Abstract
The critical asthma syndrome (CAS) encompasses the most severe, persistent, refractory asthma patients for the clinician to manage. Personalized pharmacotherapy is necessary to prevent the next acute severe asthma exacerbation, not just the control of symptoms. The 2007 National Asthma Education and Prevention Program Expert Panel 3 provides guidelines for the treatment of uncontrolled asthma. The patient’s response to recommended pharmacotherapy is highly variable which risks poor asthma control leading to frequent exacerbations that can deteriorate into CAS. Controlling asthma symptoms and preventing acute exacerbations may be two separate clinical activities with their own unique demands. Clinicians must be prepared to use the entire spectrum of asthma medications available but must concurrently be aware of potential drug toxicities some of which can paradoxically worsen asthma control. Medications normally prescribed for COPD can potentially be useful in the CAS patient, particularly those with asthma-COPD overlap syndrome. Immunomodulation with drugs like omalizumab in IgE-mediated asthma syndromes is one important approach. New and emerging drugs address unique aspects of airway inflammation and biology but at a significant financial cost. The pharmacology and toxicities of the agents that may be used in the treatment of CAS to control asthma symptoms and prevent severe exacerbations are reviewed.
Similar content being viewed by others
Introduction
The critical asthma patient can be a challenge for the emergency department (ED), the intensive care unit, the hospital floor, and the outpatient clinic. They represent the sickest of asthma patients, have very frequent exacerbations (>3/year), may have symptoms throughout the day, require large dosages of medications, and have high healthcare utilization and expenses.
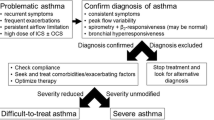
The critical asthma syndrome (CAS) defines a group of patients with frequent severe exacerbations or recent life-threatening asthma events including near-fatal asthma or status asthmaticus. Typically, these patients have very poorly controlled symptoms and are “severe persistent asthma” patients defined under the Global Initiative for Asthma (GINA) guidelines [1] and the 2007 National Asthma Education and Prevention Program (NAEPP) Expert Panel 3 guidelines [2]. There are patients who have “severe intermittent asthma” who present with occasional severe exacerbation or CAS who otherwise are well controlled. Many other terms have been used to describe these challenging patients including “severe asthma,” “difficult-to-control asthma,” and “refractory asthma,” but these terms apply more to the difficulty in controlling symptoms [3, 4]. In addition to these traditional severity classifications of asthma, efforts have been made to define asthma phenotypes and endotypes using varying degrees of clinical, physiological, and biological complexities and to link these classifications to treatment effectiveness [3, 5]. A recently described phenotype, the asthma-chronic obstructive pulmonary disease (COPD) overlap syndrome (ACOS) [6–10], describes atopic smokers who often experience very frequent and severe exacerbations at an earlier age than typical COPD patients. Many of these patients have refractory symptoms and also fall into a CAS group.
Several guidelines for the treatment of asthma exist, including the GINA, NAEPP Expert Panel 3, and the Canadian Thoracic Society-2010 [1, 2, 11]. Our review will focus on medications for adults with asthma approved by the Federal Drug Administration (FDA) and those medications not specifically approved for asthma but with evidence to support off-label use in patients who experienced CAS. The paper will concentrate on established, new/experimental, and controversial medications that may be tried in treating CAS. The goals of treatment include reducing the frequency of exacerbations, modulating airway remodeling, and improving the quality of life of asthma patients, while minimizing adverse drug events and maximizing patient safety.
Short-Acting Beta2 Agonists
The use of inhaled short-acting beta2 agonists (SABA) as “relief” or a “rescue” medication is one of the cornerstones of current asthma guidelines [12]. In fact, the frequent use or need for SABAs is thought to indicate the need to step up treatment by increasing doses or adding another maintenance medication. No large studies have shown that SABAs can prevent acute asthma exacerbations. Available beta2 agonist bronchodilators act on the beta2 airway receptors to cause relaxation of airway smooth muscles and improve airflow most of the time thereby decreasing lung hyperinflation. SABAs are the most effective bronchodilators to promptly reverse bronchoconstriction during CAS, although they have never been FDA-approved for this purpose.
The presumed mechanism of the cellular action of SABAs is through the stimulated receptors ability to modulate intracellular adenylyl cyclase resulting in the generation of cyclic adenosine monophosphate, which then results in the activation of effector protein kinases and guanine nucleotide exchange functions [13]. Figure 1 and Tables 1 and 2 offer the chemical structure of albuterol and terbutaline and summarize the various SABA preparations currently available in the USA. Although there have been many metered-dose inhalers (MDI) that delivered SABAs over the years, most relied on chlorofluorocarbon (CFC) propellants, several of which have not been converted to the currently allowed hydrofluoralkane (HFA) propellants (Table 3). Currently, racemic albuterol and levalbuterol are the only SABAs available as MDIs using HFA propellants. Albuterol is available in combination with ipratropium bromide in a spring-driven mist inhaler. Albuterol MDI when used with a disposable spacer is not inferior to nebulized albuterol in acute asthma, but the use of the MDI/spacer was found to be more economical than the nebulizer delivery system in an inner-city adult asthma population [14] and in a meta-analysis of acute episodes of asthma in children and adults in a community settings [15].
Meta-analysis has concluded that clinical equivalence exists when albuterol is given by continuous or intermittent nebulization in the treatment of acute asthma exacerbations [16]. However, a Cochrane review of eight trials found that continuous compared with intermittent SABAs reduced admissions and improved pulmonary function without an increase in pulse rate, tremor, or a decrease in serum potassium levels in adults with severe acute asthma [17].
Meta-analysis of 34 trials evaluated regular dosing compared with as-needed SABA use in outpatient asthmatics. No consistent advantage to the regular use of a SABA was seen and the data was felt to be supportive of the current guidelines that recommend SABAs as preferred rescue medications [18].
Meta-analysis on the use of intravenous (iv) albuterol in acute asthma patients presenting to the ED concluded a lack of overall support for this route [19]. Similarly, adding iv albuterol to either nebulized albuterol or iv aminophylline lacked support in separate meta-analysis [20, 21].
Both terbutaline and albuterol are available as tablets and have resulted in bronchodilator effects in asthmatic patients [22]. Oral albuterol has led to small increases in dead-space and decreases in arterial oxygen tension in adult patients with reversible airway obstruction while increasing forced expiratory volume in 1 s (FEV1) [23]. The use of oral terbutaline improved FEV1 without changing dead-space or arterial oxygen tension. Neither increased heart rate or decreased blood pressure, but tremor was reported with both drugs [22, 23].
Controlled trials of adults with severe acute asthma found no difference between nebulized epinephrine and terbutaline in either efficacy or adverse effects [24, 25]. Both epinephrine (an alpha1, beta1, and beta2 receptor agonist) and the SABA terbutaline have been used subcutaneously for the treatment of acute severe asthma. In a double-blinded study of 20 patients with acute severe asthma, no significant difference in spirometry improvement, heart rate, blood pressure, pulus paradoxus, or continuous electrocardiograms was found between subcutaneously 0.5 mg epinephrine compared with 0.5 mg terbutaline [26]. Both pediatric and adult patients with chronic severe persistent asthma have been treated every 6 h or with continuous subcutaneous terbutaline with symptomatic improvement and reduction in regular medication requirement in small case series [27, 28]. With limited data to support its use, chronic use of subcutaneous terbutaline is not included in current severe persistent asthma guidelines.
The presence of a spirometry response to a SABA does not by itself distinguish asthma from COPD. The patient’s response to albuterol can be highly variable with some not responding to treatment and some experiencing paradoxical bronchospasm and increased bronchial hyperresponsiveness with albuterol or levalbuterol [29]. This may relate to pharmacogenetics and polymorphisms that are currently very poorly understood. The downregulation of the beta2 receptor with constant SABA stimulation in some cases can limit the usefulness of these agents by causing tachyphylaxis to manifest as decreasing responsiveness and bronchodilation efficacy. Theoretically, this can place the asthma patient at risk for acute exacerbations when they will need immediate rescue.
Tulobuterol is a new short-acting SABA available in Japan with partial beta2 agonist properties that does not appear to result in beta2 receptor downregulation [30]. A tulobuterol patch formulation has led to its use in asthma and COPD with improved compliance and spirometry results [30–32].
Genetic polymorphism that results in homozygosity for arginine (Arg/Arg) rather than the normal glycine (Gly/Gly) at aminoacid 16 in the coding region of the adrenergic beta2 receptor gene (ADB2R-B16-Arg/Arg patients) has decreased long-term response to albuterol. This results in reduced morning FEV1 determinations with regular albuterol use in the ADB2R-B16-Arg/Arg genotype patients [33–35]. Other genetic polymorphisms have been identified, which appear to alter the functional properties of the beta2 receptor that are capable of changing the responsiveness to beta2 receptor agonists [36].
In addition to paradoxical bronchospasm, other adverse effects seen with SABAs include increased heart rates, palpitations, and tachyarrhythmias. Stimulation of liver glycogenolysis resulting in elevated blood sugars and the development of hypokalemia are risk factors [13]. Ventricular arrhythmias may the first sign of hypokalemia. A dose-dependent tremor from direct beta2 receptor stimulation in the skeletal muscle is common and can be very limiting to the patient. The tremor may be more associated with hypokalemia. Direct stimulation by SABAs of the arterial beta2 receptors can result in vasodilation and hypotension that further can drive a reflex tachycardia. SABA-induced type B lactic acidosis has been reported in asthmatics and may result from many mechanisms including endogenous and exogenous hyperadrenergic state [37].
