adolescents aged 10–16 years. In the present study, improved insulin resistance, increased ghrelin, and decreased ADMA concentrations were observed in obese adolescents although no significant weight loss was achieved after six-month lifestyle intervention. In obese subjects with IR, the changes in ghrelin were very sensitive to the changes of systolic blood pressure. Furthermore, no correlation was observed between ghrelin and ADMA in studied subjects.
As described by our previous studies [27] and others [28, 29], our obese adolescents presented several cardiometabolic risk factors, namely dyslipidemia, dysglicemia, higher blood pressure, and IR. Weight loss induced by lifestyle intervention or surgery could improve insulin resistance and metabolic syndrome, which was consistent with our present results [27, 30, 31].
The baseline levels from the present study on ghrelin were in concordance with some recent studies in obese children [14, 28]. However, the levels of ghrelin vary very much in previous studies in children—the average values were from 260 to 2,700 pg/mL [11, 32, 33]. It is to note that the active ghrelin molecule is extremely unstable in serum/plasma and should be rigorously protected during blood sample collection; neat samples without treatment with AEBSF and acidification exhibit approximate 30 % less total ghrelin content than samples which have been protected. Thus, care should be taken to minimize confounding factors on blood collection. Moreover, a recent study showed that overweight European Americans displayed higher circulating ghrelin and greater ghrelin suppression compared to African Americans, indicating that ghrelin differs with ethnicity [34]. Further study is warranted to explore the physiologic basis for these ethnic differences.
Ghrelin levels showed an increase in response to lifestyle intervention in the current study and this enhancement almost reached to its normal levels in lean control subjects. Previous studies have also reported similar increases in ghrelin levels associated with lifestyle intervention [33]. However, results about the association of changes in ghrelin levels and long-term weight changes are controversial. A study that examined the effects of a 3-month energy deficit-imposing diet and exercise intervention on circulating ghrelin in normal-weight healthy women showed that ghrelin exhibited particular sensitivity to changes in body weight and responded in a compensatory manner to changes in energy homeostasis [35]. In current study, the obese subjects who underwent the intervention were only able to maintain body weight and there was no apparent weight loss. Because ghrelin is produced primarily in the stomach, there may not be any strong direct link between this stomach hormone and changes in adipose tissue mass and/or number due to lifestyle intervention. It also suggested that changes in ghrelin may be most sensitive to changes elicited by overall energy deficit from dietary changes and nutritional changes since the secretion of ghrelin is very sensitive to diet composition [11], which was also indicated by our current study since the increased ghrelin levels have been observed in the obese with or without IR in the absence of a reduction in body weight after lifestyle intervention.
Glucose and insulin metabolism appear to be profoundly involved in the regulation of ghrelin levels as inverse relationships between this satiety factor and indexes of insulin resistance in both adults and children have been reported [36, 37]; however, other studies in obese children did not report such negative association [8, 32]. In the present study, the weak negative relationship between fasting ghrelin concentration and insulin resistance was observed in the whole studied subjects; however, such relationship did not remain between the changes in this satiety factor and HOMA-IR in obese subjects with or without IR after six-month lifestyle intervention. Studies have suggested that acylated ghrelin is deferentially associated with insulin sensitivity in metabolic syndrome [38] and responds differently to lifestyle intervention compared with total ghrelin [39]. In the present study, we measured the total circulating ghrelin and could not specifically measure its different forms. Therefore, any effect of the intervention on the different forms of ghrelin cannot be ruled out. It is unclear whether the small sample size may also be contributed to the lack of the association after lifestyle intervention.
It has been proposed that ghrelin has a beneficial effect on vasculature, since intravenous ghrelin injections decrease mean arterial BP and cardiac afterload in adults [25]. Few studies have assessed the association between ghrelin and blood pressure. Pedrosa et al. [28] reported inverse association between ghrelin and systolic blood pressure in obese children. In our present study, the moderate inverse association was observed between increased ghrelin and decreased systolic blood pressure in obese children with IR; it was confirmed by the multiple linear regression analysis. Such association indicated that low ghrelin levels in obese children particularly those with IR may promote the development of CVD.