Long-Acting Beta2 Agonists
Long-acting beta2 agonists (LABAs) remain the preferred add-on drug to inhaled corticosteroids (ICS) in the NAEPP Expert Panel 3 guidelines [2] at step 3 for adults and step 4 for children ≤ 4 years old with persistent asthma [12]. LABAs are contraindicated as monotherapy for long-term asthma control. Similar recommendations for the addition of LABAs to ICS therapy in adults with persistent asthma comes at an earlier treatment stage than in children in the 2010 Canadian Thoracic Society guidelines [11]. The use of LABAs in CAS patients is solely as chronic agents and not in acute severe asthma episodes.
The mechanism of action of LABAs is also by stimulating the beta2 receptors resulting in the same intracellular changes as with SABAs with functional antagonism of airway muscles leading to relaxation. In general, LABAs do not bind with greater affinity or different receptor binding characteristics than do the SABAs [38]. The mechanism for the longer duration of action of the LABAs is not known but may be from their lipophilicity, agonist efficacy, and micro-kinetic behaviors [13, 38, 39]. This increase in duration of action leads to twice a day dosing with the oldest ones (salmeterol, arformoterol, and fomorterol) and once a day dosing with the newest ones (indacaterol and vilanterol). Patients with mild asthma have, however, been shown to develop tolerance like that seen with the use of SABAs. Tolerance has been shown with the regular use of salmeterol in patients challenged with the bronchoconstrictor effects of methacholine [40]. Tables 1 and 2 offer the various LABA-containing products and dosing intervals.
Evidence for LABAs preventing exacerbations is equivocal. Meta-analysis examining the addition of LABAs to ICS in adult persistent asthma patients found reduced asthma exacerbation rates, improved lung function and symptoms, and decreased need for SABA rescues. Another meta-analysis evaluating the use of LABAs and ICS compared with higher doses of ICS in persistent asthmatic adults (23 out of 30 clinical trials) or children [41] found improvements in FEV1, symptom-free days, and the use of SABA rescue medications in adults, but there was no difference in asthma exacerbations. There was a threefold increase in the rate of tremors with the addition of LABAs but no overall increase in adverse events. A nine study systematic reviews in children examined the addition of LABAs to ICS compared with higher doses of ICS alone and found statistically improved spirometry, less use of rescue medications, and higher short-term growth with the addition of the LABAs [42]. There was no difference in the rate of asthma exacerbations or adverse events.
When the addition of LABAs to ICS was compared with higher than twice the baseline dose of ICS in a subgroup analysis of two of the trials, the rate of asthma exacerbations was statistically reduced in the higher ICS group compared with the LABA + ICS group. Another meta-analysis of 28 studies of adding LABAs and ICS compared with ICS alone in steroid-naive asthmatic children failed to show a reduction of asthma exacerbations, but it did show a significant improvement in lung function, symptoms, and study withdrawals with the combined therapy [43]. No statistical differences in adverse events were found. In summary, the addition of LABAs to ICS in patients with asthma does not seem to reduce exacerbations but consistently improves symptoms and pulmonary function without a documented increase in adverse events.
Considering the early recognition of small increases in asthma and all-cause mortality rates with the use of LABAs in asthma studies, several postmarketing studies were required [44, 45]. Even earlier observations had suggested that SABAs, especially the removed-from-market fenoterol, were associated with an increase in risk of death [46]. The infamous SMART Trial evaluated 26,355 patients treated with the LABA salmeterol or placebo added to their usual asthma care (approximately 40 % of subjects on ICS) was terminated following an interim analysis [47]. A small but statistically significant increase in respiratory- and asthma-related deaths was seen. Subgroup analysis suggested this risk was fourfold greater in African Americans compared with Caucasian subjects. Several meta-analyses including adults and children have now been performed and suggest that there is an increased risk of severe and life-threatening asthma exacerbations and death with the use of LABA monotherapy [48–50]. It is less clear that the addition of a LABA to ICS is associated with increased risk of mortality in adults or children with persistent asthma [49, 50]. The US FDA performed its own meta-analysis examining LABA therapy without ICS to non-LABA therapy. They found an estimated 3.63/1,000 more patients treated with the LABA had significant increase in asthma-related events including death, the need for intubation, or the need for hospitalization [51]. The overall recommendation of the FDA placed in a “black box warning” was to contraindicate the use of a LABA in asthma as monotherapy, to remove LABA use in stable asthmatics, but to continue the use of a LABA with an ICS in persistent asthma patients. The risks of LABAs when used with ICS were felt to be counterbalanced by the meaningful clinical symptomatic improvements seen when they are added to ICS. LABA remain the preferred add-on drug to ICS in the 2007 NAEPP Expert Panel Report when ICS alone are ineffective in achieving asthma control.
Meta-analysis of LABAs in asthma and COPD patients found an increase in [52] sinus tachycardia, hypokalemia, and major cardiovascular events but none reached statistical significance. In addition to asthma- and cardiovascular-related events, other adverse effects reported with LABA use include increases in blood glucose levels, severe hypokalemia, and major muscle tremor.
Short-Acting Muscarinic Antagonist
Both muscarinic receptor 2 (M2) and muscarinic receptor 3 (M3) are expressed in the bronchial and tracheal smooth muscles. It is unclear exactly what the contribution of the M2 receptor is but the M3 receptor when stimulated by its parasympathetic neurotransmitter acetylcholine inhibits smooth muscle relaxation induced by beta2 agonists [53]. In addition to indirectly causing bronchial airway constriction, stimulation of the M3 receptor also causes submucosal glands to release mucus and may play a role in airway remodeling and inflammation. Inflammation can modulate and amplify cholinergic tone [53]. Ipratropium is a short-acting muscarinic receptor antagonist (SAMA) lasting about 6 h while the long-acting muscarinic receptor (LAMA) tiotropium and aclidinium slowly dissociates from and antagonizes M3 receptors lasting at least 12–24 h. Tables 1 and 2 offer the various anti-muscarinic receptor agents used in respiratory medicine and their dosing intervals. Figure 1 includes the chemical structures of these drugs. SAMA and LAMA prevent contraction of airway smooth muscles and improve airflow most of the time thereby decreasing lung hyperinflation. Not all severe asthmatics will respond to SAMA [29].
The NAEPP Expert Panel 3 did not include the SAMA ipratropium bromide in the stepwise treatment guidelines, but more recent evidence suggests an important role in pharmacotherapy. A study by Gelb et al. [54] shows that 106 adult asthmatics with moderate-to-severe airway obstruction despite treatment with ICS were randomized in a double-blind crossover study to a single MDI dose of fixed combination of albuterol + ipratropium compared with a single MDI dose of albuterol alone. The combination of albuterol + ipratropium resulted in significantly greater improvement in FEV1 and longer duration of response compared with albuterol alone.
Several guidelines for the treatment of acute severe asthma exacerbations in the ED include the use of inhaled SAMAs [2, 55]. SAMAs alone compared with either SABAs alone or SAMAs + SABAs in treating acute asthma exacerbations were less efficacious [56]. Meta-analysis of acute exacerbations in asthmatic children showed a significant improvement in lung function 60 min after a single dose of a SAMA combined with SABAs but no change in hospital admission rates [57]. This finding contrasted the observation that when multiple doses of SAMAs are combined with SABAs both significant improvement in lung function and reduced hospital admissions are seen. Another meta-analysis reviewed 32 randomized controlled trials of 3,611 patients and showed significant reductions in hospital admissions in both adults and children treated with multiple doses of SAMAs + SABAs compared with SABAs alone in acute moderate-to-severe asthma exacerbations treated in the ED. Combined treatment with SAMA + SABA also produced significant increases in spirometric function compared with a SABA alone [58]. This combined multiple-dose of a SABA + SAMA has been called first-line therapy for acute asthma exacerbations in the ED and can be effectively given by MDI or by nebulizer [59]. Currently, no combination SABA + SAMA MDI is approved for treating asthma in the USA but a spring-driven soft mist inhaler is available and approved for COPD (Table 1).
Long-Acting Muscarinic Antagonist
LAMAs for the treatment of acute asthma exacerbations are not recommended in asthma guidelines nor are they FDA-approved for an asthma indication (Table 1). Several recent studies have suggested an emerging role for LAMAs in difficult-to-control asthma patient including those with severe asthma [6, 53]. Two replicated, randomized controlled trials of asthmatic patients on LABAs and ICS showed the addition of the LAMA tiotropium significantly increased the time to first exacerbation and provided modest but clinically significant and sustained improvement in FEV1 [60]. A three-way, double-blind, triple-dummy crossover trial of 210 patients with “uncontrolled asthma” compared doubling their ICS dose with adding a LABA or LAMA (tiotropium) [61]. Adding a LAMA to ICS was superior in improving symptoms and lung function than doubling the dose of ICS in poorly controlled asthma patients. Adding a LAMA to ICS was not inferior to adding a LABA to ICS in the same patient population [61]. In a double-blind, double-dummy, and placebo-controlled study of asthmatic ADB2R-B16-Arg/Arg genotype patients who were uncontrolled on an ICS received either a LAMA or a LABA [62]. Again, tiotropium was found to be noninferior to salmeterol in morning peak expiratory flows (PEF) and both were superior to placebo in PEF and patient-reported secondary outcomes. Adverse events were similar across the three groups. ADB2R-B16-Arg/Arg genotype patients are known to represent 10–12 % of white and 20–25 % of African American asthmatic subjects and may be less responsive to LABAs (in the absence of ICS therapy) or may actually have worsening of symptoms with LABAs [62]. A recent review of tiotropium, recommended that symptomatic asthma patients already on high dose ICS and LABA therapy should be considered for the addition of LAMAs [53].
The risk of cardiovascular events including stroke, heart attack or death with the use of a SAMA or LAMA in COPD patients has been discussed and recently rejected regarding tiotropium [63], but this needs to be prospectively studied in asthma patients. Dry mouth, dry respiratory secretions, urinary retention, dilated pupils, blurred vision (if put into eyes), and increases in intraocular pressures in patients with glaucoma are major SAMA and LAMA side effects.
Corticosteroids
ICS are preferred initial controller drugs in persistent asthma, and systemic corticosteroids can be life-saving in acute severe asthma exacerbations in adults and children [2, 55]. The NAEPP Expert Panel 3 guidelines and separate reviews have focused on the importance of ICS therapy in treating persistent asthma patients [2, 64]. In adults and children, low-dose ICS therapy is preferred as early as step 2 and increases in ICS dose until step 6 is reached when oral corticosteroids may be added in an attempt to better control symptoms [2, 12]. Similarly, in the treatment of acute exacerbations of asthma in adults and children, the use of corticosteroids is a major therapeutic pillar [2, 55].
The mechanism of action of corticosteroids includes many cell- and tissue-specific anti-inflammatory effects. They bind to the glucocorticoid receptor (GR) that is localized primarily in the cytoplasm [65]. The interaction of the corticosteroid with the GR induces a conformational change that allows the activated GR to bind to DNA [66]. The binding occurs at the glucocorticoid responsive DNA sequence promoting the synthesis of anti-inflammatory proteins and inhibiting the transcription of many pro-inflammatory cytokines. Reductions in T lymphocytes, mast cells, eosinophils, and dendritic cells are seen with corticosteroid therapy [66]. Additional more complex and poorly understood effects are thought to be involved in explaining the entirety of the corticosteroid manifestations [65, 67, 68].
The currently available ICS products include dry powder, liquid for nebulization, or MDI delivery system (Table 1). Various strengths are available that makes it possible to establish low-, medium-, and high-dose ICS for maintenance therapy in increasingly severe persistent asthma.
In children and adults with persistent asthma, ICS therapy reduces wheezes, asthma exacerbations, and the risk of asthma-related hospitalization [69–73]. Clinical dose–response relationships in asthma have been variable with not all ICS demonstrating them in adults and children [74–76]. Significant response variability has been reported with ICS in persistent asthma patients that may account for some of the difficulty in demonstrating a strong ICS dose–response effect [77]. The PRICE Study demonstrated that short-term response to ICS predicts long-term asthma efficacy, but as high as 40 % of the patients were ICS nonresponders [78].
The recent “FENOtype” trial found a significant dose–response effect with ICSs for diurnal fractional exhaled nitric oxide (FENO) in a phenotype of asthma patients with high FENO [79]. Poorly controlled persistent asthma patients do not always respond to just doubling of their ICS dose [80]. High-dose ICS therapy has been shown to give better control than low-dose ICS therapy in asthma patients who were poorly controlled at the start of the study [81]. A systematic review confirmed that stopping low-dose ICS therapy in persistent but well-controlled asthma patients was associated with a statistically significant increase in the risk of asthma exacerbations [82].
Adding a LABA to low-dose ICS versus going to high-dose ICS in poorly controlled asthmatic patients has been systematically reviewed. The combination of a LABA and low-dose ICS was modestly more effective in reducing the risk of asthma exacerbations than the higher dose of ICS [83]. The LABA + low-dose ICS-treated group had higher rates of tremor and lower rates of oral candidiasis than did the high-dose ICS-treated group. Asthma patients controlled with low-dose ICS therapy then switched to a LABA or placebo were shown to have more treatment failures and asthma exacerbations than those left on low-dose ICS and both active treatment groups were superior to placebo [84]. A systematic review of asthmatic patients on ICS therapy who remained symptomatic and had either a LABA or an anti-leukotriene agent added was performed. The addition of the LABA to the ICS was superior to the addition of an anti-leukotriene therapy to the ICS in reducing oral corticosteroid treated exacerbations [85]. Steroid-naive adults and children with persistent stable asthma randomized to either an ICS + LABA were compared with those treated with just an ICS alone demonstrated improvement in lung function and asthma symptoms but no change in the rate of exacerbations requiring oral corticosteroids [43].
The recent STAMINA trial attempted to use mannitol provocation testing to predict the needed dose of ICS in patients with persistent asthma. The mannitol provocation test determined dose of ICS was then compared with a group that had their ICS dose based on its effect on PEF and FEV1 determinations [86]. Using the provocation approach, higher doses of ICS were given but no addition reduction in severe asthma exacerbations were found. FENO has been successfully used as a guide to decrease the dose of ICS in asthma patients [87]. The utility of FENO was confirmed by the recent “FENOtype” Trial that found that FENO could be used to direct dose and help control asthma in patients on ICSs [79].
Many of the CAS or refractory asthma patients fail to respond robustly to both inhaled and systemic corticosteroids [88]. Asthma patients that are smokers and patients that have persistent severe asthma often show reduced anti-inflammatory responsiveness to corticosteroids [89]. Corticosteroid resistance asthma may be due to one of several abnormalities including reduced glucocorticoid to GR binding, reduced GR expression, enhanced activation of inflammatory pathways, or lack of repressor function on these pathways [90]. A study examining 17 corticosteroid resistant asthma patients found that compared with corticosteroid sensitive asthmatics the vast majority displayed significant reduction in GR binding and the remaining had an abnormally low GR number with normal binding affinity [91].
Daily versus as-needed ICS therapy has been examined in mild-to-moderate asthma patients and found to be equal in their ability to reduce acute exacerbations [92, 93]. The daily ICS approach was found to be superior to intermittent ICS in many secondary outcomes such as spirometry and symptoms [94, 95].
A new extra-fine powder of beclomethasone + formoterol has been shown to have better distal airway delivery [96]. A pilot study compared it with fluticasone propionate + salmeterol in asthma patients and found it was associated with improved FEV1 during a 12-week treatment schedule [97]. The improved clinical outcome was thought to be because of its smaller particle size that allowed it to get deeper airway penetration [98]. Further clinical trials are needed in moderate-severe asthmatics to understand if there are real advantages to the extra fine particle ICS approach. No specific ICS agents when corrected for potency have been shown in systematic reviews to be more efficacious or to have less side effects, including one of the newest ICS ciclesonide, when compared with budesonide or fluticasone [99].
Self-reported ICS use is inaccurate with significant underuse of their maintenance medications being found [100]. Non-adherence is a serious problem in asthma and must be addressed in the difficult to control CAS patient before suggesting corticosteroid resistance [101, 102]. Poor adherence in difficult-to-control asthmatics can be improved with interventions and results in improved medication adherence but also improved clinical outcomes [103].
During acute asthma exacerbation, the use of oral corticosteroids is a well-established clinical practice [104]. Most studies have not found that doubling the maintenance dose of the ICS during outpatient acute asthma exacerbations changes the pattern of the exacerbation [80, 105]. A systematic review of increased versus stable doses of ICSs for exacerbations of chronic asthma in adults and children failed to show that an increase in ICS dose reduced the need for rescue oral corticosteroids [106]. This is contrasted to a systematic review of outpatient asthma exacerbations treated with a short-course of systemic corticosteroids (oral or intramuscular). The systemic corticosteroids reduced the number of relapses that required hospitalization and the number of doses of SABAs used without an apparent increase in side effects [107].
Patients presenting to an ED with acute asthma exacerbations are often treated with iv corticosteroids. A meta-analysis has suggested that patients initially treated with ICS therapy can reduce hospital admissions even when the ICS therapy is paired with systemic (oral, intramuscular, and iv) corticosteroids [108]. There is insufficient data to suggest ICS therapy alone can be used instead of systemic corticosteroids when treating acute asthma. A separate systematic review has concluded that the use of systemic corticosteroids within the first hour of ED presentation significantly reduces the need for hospitalization in acute asthma patients [109]. Systemic corticosteroids given to hospitalized children with acute asthma events produced improvements including earlier discharges and fewer relapses [110]. No difference in outcomes of hospitalized patients with acute severe asthma could be found between those patients receiving high- and low-dose systemic corticosteroids [111]. Several trials have specifically shown that oral and iv systemic corticosteroids produce similar clinical outcomes in acute asthma exacerbations that require hospitalizations [112–114].
Multiple studies of children and adults with acute asthma exacerbations treated and discharged from an ED or outpatient clinic have compared intramuscular corticosteroids (betamethasone, dexamethasone, methyl prednisolone, or triamcinolone) to short courses of oral prednisone or methylprednisolone [115–118]. All four trials found that the intramuscular dose was as effective as the short course of oral corticosteroids in reducing the relapse rate of acute asthma. An early randomized, double-blind trial of asthmatic patients with acute exacerbations discharged from the ED on tapering doses of oral corticosteroids evaluated the addition of ICS therapy [119]. After 21 days, those patients receiving ICS had statistically significant reductions in relapse rates and improved symptom scores compared with placebo inhalers. However, a recent meta-analysis evaluated the use of ICS therapy after ED discharge for acute asthma exacerbations and found insufficient evidence that it provided additional benefit when paired with systemic corticosteroids [120]. This same review found some, though nonconclusive, evidence that starting high-dose ICS therapy at the time of discharge from the ED improves outcomes.
The adverse effects and toxicities associated with corticosteroids are related to the dose, the potency, route, and total time of the exposure of the corticosteroid exposure. ICS are associated with candidiasis leading to cough, dysphonia, and oral thrush. Other effects include impaired growth in children, adrenal-axis suppression, decreased bone mineral density, skin thinning and bruising, glucose intolerance, and cataracts [121, 122]. Cortisol suppression has been shown to be dose-dependent when six ICSs were tested in 156 naive asthma subjects [123]. Ciclesonide, a “pro-drug” with unique pharmacokinetics and once-daily dosing, was hoped to reduce to systemic toxicities [121, 122] but this has not been confirmed [99].