Recently, ADMA is considered as a predictor of cardiovascular events and a sensitive marker for cardiovascular risk. In the current study, the levels of ADMA were slightly, but significantly, elevated in obese adolescents, which was in line with the previous studies in children and adults [40–42]. Further analysis revealed a weak positive correlation between ADMA and BMI and insulin resistance in the whole studied groups. However, no difference in ADMA was observed between obese adolescents with or without IR. The previous data assessing the association between ADMA and insulin resistance are controversial. A study in juveniles did not find correlation between ADMA and parameter of the lipid metabolism involving cholesterol, triglycerides, insulin, and glucose [40]. However, another study in obese insulin-resistant women demonstrated a significant association between the decline in insulin resistance and the fall in ADMA concentration after weight loss [43]. The different subjects involved in these studies (adolescents or adults) should be taken in consideration.
In the current study, we showed that lifestyle intervention with concurrent enhancement of insulin sensitivity leads to a slight, but significant, decline in ADMA concentration in obese with IR. The reduction of ADMA contributes significantly to the restored endothelial function [43]. Since ADMA is an endogenous eNOS inhibitor, thereby reducing levels of ADMA would restore the endothelial NO production, the main reason for impaired endothelial function. However, recent study in severe obesity assessing biochemical and clinical measurement of endothelial function did not show a significant influence of ADMA reduction on endothelial restoration [41]. The exact mechanism of ADMA involved in endothelial function remains further investigation.
We expected the possible correlation between ghrelin and ADMA because ghrelin was reported beneficial effect on vasculature, and ADMA is an endogenous inhibitor of endothelial nitric oxide synthase, which was associated with vascular function. To our knowledge, it is the first study assessing the possible correlation between the satiety hormone and biomarker of endothelial function. It is surprising that no association was observed between these two factors in our studied subjects before and after intervention. A possible explanation for the missing correlation in the present study derived from the fact that alterations of ADMA and ghrelin in obese adolescents were slight compared with normal-weight control, 38.8 and 18 %, respectively. On the other hand, the small sample size would be contributed to the missing correlation. The mechanism on regulating vascular function involved by ADMA and ghrelin and the possible relationship between these two factors needs further investigation.
One limitation of our study was clearly provided by the small number of patients included in this trial. Therefore, we might have missed the relationship between ADMA and ghrelin. Another limitation was that no significant weight loss was observed induced by six-month lifestyle intervention, which may mask the association between reduced ADMA or increased ghrelin and ameliorated IR.
In summary, our present study demonstrated increased ADMA and decreased ghrelin in obese adolescents. Lifestyle intervention improved insulin resistance, decreased ADMA, and increased ghrelin in obese subjects with IR although no significant weight loss was observed. The pressing question is if these beneficial changes can indeed be sustained for a longer period preventing the progression of obesity and the culmination into overt cardiovascular diseases.