Combination-Inhaled Preparations
Current combination-inhaled medications that are FDA-approved fall into two classes. The first class is that of bronchodilators (Table 1). A combination of albuterol and ipratropium is available as a SDM (Combivent Respirmat®) or as a solution for nebulizing (various generics or as Duoneb®). Although these are not FDA-approved for asthma, they are used in the treatment of acute exacerbations of asthma and allow for more rapid delivery of the two medications than sequential dosing.
The second class of combination-inhaled products includes a LABA plus an ICS (Table 1). There are currently four combinations of LABA + ICS available in the USA (budesonide + formoterol, fluticasone + salmeterol, fluticasone + vilanterol, and mometasone + formoterol). In addition, there is both a dry powder and a MDI version of the fluticasone + salmeterol combination available. The rest are either available as a dry powder or a MDI (Table 1). Many come in various corticosteroid doses and all are FDA-approved for asthma except the newest one, fluticasone + vilanterol, which is currently FDA-approved only for COPD.
In a recent review, little data was found to support better control with a combined LABA + ICS product compared with using separate LABA and ICS inhalers. The exception was a product mentioned before and not currently available in the USA, an extra fine beclomethasone + formoterol inhaler. A systematic review and a UK economic analysis evaluated various ICS and LABA combination products used in the treatment of asthma. They found that the ICS + LABA combination was potentially more clinically effective than doubling the dose of the ICS alone. The cost differences between the combined product therapy versus ICS monotherapy was variable depending on the doses required but there are potential cost savings using ICS + LABA combination products compared with an individual LABA inhaler used with an individual ICS inhaler [124]. This review also did not find either fluticasone + salmeterol or budesonide + formoterol inhalers to be consistently better than the other in the treatment of asthma.
A recent trial compared a defined dose of two actuations of a combined budesonide + formoterol MDI twice a day with the option to use one extra actuation as needed to the same maintenance dose of budesonide + formoterol MDI but with the option to use one or two albuterol actuations a day for asthma relief [125]. This 24-week trial in 303 asthmatic patients found that the as needed extra dose of the combination regimen resulted in higher ICS exposures, reduced oral corticosteroid exposures, and was associated with fewer severe asthma exacerbations. Patient convenience, better compliance, and potential expense savings make combination therapy with LABAs + ICS attractive in certain asthma patients.
Leukotriene Modulators
The NAEPP Expert Panel 3 guidelines [2] include leukotriene receptor (LTR) antagonists or the 5-lipoxygenase inhibitor zileuton as alternative therapies to ICSs for adults with persistent asthma in steps 2 through 4. The guidelines also suggest that for children ICSs are the preferred controller medication for children ages 0–4 years in step 2 and as potential add-on therapy from step 3 up to step 6. The LTR antagonist montelukast is identified as the alternative controller agent of choice for the 0- to 4-year-old asthmatic patients [12]. Although iv montelukast has been studied in acute asthma exacerbations with improvement in FEV1 documented [126], it has not been approved in the USA. Oral LTR antagonists are not included as treatment options for acute asthma exacerbations in the NAEPP Expert Panel 3 guidelines and reviews [2, 55, 126].
LTR antagonists (montelukast, pranlukast, and zafirlukast) block leukotriene D4 from interacting with cysteinyl leukotriene (CysLT1) receptors on airway smooth muscle [127]. The antagonism of the CysLT1 receptor on airway smooth muscle reduces bronchospasm and airway hyperresponsiveness. By inhibiting the enzyme 5-lipooxyenase, zileuton inhibits the formation of cytosol leukotriene A4 (LTA4). LTA4 is converted to leukotriene C4 (LTC4) and leukotriene B4 (LTB4) in the cytosol. Both LTB4 and LTC4 go through the cell wall transmembrane transporter into extracellular space where LTC4 is converted to LTD4 [127]. In a study of 25 children with mild-to-moderate persistent asthma, serum interleukin (IL)-10, an anti-inflammatory cytokine increased and eosinophil counts decreased with montelukast treatment. These changes correlated with lung function and clinical symptom improvements [128].
Montelukast provided clinically significant protection against cold, dry air-induced bronchospasm in 13 asthmatic children ages 3 to 5 independent of whether they were also on ICSs [129]. A large number of trials have investigated montelukast in comparison to ICS treatment in adult and pediatric asthma patients. Some have shown montelukast to be non-inferior to ICS treatment [130]. Other studies have reported similar improvement in air flow and rescue-free days in the 12-week double-blind portion of the study comparing montelukast to inhaled fluticasone, but during the 36 weeks follow-up of open-label period, the ICS group was associated with improved asthma control [131]. Most double-blind trials have reported the superiority of ICSs over montelukast in mild-to-moderate persistent childhood and adult asthma [132–134]. By contrast, using medical and drug records, montelukast-treated children with asthma had fewer hospital admissions and used less beta2 receptor agonist rescue inhaler doses per week than did those treated with ICSs [135]. It was postulated that this paradoxical finding might be related to shorter durations of prescriptions and lower patient adherence with ICSs than with montelukast. Significant variability in response exists with both ICS and montelukast therapy in children with asthma. Children with low pulmonary function or high levels of allergic inflammatory markers did better with ICS therapy [136]. In a study that compared eformoterol, fluticasone, and montelukast in adult asthmatics, peak expiratory flow rates were found to be greater in the morning with eformoterol and fluticasone than with montelukast but greater in the evening with montelukast the others [137]. When more “patient-centered” subjective endpoints were evaluated, fluticasone and eformoterol were better than montelukast in all three domains measured. A meta-analysis comparing inhaled fluticasone to oral montelukast in long-term control of pediatric asthma patients found montelukast to be effective in placebo controlled trials but to be inferior to ICSs [138].
Asthmatic cigarette smokers showed improvement with both montelukast and inhaled fluticasone therapy. The fluticasone treatments tended to show more benefit in patients with ≤11 pack years of smoking and those with >11 years tended to show more benefit with montelukast [139]. Asthmatic children with ADB2R-B16-Arg/Arg genotype were randomized to either add-on therapy with salmeterol or montelukast. The use of montelukast was associated with significant reductions in school absences and SABA use. Similarly, quality-of-life and symptom scores were better with montelukast than with salmeterol with no difference in FEV1 [140].
The data is similar with zafirlukast. When zafirlukast was evaluated in 50 moderate-severe asthmatic children between the ages of 12 and 16 years, 88 % showed clinical improvement and the medication was well tolerated over the 12 weeks of the study [141]. When zafirlukast or pranlukast was added to ICS, improved clinical outcomes compared with the ICS alone resulted [142, 143]. A series of studies have compared inhaled fluticasone to oral zafirlukast in adult and pediatric asthma patients. Inhaled fluticasone was associated with improved clinical and airflow outcomes compared with zafirlukast [144–147]. Using prescription event monitoring in England, zafirlukast was well tolerated in general practice settings [148].
A review of eight trials of LTR antagonists did not support their oral use in acute asthma exacerbations. Additional trials were thought to be needed to better understand whether iv LTR antagonists have a role in these patients [149].
Zileuton was added to usual care or the patients were kept on usual care in a study of 2,947 chronic asthmatics. Over the 12-months of the study, statistically significant reductions in hospitalizations need for emergency care and corticosteroid rescues occurred with increases in FEV1 were seen with zileuton compared with usual care [150]. An efficacy study of zileuton extended-release preparation compared it with montelukast in 210 adults patients suffering from chronic persistent asthma found zileuton to be significantly better than montelukast in improving air flow measures and asthma symptom scores [151]. Zileuton added to ICS was as effective as doubling the dose of ICS in patients with severe persistent asthma [152]. In stable moderate–severe asthma patients, the addition of zileuton to an ICS failed to change exhaled nitric oxide concentrations but increased FEV1 by a small but significant amount compared with baseline measures [153]. Single nucleotide polymorphisms (SNPs) in genes associated with CycLT1 receptor were studied in asthmatics. After adjusting for age and sex, six SNPs were found that appear to be linked to FEV1 response to zileuton, two of which are also known to be associated with the FEV1 response to montelukast [154]. Improvement in asthma control including improved FEV1 measures, decline in beta2 agonist use and a smaller proportion of patients reporting asthma exacerbations was seen with both immediate and extended-release zileuton compared with placebo [155].
Meta-analysis of 56 trials evaluating anti-leukotriene agents (zileuton and LTR antagonists) compared with ICSs in chronic asthmatic children and adults found the ICSs were superior to the anti-leukotriene agents [156]. Seventeen trials were used in a systematic review evaluating adding a LABA versus an anti-leukotriene to low-dose ICS therapy in chronic asthma patients. Although lung function and quality-of-life scores favoring the addition of a LABA were modest, LABAs were superior to anti-leukotriene agents in reducing oral corticosteroid-treated asthma exacerbations [85].
Limited adverse effects have been reported with montelukast except for rare cases of Churg–Strauss vasculitis. Reversible and rarely irreversible hepatitis has been reported with zafirlukast. Hepatic failure requiring liver transplant and resulting in death associated with zafirlukast-induced hepatitis has been reported. Cases of Churg–Strauss vasculitis have also been have also been reported with zafirlukast [2, 157]. Zileuton use has resulted in elevated liver enzymes in about 5 % of asthma patients with about 82 % occurring during the first 3 months of treatment [158, 159]. Resolution of the elevated liver enzymes occurred within 21 days after discontinuation of zileuton but 53 % of patients continued on the drug experienced resolution of the elevated liver enzymes.
Mast Cell Stabilizers
The first mast cell stabilizing agent used clinically is disodium cromoglycate also known as sodium cromolyn. This was followed by nedocromil but with the removal of all CFC propellants both MDI delivery systems for cromolyn and nedocromil were removed from market and not replaced (Table 3). Currently, only sodium cromolyn solutions for use in a nebulizer are available in the USA for the treatment of asthma (Tables 1 and 2).
The NAEPP Expert Panel 3 stepwise guidelines for the treatment of persistent severe asthma limit the use of sodium cromolyn to mild persistent asthma (step 2) in both adults and children as an alternative to ICS [2]. It is not useful in acute exacerbations of asthma and has little utility in adults or children with severe persistent asthma of the degree consistent with the CAS [64, 126, 160].
The mechanism of action of sodium cromolyn is not completely understood. It has been shown to inhibit IgE-stimulated mediator release from human mast cells in a dose–response fashion [161]. Both sodium cromolyn and sodium nedocromil are potent G-protein 35 (GPR35) agonists. GPR35 is found on human mast cells, basophils and eosinophils. It is up regulated with IgE challenge and the IgE effects are “dampened” by the presence of cromoglycates [161].
Evaluating the data for children ages 3 to 15 years with asthma in three HMOs from Seattle, Boston, and Chicago, the use of sodium cromolyn and ICS were both associated with large reductions in ED visits and hospitalizations [162]. A systematic review of 25 trials evaluated the effectiveness of ICS versus inhaled sodium cromolyn in adults and children with asthma. It concluded that the use of ICS was superior to inhaled sodium cromolyn in preserving lung function measures and in asthma symptom control [163]. A systematic review of 24 randomized, placebo-controlled trials in asthmatic patients found a small overall favorable treatment effect (lung function and symptoms) with sodium cromolyn over placebo despite apparent publication bias. Insufficient evidence was found for determining a beneficial effect as a maintenance treatment in children [164]. A more recent systematic review evaluated sodium cromolyn and failed to convincingly show evidence of its efficacy over placebo as maintenance therapy in childhood asthma [165]. Problems with dose and drug delivery have been suggested as possible explanations for the variability of results seen with sodium cromolyn in clinical trials and meta-analyses [166].
The potential adverse effects of inhaled sodium cromolyn are few but include cough, airway irritation, and acute bronchospasm. A single serious adverse reaction was reported in an asthmatic patient. The patient had previously demonstrated a positive skin test and inhalation provocation test to sodium cromolyn but used it during an acute asthma exacerbation resulting in a “near-death” exacerbation [167].
Methylxanthines and Phosphodiesterase 4 Inhibitors
The methylxanthines include theophylline and aminophylline. Aminophylline is a compound of theophylline and ethylenediamine in a 2:1 ratio. The ethylenediamine improves water solubility. The NAEPP Expert Panel 3 guidelines include oral theophylline as an alternative therapy to ICS for long-term control and prevention of only moderate to persistent asthma (steps 2–4) [2]. These guidelines do not include it for the treatment of children 4 years and younger [12]. A recent review of theophylline notes that it is now usually used as an “add-on” therapy in asthma patients not well controlled on ICS with or without LABAs [168]. Low-dose (blood levels in the 5–10 mg/L range) theophylline has also reduced peripheral blood monocytes, modulated T-lymphocyte activation in allergen-challenged asthmatics, improved clinical symptoms and modified bronchial biopsy associated T-lymphocytes counts [169–172]. Low-dose theophylline with a mean theophylline level of 6 mg/L reduced eosinophilic inflammation but not FENO in mild asthma [173]. Not nearly as popular as before, theophylline still remains a widely used medication in the worldwide treatment of asthma [4].
In acute exacerbations of severe asthma, the NAEPP Expert Panel 3 guidelines do not recommend the use of iv aminophylline [2]. A review of the emergency treatment of asthma in adults notes that methylxanthines were once “standard treatment” but now are not recommended for acute exacerbations of asthma in the ED because of the lack of data to support benefit and significant potential complication with their use [55, 126].
The bronchodilator effect of theophylline is thought to be through inhibition of phosphodiesterase (PDE)3 and the anti-inflammatory effect is from its inhibition or PDE4 and histone deacetylase-2 activation that turns off activated inflammatory genes and can reverse corticosteroid resistance seen in some patients with severe asthma [168, 174]. The methylxanthines may also improve diaphragm contractility and mucociliary clearance [2].
Suppression of pro-inflammatory mediators such as eosinophil cationic protein, histamine, serotonin, thromboxane B2, and leukotriene C4 was found with aminophyliine infusions compared with SABA inhalation in acute asthma patients [175]. In a randomized, double blind, placebo controlled trial of 163 children (aged 1–19) who presented with acute asthma exacerbation and were unresponsive to three nebulized SABA treatment, those treated with aminophylline had greater spirometric improvement at six hours and fewer patients required intubation and mechanical ventilation [176]. Another trial of children between 2 and 5 years of age randomized to aminophylline or normal saline with acute asthma in an ED failed to show any change in the number of required SABA treatments, duration of oxygen treatment and length of hospital stay [177]. A trial of theophylline versus terbutaline in treating critically ill children in status asthmaticus found that adding theophylline to continuous albuterol nebulization and iv corticosteroids was as effective as adding terbutaline and more cost-effective [178]. An early meta-analysis evaluating 13 trials of aminophylline treatment in severe acute asthma failed to show a difference between the aminophylline-treated group and the control groups despite widespread use of it at the time in treating acute asthma [179]. A more recent systematic review of 15 trials found no statistically significant effect of aminophylline on airflow outcomes compared with standard use of inhaled SABA therapy in the treatment of acute asthma exacerbation but those getting aminophylline reported significant increases in palpitations and arrhythmias but not tremor or hospital admissions [180].
A study of 747 patients with asthma over a year randomized to twice daily theophylline or inhaled beclomethasone dipropriate confirmed the effectiveness of theophylline at lower than customarily recommended blood levels in controlling asthma symptoms. Inhaled beclomethasone also improved all the clinical and symptom measures at a small but statistically better degree than did theophylline [181]. Theophylline was associated with more headaches, nervousness, insomnia, and gastrointestinal distress than did inhale beclomethasone. Inhaled beclomethasone was associated with more oropharyngeal candidiases, hoarseness, reduced morning cortisol levels, and rate of growth in children than did theophylline. More patients discontinued theophylline than did beclomethasone [181].
Several studies have demonstrated clinical symptoms and lung function improvement with oral theophylline [182–184]. When moderate asthma patients on low-dose inhaled budesonide were randomized to theophylline or high-dose inhaled budesonide, both approaches produced similar benefits. These effects were achieved with theophylline concentrations lower than the recommended therapeutic range of 10–20 mg/L [185]. Several other clinical trials have shown less impressive findings. Inhaled budesonide was better than oral theophylline in improving lung function [186]. Low-dose theophylline failed to demonstrate immunomodulatory effects and improve clinical symptoms in moderate childhood asthma [187]. Inhaled beclomethasone was favored over oral theophylline in moderate asthma during pregnancy [188]. Adding salmeterol was more effective than adding theophylline in moderate asthma patients on ICS [189]. Adding a LABA was more efficacious in asthma patients with nocturnal exacerbations uncontrolled on ICS than adding theophylline [190]. When once a day LTR antagonist was compared with once a day theophylline or once a day theophylline in patients with mild persistent asthma, the budesonide-treated group resulted in significantly greater improvement in lung function and no exacerbations over the 3-month study period [191]. In a systematic review of methylxanthines as maintenance treatment for asthma in children, methylxanthine treatment was shown to be better than placebo in symptom free days, the use of rescue medication and in FEV1 determinations [192]. When methylxanthines were compared with ICS, asthma exacerbations were less frequent with ICS therapy than with methylxanthines but no significant difference in lung function was noted. More headaches and nausea was reported with the use of methylxanthines. In studies that compared the use of methylxanthines with the use of inhaled SABAs, fewer hospitalization, better lung function, and fewer headaches were seen with SABA use while fewer complaints about tremor were seen with the use of methylxantines [192].
No reports were found on the role of theophylline in the outpatient care of CAS patients.
The potential role of theophylline in chronic therapy of asthma is limited in part because of the lack of consistent data on its benefits but also because of its adverse effects including headaches, nausea, vomiting, gastrointestinal distress, cardiac arrhythmias, and seizures [168].
A specific PDE4 inhibitor, roflumilast, has been approved worldwide for the treatment of COPD. Its use in COPD patients results in small improvement in FEV1 but more importantly roflumilast reduces COPD exacerbations in those patients with significant airflow obstruction and frequent exacerbations [193–195]. Oral PDE4 inhibitors including cilomilast and roflumilast have been evaluated in asthma since the early 1990s with variable results. Current asthma guidelines do not include roflumilast. They are not indicated in acute exacerbations of COPD and are unlikely to be used in acute asthma. Roflumilast has been suggested as a possible treatment in patients with difficult-to-control asthma consistent with the CAS patient [64].
There are 11 known PDE isoenzymes with roflumilast selectively inhibiting PDE4. Roflumilast and its dichloropyridyl N-oxide metabolite both have similar PDE4 inhibitor potency [195]. The inhibition of the PDE4 results in increased intracellular cyclic AMP levels and this is thought to contribute to its mechanism of action. Additional effects of roflumilast include anti-inflammatory, anti-remodeling, and anti-fibrotic properties. Modulation of neutrophils, monocytes, marcophages, CD4+ and CD8+ T cells, endothelial cells, fibroblasts, smooth muscle cells, and epithelial cells are thought to be the beneficial effects of roflumilast [195].