References
A.J. Van der Lely, M. Tschop, M.L. Heiman, E. Ghigo, Biological, physiological, pathophysiological, and pharmacological aspects of ghrelin. Endocr. Rev. 25, 426–457 (2004)
M. Kojima, H. Hosoda, Y. Date, M. Nakazato, H. Matsuo, K. Kangawa, Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature 402, 656–660 (1999)
P. Wiedmer, R. Nogueiras, F. Broglio, D. D’Alessio, M.H. Tschop, Ghrelin, obesity and diabetes. Nat. Clin. Pract. Endocrinol. Metab. 3, 705–712 (2007)
M. Tschöp, C. Weyer, P.A. Tataranni, V. Devanarayan, E. Ravussin, M.L. Heiman, Circulating ghrelin levels are decreased in human obesity. Diabetes 50, 707–709 (2001)
A. Ikezaki, H. Hosoda, K. Ito, S. Iwama, N. Miura, H. Matsuoka, C. Kondo, M. Kojima, K. Kangawa, S. Sugihara, Fasting plasma ghrelin levels are negatively correlated with insulin resistance and PAI-1, but not with leptin, in obese children and adolescents. Diabetes 51, 3408–3411 (2002)
T. Shiiya, M. Nakazato, M. Mizuta, Y. Date, M.S. Mondal, M. Tanaka, S. Nozoe, H. Hosoda, K. Kangawa, S. Matsukura, Plasma ghrelin levels in lean and obese humans and the effect of glucose on ghrelin secretion. J. Clin. Endocrinol. Metab. 87, 240–244 (2002)
R.S. Ahima, Ghrelin—a new player in glucose homeostasis? Cell Metab. 3, 301–302 (2006)
S. Bellone, N. Castellino, F. Broglio, A. Rapa, D. Vivenza, G. Radetti, J. Bellone, C. Gottero, E. Ghigo, G. Bona, Ghrelin secretion in childhood is refractory to the inhibiting effect of feeding. J. Clin. Endocrinol. Metab. 89, 1662–1665 (2004)
K.M. Choi, J. Lee, K.W. Lee, J.A. Seo, J.H. Oh, S.G. Kim, D.S. Choi, S.H. Baik, The associations between plasma adiponectin, ghrelin levels, and cardiovascular risk factors. Eur. J. Endocrinol. 150, 715–718 (2004)
L. Soriano-Guillen, V. Barrios, A. Campos-Barros, J. Argente, Ghrelin levels in obesity and anorexia nervosa: effect of weight reduction or recuperation. J. Pediatr. 144, 36–42 (2004)
T. Reinehr, C.L. Roth, U. Alexy, M. Kersting, W. Kiess, W. Andler, Ghrelin levels before and after reduction of overweight due to a low fat high carbohydrate diet in obese children and adolescents. Int. J. Obes. 29, 362–368 (2005)
D.G. Haider, K. Schindler, G. Prager, A. Bohdjalian, A. Luger, M. Wolzt, B. Ludvik, Serum retinol-binding protein-4 is reduced after weight loss in morbidly obese subjects. J. Clin. Endocrinol. Metab. 92, 1168–1171 (2007)
D.E. Cummings, D.S. Weigle, R.S. Frayo, P.A. Breen, M.K. Ma, E.P. Dellinger, J.Q. Purnell, Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N. Engl. J. Med. 346, 1623–1630 (2002)
T. Reinehr, G. de Sousa, L.R. Christian, Obestatin and ghrelin levels in obese children and adolescents before and after reduction of overweight. Clin. Endocrinol. 68, 304–310 (2008)
J.M. Garcia, D. Iyer, W.C.S. Posten, M. Marcelli, R. Reeves, J. Foreyt, A. Balasubramanyam, Rise of plasma ghrelin with weight loss is not sustained during weight maintenance. Obesity 14, 1716–1723 (2006)
D.S. Weigle, D.E. Cummings, P.D. Newby, P.A. Breen, R.S. Frayo, C.C. Matthys, H.S. Callahan, J. Purnell, Roles of leptin and ghrelin in the loss of body weight caused by a low fat, high carbohydrate diet. J. Clin. Endocrinol. Metab. 88, 1577–1586 (2003)
R.H. Böger, S.M. Bode-Böger, A. Szuba, P.S. Tsao, J.R. Chan, O. Tangphao, T.F. Blaschke, J.P. Cooke, Asymmetric dimethylarginine (ADMA): a novel risk factor for endothelial dysfunction: its role in hypercholesterolemia. Circulation 98, 1842–1847 (1998)