In a small (n = 23) randomized, double-blind, placebo-controlled, crossover study of 7–10 days each, mild asthmatics showed attenuation of allergen-induced FEV1 reductions with either 250 or 500 μg/day of roflumilast. The effects were greatest on the late phase asthmatic reactions but the drug also significantly attenuated early phase response compared with placebo [196]. A single dose of 1,000 μg of roflumilast was shown to attenuate allergen-induced airway hyperresponsiveness again during primarily the late phase reaction compared with placebo [197]. A double-blind, placebo-controlled, crossover study (each phase of 14 days) evaluated 500 μg of roflumilast versus placebo in 25 subjects with mild asthma against allergen-induced late phase response using FEV1 and sputum analysis. A protective effect in allergen-induced late phase decrease in FEV1 and an impressive reduction in sputum airway inflammatory cells was seen with roflumilast compared with placebo [198]. Roflumilast has also been shown to be effective in exercise-induced asthma and to suppress lipopolysaccharide-induced tumor necrosis factor alpha release in patients [199]. Two moderately sized clinical trials in asthmatic patients have been performed. In a double-blind, double-dummy, randomized noninferiority study of 499 patients with persistent asthma, roflumilast and inhaled beclomethasone dipropriate both significantly improved FEV1, FVC, and median asthma symptom scores and reduced rescue medication use over 12 weeks [200]. A 12-week randomized, double-blind, parallel-group study in 693 asthmatic patients compared 3 different doses of roflumilast. FEV1 improvement compared with baseline was seen in all three roflumilast doses with the change being the largest (400 mL) in the 500 mcg/day dose [201]. Despite these promising early clinical studies, indications for asthma use were not pursued to approval.
Side effects of roflumilast include nausea, diarrhea and headaches. The diarrhea can be mild to moderate severity, is usually self-limited but it can limit the use of the medication [193, 194]. The weight loss (up to 10 % of body weight) reported in COPD patients have not been reported to date in these small trials.
Immunotherapy and Immunomodulators
The adjunctive use of allergen-specific immunotherapy (SIT) is considered in steps 2–4 but not in steps 5–6 in patients with persistent asthma in the NAEPP Expert Panel 3 guidelines [2]. SIT is recommended for house-mites, animal dander, and pollen. The evidence is thought to be strongest for single allergens and weakest for molds and cockroaches in asthma [2]. Allergen therapy is associated with increases in allergen-specific IgA and IgG antibodies and with reductions in the level of allergen-specific IgE antibodies [202]. The resulting immunological tolerance may generate blocking IgG antibodies after repeated exposure to the allergen. Other SIT mechanisms postulated include T regulatory cell induction that produces ILs that suppress mast cells, eosinophils and other T cell [202].
The most recent meta-analysis of 88 trials evaluating subcutaneous SIT in asthma demonstrated significant improvement in asthma symptom scores, reduction in needed asthma medications, improvement in bronchial hyper-reactivity, and reductions in the rate of symptom deterioration [203]. A recently published systematic review of sublingual immunotherapy (SLIT) found moderate grade level of evidence to support effectiveness in the treatment of asthma [204]. Improvement in asthma symptoms and a reduction in asthma medication requirements were found with SLIT. Little information exists on the use of subcutaneous SIT or SLIT in patients with more severe asthma including CAS patients. Avoidance of SIT during severe acute exacerbations of asthma is common. Adverse effects of immunotherapy include local skin reactions to allergens, upper and lower respiratory reactions, worsening of asthma symptoms, and systemic reactions rarely including anaphylaxis [204].
In patients with poorly controlled IgE-medicated asthma, omalizumab is an approved humanized IgG that inhibits the binding of IgE to the high-affinity IgE receptor on the surface of mast cells and basophils [202]. In the NAEPP Expert Panel 3 guidelines [2], omalizumab is considered in IgE-mediated asthma in children greater than or equal to 12 years and in adults at steps 5 or 6. Subcutaneous dosing of omalizumab is based on weight and the initial IgE levels and must be given in a health-care facility because of the small risk of anaphylaxis. It is dosed every 2 to 4 weeks and is currently very expensive therapy.
Clinical trials have shown fewer asthma exacerbations and reduced corticosteroids requirements with omalizumab treatment in severe allergic asthma patients 12 to 75 years of age [205–208]. A systematic review of 14 trials also found that treatment with omalizumab significantly reduced free levels of IgE in patients with allergic asthma and high initial levels of IgE [209]. This review also confirmed the reduction with omalizumab treatment in both asthma exacerbations and ICS needs. Looking at patients treated with omalizumab between the ages of 6–11 years with IgE-mediated severe persistent asthma, the National Institute for Health and Clinical Excellence (NICE) of the UK initially found a statistically significant reduction of asthma exacerbation at 52 weeks using sponsors existing data but did not recommend its continued use in this age group because of poor cost-effectiveness [210, 211]. The NICE group recommended omalizumab as a “possible” treatment for adults and young people over the age of 12 with severe persistent allergic asthma poorly controlled on standard therapy [212]. Recently, NICE published guidance has changed and now is recommending omalizumab as an approved add-on option for severe, persistent, IgE-mediated asthma for patients aged 6 and older if the manufacturer provides a “confidential discount” [213]. Current US FDA indications still limit its indication to patients ≥ age 12 with IgE mediated severe persistent asthma. Many CAS patients with IgE-mediated asthma should be considered for a trial of 4–6 months of omalizumab to assess its effectiveness in preventing acute exacerbations.
Adverse events with omalizumab include anaphylaxis, injection site reactions, urticaria, and small possible small increased risk (estimated at 0.5 %) for malignancies [214], which has not been confirmed in long-term safety studies [215].
Magnesium Sulfate
The NAEPP Expert Panel 3 guidelines [2] endorse the use of iv magnesium sulfate in the treatment of acute asthma exacerbations and are silent on its use orally in poorly controlled persistent asthma. Some reviews and guidelines on the treatment of acute asthma exacerbations in children and adults do not address the use of magnesium [12, 55, 216], while others support its use [4, 126]. There are a number of possible mechanism postulated to explain the bronchial smooth muscle relation seen with magnesium including inhibiting calcium influx into the cytosol by blocking its entry and its release from the endoplasmic reticulum and activating sodium–calcium pumps [217, 218]. Magnesium also inhibits the interaction between calcium and myosin leading to muscle cell relaxation. It also can stabilize T-cells and inhibits mast cell degranulation, histamine release, and inflammatory mediators. It may inhibit acetylcholine release from cholinergic nerves, increase beta2 agonist receptor affinity, and stimulate nitric oxide and prostacyclin synthesis leading to bronchodilation.
The evaluation of chronic magnesium supplementation in asthma patients has been variable with some investigators reporting no clinical improvement with it [219], while others showing improved symptom control, reduced bronchial reactivity to methacholine, and decreased allergen-induced skin responses in children and adults [220, 221]. A review of magnesium therapy concluded that further research is needed to define any responsive sub-populations and to confirm any overall efficacy of oral magnesium in adult and pediatric persistent asthma patients [216].
The utility of iv magnesium sulfate for acute exacerbations of asthma treated in the ED in adults and children has been confirmed by several systematic reviews and meta-analyses [217, 218, 222]. When combined with SABAs and systemic corticosteroids, iv magnesium improved pulmonary function and reduced hospitalization in children and improved pulmonary function in adults [218]. A recent randomized-controlled trial in children with acute severe asthma exacerbations confirmed that iv magnesium sulfate given with the first hour in the ED significantly reduced the percentage of children who required mechanical ventilation [223].
The use of nebulized magnesium sulfate has been reviewed and felt to be better than placebo as an acute bronchodilator in acute asthma exacerbations [216]. An early systematic review suggested that nebulized magnesium sulfate when added to a SABA improved pulmonary function and reduced hospital admissions [224]. In a more recent meta-analysis, weak evidence of improvement in pulmonary function and hospital admission rates with nebulized magnesium was seen in adults but not in children [222]. A Cochrane Systematic Review concluded that there is no good evidence that magnesium can be used as a substitute for inhaled SABAs or adds anything to SABAs when combined in acute asthma exacerbations [225]. This is in contrast to a recent meta-analysis which found nebulized magnesium with beta2 agonists compared with nebulized beta2 agonist alone was associated with greater improved pulmonary function and reduced hospital admissions in adult patients with asthma exacerbations [218]. Further study has been suggested with both inhaled magnesium and current the recommended bronchodilators (SABAs + SAMAs) to better understand if there is a role for nebulized magnesium in the treatment of acute asthma exacerbation [225, 226].
As magnesium is primarily an intracellular ion, monitoring serum levels do not reflect adequately intracellular concentrations or total body stores [217]. Lower intracellular magnesium concentrations have been found during asthma exacerbations [227]. Adverse effects from acute magnesium are rare. Minor side effects include flushing, iv site pain and fatigue [216]. Abnormal renal function may put the patient at increased risk for more serious magnesium side effects including hypotension, hyporeflexia, arrhythmia, and respiratory depression.
Heliox
Heliox, a combination of helium and oxygen gas has been evaluated in asthma since the 1930s [228]. Its low density and viscosity gives helium favorable characteristics in laminar and turbulent flow situations that are seen in asthma patients. The NAEPP Expert Panel 3 [2] has recommended that heliox-driven albuterol nebulization be considered for life-threatening exacerbations of asthma in patients remaining critical after 1 h of intensive conventional therapy. A review of the emergency treatment of asthma concluded the role of Heliox in the management of acute asthma is still “unclear” [55].
Technical aspects of using heliox in clinical settings has improved with regulators, flow meters and devices now available that are designed and calculated for the commonly available helium and oxygen mixed concentrations (80:20 and 70:30) [229]. Several devices are now FDA approved for use with heliox. Heliox can also be used to drive bronchodilator nebulization devices [230].
Using Heliox to drive bronchodilator nebulization is associated with deeper lung delivery of the agent [230]. Several studies in adults have shown improved FEV1 using heliox-driven bronchodilator nebulization compared with using pure oxygen-driven systems [231, 232]. However, a study in children (ages 2–21 years) failed to demonstrate shorter hospitalizations in moderate-to-severe asthma exacerbations with the use of heliox-powered albuterol nebulization compared with oxygen-driven albuterol nebulization [233]. A systematic review published in 2007 evaluated the use of heliox-driven nebulizers and found improved air-flow measures in patients compared with those getting oxygen-driven nebulizers but failed to show improved rates of recovery [234].
Using heliox (60:40 or 70:30 concentrations) alone in adult patients presenting with acute exacerbations of asthma rapidly improved both arterial blood gas carbon dioxide and pH determinations [235]. A randomized controlled trial of using heliox (70:30 concentration) or 30 % oxygen in the ED in patients with acute severe asthma resulted in both statistically improved peak expiratory flow rates and symptoms [236]. A systematic review concluded that heliox during the first hour of acute asthma treatment offered mild-to-moderate benefits using surrogate markers including peak expiratory flow rates and dyspnea [237]. A 2006 systematic review of seven trials of adults and children confirmed an improvement in pulmonary function in the subgroup of patients with the most severe asthma exacerbations but failed to show improvement overall [238].
It has been pointed out that the greatest risk of heliox therapy is its use in a “jury-rigged device” by an incompletely trained provider [229]. Monitory equipment and devices not approved for heliox run the risk of providing low oxygen concentrations, generating excessive tidal volumes on a ventilator and delivering to little or much bronchodilators. Hypothermia has been associated with hood delivery systems in infants and is a potential issue with adults using facemasks.
Emerging Agents
Future advances in the treatment of CAS patients appear near and are likely to be the result of a better understanding of the immunobiology and pathophysiology of asthma and the improved ability to define the genotype and phenotype of individual asthma patients [239, 240]. The heterogeneity of patient response to current asthma medications suggests that a better understanding of the individual genetic polymorphisms will allow the utilization of “personalized medicine” for asthma patients in the future [241].
The use and relative success of the biological agent omalizumab has generated wide interest in potential biologics for the treatment of asthma [242]. A number of agents are in development or in actual clinical trials. Most are IgG antibodies to IL-5, IL-13, IL-4, IL-9, IL-17, and tumor necrosis factor alpha (TNF) but others are agents that inhibit IL-4, IL-13, IL-9, or granulocyte-macrophage colony-stimulating factor and soluble TNF [242]).
IL-13 is a key type 2 helper T cell (TH2) cytokine that modulates many parts of airway inflammation and remodeling triggered in allergic asthma [243]. A recent double-blind, randomized, placebo-controlled 24-week trial of lebrikizumab, an anti-IL-13 humanized IgG antibody was performed with 219 adult asthmatics with inadequately controlled symptoms despite corticosteroids. Periostin was used as a surrogate biomarker for IL-13 levels. Patients were stratified based on high or low baseline periostin levels. Clinically, small but statistically significant increases in FEV1 were found with the lebrikizumab treatment. The high baseline periostin subgroup showed the greatest improvement [244]. No significant changes were seen in asthma exacerbation rates.
Another study evaluated dupilumab, a monoclonal IgG antibody to the IL-4 receptor in patients with persistent moderate-to-severe asthma patients. The IL-4 receptor that dupilumab is directed against inhibits both IL-4 and IL-13 signaling of the TH2 pathway. This pathway is activated in more than 50 % of asthmatics [245]. The randomized, double-blind, placebo-controlled parallel group trial included 104 asthma patients. Marked reductions were seen in asthma exacerbations in the dupilumab treated group with improved lung function, symptoms, and TH2 inflammatory biomarkers [246].
Two trials have evaluated mepolizumab, a monoclonal antibody against IL-5 in severe persistent asthma patients. Both studies showed significant reductions in rates of asthma exacerbations over the year of treatment [247, 248]. Other preliminary clinical trials have shown potential in controlling asthma symptoms with the Toll-like receptor 9 agonist packaged into virus-like particles called QbG10. The agent suppresses TH2 responses [249]. Anti-TNF therapies in asthma have resulted in mixed outcomes leading one author to conclude that the risk of anti-TNF therapies outweighs any potential benefit in severe asthma while others argue a subgroup of severe asthma patient may still benefit [250, 251].
Several other drugs have recently been investigated in persistent asthma or acute asthma exacerbations with limited clinical efficacy shown. Neither azithromycin nor statin therapy have to date been shown to improve chronic asthma [252, 253]. Oral ketamine for acute asthma exacerbations was evaluated in a systematic review with only one randomized study found and it failed to find significant benefit in non-intubated children with acute severe asthma exacerbations [254]. A trial of adults with acute severe asthma exacerbations failed to show any advantage when recombinant human DNAase was nebulized and given in addition to standard bronchodilator [255].
As the currently available ICS and combination inhalers are in general very effective, relatively inexpensive and reasonably safe in controlling the vast majority of asthma patients, new drug development in asthma of expensive biologics may face a real financial challenge in the future [240].
Conclusions
Current guidelines for the treatment of the CAS patient offer a good starting point for chronic and the acute asthma management. However, many CAS patients remain poorly controlled and need special attention to their pharmacotherapy which should be aimed to effectively prevent the next exacerbation. Approaches that address genotype and phenotype are needed to maximize personalized therapy to reduce impairment and risk from persistent asthma. Corticosteroids remains a main pillar in the controller treatment of these patients but expertise in adding on alternative treatments, inflammatory modulators and biological agents will likely improve outcomes and help to prevent acute severe exacerbations. Early use of systemic corticosteroids and aggressive bronchodilator therapy is lifesaving in severe acute asthma exacerbations and CAS.
References
Bateman ED, Hurd SS, Barnes PJ et al (2008) Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J 31:143–178
National Asthma Education and Prevention Program (2007) National Heart, Lung and Blood Institute. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Available from http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.pdf
Lin TY, Poon AH, Hamid Q (2013) Asthma phenotypes and endotypes. Curr Opin Pulm Med 19:18–23
Murata A, Ling PM (2012) Asthma diagnosis and management. Emerg Med Clin North Am 30:203–222, vii
Agache I, Akdis C, Jutel M, Virchow JC (2012) Untangling asthma phenotypes and endotypes. Allergy 67:835–846
Louie S, Zeki AA, Schivo M et al (2013) The asthma-chronic obstructive pulmonary disease overlap syndrome: pharmacotherapeutic considerations. Expert Rev Clin Pharmacol 6:197–219
Miravitlles M, Soriano JB, Ancochea J et al (2013) Characterisation of the overlap COPD-asthma phenotype. Focus on physical activity and health status. Respir Med 107:1053–1060
de Marco R, Pesce G, Marcon A et al (2013) The coexistence of asthma and chronic obstructive pulmonary disease (COPD): prevalence and risk factors in young, middle-aged and elderly people from the general population. PLoS One 8:e62985
McDonald VM, Higgins I, Gibson PG (2013) Insight into older peoples’ healthcare experiences with managing COPD, asthma, and asthma-COPD overlap. J Asthma 50:497–504
Zeki AA, Schivo M, Chan A, Albertson TE, Louie S (2011) The asthma-COPD overlap syndrome: a common clinical problem in the elderly. J Allergy (Cairo) 2011:861926
Lougheed MD, Lemiere C, Dell SD et al (2010) Canadian Thoracic Society Asthma Management Continuum—2010 Consensus Summary for children six years of age and over, and adults. Can Respir J 17:15–24
Bacharier LB, Guilbert TW (2012) Diagnosis and management of early asthma in preschool-aged children. J Allergy Clin Immunol 130:287–296, quiz 297–288
Cazzola M, Page CP, Rogliani P, Matera MG (2013) Beta2-agonist therapy in lung disease. Am J Respir Crit Care Med 187:690–696
Dhuper S, Chandra A, Ahmed A et al (2011) Efficacy and cost comparisons of bronchodilatator administration between metered dose inhalers with disposable spacers and nebulizers for acute asthma treatment. J Emerg Med 40:247–255