H. Matsuoka, S. Itoh, M. Kimoto, K. Kohno, O. Tamai, Y. Wada, H. Yasukawa, G. Iwami, S. Okuda, T. Imaizumi, Asymmetrical dimethylarginine, an endogenous nitric oxide synthase inhibitor, in experimental hypertension. Hypertension 29, 242–247 (1997)
R.H. Böger, S.M. Bode-Böger, W. Thiele, W. Junker, K. Alexander, J.C. Frolich, Biochemical evidence for impaired nitric oxide synthesis in patients with peripheral arterial occlusive disease. Circulation 95, 2068–2074 (1997)
F. Abbasi, T. Asagmi, J.P. Cooke, C. Lamendola, T. McLaughlin, G.M. Reaven, M. Stuehlinger, P.S. Tsao, Plasma concentrations of asymmetric dimethylarginine are increased in patients with type 2 diabetes mellitus. Am. J. Cardiol. 88, 1201–1203 (2001)
C.D. Goonasekera, D.D. Rees, P. Woolar, Nitric oxide synthase inhibitors and hypertension in children and adolescents. J. Hypertens. 15, 901–909 (1997)
C.D. Goonasekera, V. Shah, D.D. Rees, M.J. Dillon, Nitric oxide activity in childhood hypertension. Arch. Dis. Child. 77, 11–16 (1997)
N. Nagaya, M. Kojima, M. Uematsu, Hemodynamic and hormonal effects of human ghrelin in healthy volunteers. Am. J. Physiol. Regul. Integr. Comp. Physiol. 280, R1483–R1487 (2001)
R.J. Kuczmarski, C.L. Ogden, L.M. Grummer-Strawn, K.M. Flegal, S.S. Guo, R. Wei, Z. Mei, L.R. Curtin, A.F. Roche, C.L. Johnson, CDC growth charts: United States. Adv. Data 314, 1–28 (2000)
B. García-Cuartero, C. García-Lacalle, C. Jiménez-Lobo, A. González-Vergaz, C. Calvo-Rey, M.J. Alcázar-Villar, E. Díaz-Martínez, Indice HOMA y QUICKI, insulina y peptido C en ninos sanos. Puntos de corte de riesgo cardiovascular. An. Pediatr. (Barc) 66, 481–490 (2007)
R.K. Golley, A.M. Magarey, L.A. Baur, K.S. Steinbeck, L.A. Daniels, Twelve-month effectiveness of a parent-family-focused weight-management program for prepubertal children: a randomized controlled trial. Pediatrics 119, 517–525 (2007)
F.Y. Huang, B. Del-Río-Navarro, G. Toussaint Martínez de Castro, S. Torres-Alcántara, J.J.J. Siera-Monge, J.A. Pérez-Ontiveros, E. Navarro-Olivos, M. Figueroa-Barron, A. Reyes-Lopéz, S. Villafaña, E. Hong, Weight loss induced by 6-month lifestyle intervention improves early endothelial activation and fibrinolysis in obese adolescents. Child Care Health. Dev. 37, 377–384 (2011)
C. Pedrosa, B.M.P.M. Oliveira, I. Albuquerque, C. Simões-Pereira, M.D. Vaz-de-Almeida, F. Correia, Metabolic syndrome, adipokines and ghrelin in overweight and obese schoolchildren: results of a 1-year lifestyle intervention programme. Eur. J. Pediatr. 170, 483–492 (2011)
M.P. Bahíllo-Curieses, F. Hermoso-López, M.J. Martínez-Sopena, P. Cobreros-García, P. García-Saseta, M. Tríguez-García, J.M. Marugán-Miguelsanz, Prevalence of insulin resistance and impaired glucose tolerance in a sample of obese Spanish children and adolescents. Endocrine 41, 289–295 (2012)
C. Gazzaruso, S. Giordanetti, A. La Manna, M. Celsa, E. De Amici, C. Turpini, A. Catona, P. Fratino, Weight loss after Swedish Adjustable Gastric Banding: relationships to insulin resistance and metabolic syndrome. Obes. Surg. 12, 841–845 (2002)
L. Velázquez-López, E. González-Figueroa, P. Medina-Bravo, I. Pineda-del Aguila, L. Ávila-Jiménez, R. Ramos-Hernández, M. Klunder-Klunder, J. Escobedo-de la Peña, Low calorie and carbohydrate diet: to improve the cardiovascular risk indicators in overweight or obese adults with prediabetes. Endocrine (2012). doi:10.1007/s12020-012-9775-z
P. Balagopal, S.S. Gidding, L.M. Buckloh, H.N. Yarandi, J.E. Sylvester, D.E. George, V.L. Funanage, Changes in circulating satiety hormones in obese children: a randomized controlled physical activity-based intervention study. Obesity 18, 1747–1753 (2010)
R. Kelishadi, M. Hashemipour, N. Mohammadifard, H. Alikhassy, K. Adeli, Short- and long-term relationships of serum ghrelin with changes in body composition and the metabolic syndrome in prepubescent obese children following two different weight loss programmes. Clin. Endocrinol. 69, 721–729 (2008)
A.C. Ellis, P. Chandler-Laney, K. Casazza, L.L. Goree, B.A. Gower, Effects of habitual diet on ethnic differences in serum total ghrelin. Endocrine (2012). doi:10.1007/s12020-012-9667-2
H.J. Leidy, J.K. Gardner, B.R. Frye, M.L. Snook, M.K. Schuchert, E.L. Richard, N.I. Williams, Circulating ghrelin is sensitive to changes in body weight during a diet and exercise program in normal-weight young women. J. Clin. Endocrinol. Metab. 89, 2659–2664 (2004)
F. Bacha, S.A. Arslanian, Ghrelin suppression in overweight children: a manifestation of insulin resistance? J. Clin. Endocrinol. Metab. 90, 2725–2730 (2005)
T. McLaughlin, F. Abbasi, C. Lamendola, R.S. Frayo, D.E. Cummings, Plasma ghrelin concentrations are decreased in insulin-resistant obese adults relative to equally obese insulin-sensitive controls. J. Clin. Endocrinol. Metab. 89, 1630–1635 (2004)
R. Barazzoni, M. Zanetti, C. Ferreira, Relationships between desacylated and acylated ghrelin and insulin sensitivity in the metabolic syndrome. J. Clin. Endocrinol. Metab. 92, 3935–3940 (2007)
H.J. Kim, S. Lee, T.W. Kim, Effects of exercise-induced weight loss on acylated and unacylated ghrelin in overweight children. Clin. Endocrinol. (Oxf) 68, 416–422 (2008)
H.-J. Gruber, C. Mayer, A. Meinitzer, G. Almer, R. Horejsi, R. Möller, S. Pilz, W. März, R. Gasser, M. Truschnig-Wilders, H. Mangge, Asymmetric dimethylarginine (ADMA) is tightly correlated with growth in juveniles without correlations to obesity related disorders. Exp. Clin. Endocrinol. Diabetes 116, 520–524 (2008)
G. Rudofsky, E. Roeder, T. Merle, M. Hildebrand, P.P. Nawroth, C. Wolfrum, Weight loss improves endothelial function independently of ADMA reduction in severe obesity. Horm. Metab. Res. 43, 343–348 (2011)
K. Krzyzanowska, F. Mittermayer, H.-P. Kopp, M. Wolzt, G. Schernthaner, Weight loss reduces circulating asymmetrical dimethylarginine concentrations in morbidly obese women. J. Clin. Endocrinol. Metab. 89, 6277–6281 (2004)
T. McLaughlin, M. Stühlinger, C. Lamendola, F. Abbasi, J. Bialek, G.M. Reaven, P.S. Tsao, Plasma asymmetric dimethylarginine concentrations are elevated in obese insulin-resistant women and fall with weight loss. J. Clin. Endocrinol. Metab. 91, 1896–1900 (2006)
Acknowledgments
We thank Emma Guadalupe Gazcón Morales, Daniel Chavez Vazquez, and Sergio Arturo Mavil Cortes for help with blood sample collection and laboratory measures. This work was supported by Grants (HIM/2007/008 and HIM/2008/007) from Hospital Infantíl de México Federico Gómez.
Conflict of interest
The authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huang, F., del-Río-Navarro, B.E., Pérez Ontiveros, J.A. et al. Changes in ghrelin and asymmetrical dimethylarginine in obese Mexican adolescents after six-month lifestyle intervention. Endocrine 43, 603–610 (2013). https://doi.org/10.1007/s12020-012-9808-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-012-9808-7