Cates, C.J., Crilly, J.A. and Rowe, B.H. (2006) Holding chambers (spacers) versus nebulisers for beta-agonist treatment of acute asthma. Cochrane Database Syst Rev. CD000052
Rodrigo GJ, Rodrigo C (2002) Continuous vs intermittent beta-agonists in the treatment of acute adult asthma: a systematic review with meta-analysis. Chest 122:160–165
Camargo, C.A., Jr., Spooner, C.H. and Rowe, B.H. (2003) Continuous versus intermittent beta-agonists in the treatment of acute asthma. Cochrane Database Syst Rev. CD001115
Walters, E.H. and Walters, J. (2000) Inhaled short acting beta2-agonist use in asthma: regular vs as needed treatment. Cochrane Database Syst Rev. CD001285
Travers AH, Rowe BH, Barker S, Jones A, Camargo CA Jr (2002) The effectiveness of IV beta-agonists in treating patients with acute asthma in the emergency department: a meta-analysis. Chest 122:1200–1207
Travers AH, Milan SJ, Jones AP, Camargo CA Jr, Rowe BH (2012) Addition of intravenous beta(2)-agonists to inhaled beta(2)-agonists for acute asthma. Cochrane Database Syst Rev 12:CD010179
Travers AH, Jones AP, Camargo CA Jr, Milan SJ, Rowe BH (2012) Intravenous beta(2)-agonists versus intravenous aminophylline for acute asthma. Cochrane Database Syst Rev 12:CD010256
Cochrane GM, Clark TJ, Hanan ME (1973) The role of oral bronchodilator therapy as shown by a comparison between salbutamol and terbutaline. Curr Med Res Opin 1:517–523
Harris L (1973) Comparison of cardiorespiratory effects of terbutaline and salbutamol aerosols in patients with reversible airways obstruction. Thorax 28:592–595
Adoun M, Frat JP, Dore P, Rouffineau J, Godet C, Robert R (2004) Comparison of nebulized epinephrine and terbutaline in patients with acute severe asthma: a controlled trial. J Crit Care 19:99–102
Abroug F, Nouira S, Bchir A, Boujdaria R, Elatrous S, Bouchoucha S (1995) A controlled trial of nebulized salbutamol and adrenaline in acute severe asthma. Intensive Care Med 21:18–23
Spiteri MA, Millar AB, Pavia D, Clarke SW (1988) Subcutaneous adrenaline versus terbutaline in the treatment of acute severe asthma. Thorax 43:19–23
Ayres J, Fish DR, Wheeler DC, Wiggins J, Cochrane GM, Skinner C (1984) Subcutaneous terbutaline and control of brittle asthma or appreciable morning dipping. Br Med J (Clin Res Ed) 288:1715–1716
Payne DN, Balfour-Lynn IM, Biggart EA, Bush A, Rosenthal M (2002) Subcutaneous terbutaline in children with chronic severe asthma. Pediatr Pulmonol 33:356–361
Donohue JF (2004) Therapeutic responses in asthma and COPD. Bronchodilators. Chest 126:125S–137S, discussion 159S–161S
Nishiyama O, Taniguchi H, Kondoh Y et al (2006) Comparison of the effects of tulobuterol patch and salmeterol in moderate to severe asthma. Clin Exp Pharmacol Physiol 33:1016–1021
Mochizuki H, Nanjo Y, Takahashi H (2013) Better adherence to a transdermal tulobuterol patch than inhaled salmeterol in elderly chronic obstructive pulmonary disease patients. Geriatr Gerontol Int 13:398–404
Katsunuma T, Ohya Y, Fujisawa T et al (2012) Effects of the tulobuterol patch on the treatment of acute asthma exacerbations in young children. Allergy Asthma Proc 33:e28–e34
Israel E, Chinchilli VM, Ford JG et al (2004) Use of regularly scheduled albuterol treatment in asthma: genotype-stratified, randomised, placebo-controlled cross-over trial. Lancet 364:1505–1512
Israel E, Drazen JM, Liggett SB et al (2001) Effect of polymorphism of the beta(2)-adrenergic receptor on response to regular use of albuterol in asthma. Int Arch Allergy Immunol 124:183–186
Tattersfield AE, Hall IP (2004) Are beta2-adrenoceptor polymorphisms important in asthma–an unravelling story. Lancet 364:1464–1466
Johnson M (2006) Molecular mechanisms of beta(2)-adrenergic receptor function, response, and regulation. J Allergy Clin Immunol 117:18–24, quiz 25
Dodda VR, Spiro P (2012) Can albuterol be blamed for lactic acidosis? Respir Care 57:2115–2118
Sykes DA, Charlton SJ (2012) Slow receptor dissociation is not a key factor in the duration of action of inhaled long-acting beta2-adrenoceptor agonists. Br J Pharmacol 165:2672–2683
Patel S, Summerhill S, Stanley M, Perros-Huguet C, Trevethick MA (2011) The reassertion profiles of long acting beta2-adrenoceptor agonists in the guinea pig isolated trachea and human recombinant beta2-adrenoceptor. Pulm Pharmacol Ther 24:247–255
Cheung D, Timmers MC, Zwinderman AH, Bel EH, Dijkman JH, Sterk PJ (1992) Long-term effects of a long-acting beta 2-adrenoceptor agonist, salmeterol, on airway hyperresponsiveness in patients with mild asthma. N Engl J Med 327:1198–1203
Greenstone, I.R., Ni Chroinin, M.N., Masse, V., et al. (2005) Combination of inhaled long-acting beta2-agonists and inhaled steroids versus higher dose of inhaled steroids in children and adults with persistent asthma. Cochrane Database Syst Rev. CD005533
Castro-Rodriguez JA, Rodrigo GJ (2012) A systematic review of long-acting beta2-agonists versus higher doses of inhaled corticosteroids in asthma. Pediatrics 130:e650–e657
Ni Chroinin, M., Greenstone, I., Lasserson, T.J. and Ducharme, F.M. (2009) Addition of inhaled long-acting beta2-agonists to inhaled steroids as first line therapy for persistent asthma in steroid-naive adults and children. Cochrane Database Syst Rev. CD005307
Suissa S, Ariel A (2013) US Food and Drug Administration-mandated trials of long-acting beta-agonists safety in asthma: will we know the answer? Chest 143:1208–1213
Castle W, Fuller R, Hall J, Palmer J (1993) Serevent nationwide surveillance study: comparison of salmeterol with salbutamol in asthmatic patients who require regular bronchodilator treatment. BMJ 306:1034–1037
Spitzer WO, Suissa S, Ernst P et al (1992) The use of beta-agonists and the risk of death and near death from asthma. N Engl J Med 326:501–506
Nelson HS, Weiss ST, Bleecker ER, Yancey SW, Dorinsky PM, Group, S.S (2006) The Salmeterol Multicenter Asthma Research Trial: a comparison of usual pharmacotherapy for asthma or usual pharmacotherapy plus salmeterol. Chest 129:15–26
Salpeter SR, Buckley NS, Ormiston TM, Salpeter EE (2006) Meta-analysis: effect of long-acting beta-agonists on severe asthma exacerbations and asthma-related deaths. Ann Intern Med 144:904–912
Cates CJ, Oleszczuk M, Stovold E, Wieland LS (2012) Safety of regular formoterol or salmeterol in children with asthma: an overview of Cochrane reviews. Cochrane Database Syst Rev 10:CD010005
Weatherall M, Wijesinghe M, Perrin K, Harwood M, Beasley R (2010) Meta-analysis of the risk of mortality with salmeterol and the effect of concomitant inhaled corticosteroid therapy. Thorax 65:39–43
Kramer JM (2009) Balancing the benefits and risks of inhaled long-acting beta-agonists—the influence of values. N Engl J Med 360:1592–1595
Salpeter SR, Ormiston TM, Salpeter EE (2004) Cardiovascular effects of beta-agonists in patients with asthma and COPD: a meta-analysis. Chest 125:2309–2321
Bollmeier SG, Lee SY (2013) The emerging role of tiotropium for patients with asthma. Ann Pharmacother 47:704–713
Gelb AF, Karpel J, Wise RA, Cassino C, Johnson P, Conoscenti CS (2008) Bronchodilator efficacy of the fixed combination of ipratropium and albuterol compared to albuterol alone in moderate-to-severe persistent asthma. Pulm Pharmacol Ther 21:630–636
Lazarus SC (2010) Clinical practice. Emergency treatment of asthma. N Engl J Med 363:755–764
Teoh L, Cates CJ, Hurwitz M, Acworth JP, van Asperen P, Chang AB (2012) Anticholinergic therapy for acute asthma in children. Cochrane Database Syst Rev 4:CD003797
Plotnick, L.H. and Ducharme, F.M. (2000), Combined inhaled anticholinergics and beta2-agonists for initial treatment of acute asthma in children. Cochrane Database Syst Rev. CD000060
Rodrigo GJ, Castro-Rodriguez JA (2005) Anticholinergics in the treatment of children and adults with acute asthma: a systematic review with meta-analysis. Thorax 60:740–746
Rodrigo GJ, Rodrigo C (2000) First-line therapy for adult patients with acute asthma receiving a multiple-dose protocol of ipratropium bromide plus albuterol in the emergency department. Am J Respir Crit Care Med 161:1862–1868
Kerstjens HA, Engel M, Dahl R et al (2012) Tiotropium in asthma poorly controlled with standard combination therapy. N Engl J Med 367:1198–1207
Peters SP, Kunselman SJ, Icitovic N et al (2010) Tiotropium bromide step-up therapy for adults with uncontrolled asthma. N Engl J Med 363:1715–1726
Bateman ED, Kornmann O, Schmidt P, Pivovarova A, Engel M, Fabbri LM (2011) Tiotropium is noninferior to salmeterol in maintaining improved lung function in B16-Arg/Arg patients with asthma. J Allergy Clin Immunol 128:315–322
Michele TM, Pinheiro S, Iyasu S (2010) The safety of tiotropium—the FDA’s conclusions. N Engl J Med 363:1097–1099
Mathew J, Aronow WS, Chandy D (2012) Therapeutic options for severe asthma. Arch Med Sci 8:589–597
Chung KF, Caramori G, Adcock IM (2009) Inhaled corticosteroids as combination therapy with beta-adrenergic agonists in airways disease: present and future. Eur J Clin Pharmacol 65:853–871
Raissy HH, Kelly HW, Harkins M, Szefler SJ (2013) Inhaled corticosteroids in lung diseases. Am J Respir Crit Care Med 187:798–803
Yick CY, Zwinderman AH, Kunst PW et al (2013) Glucocorticoid-induced changes in gene expression of airway smooth muscle in patients with asthma. Am J Respir Crit Care Med 187:1076–1084
Newton R (2000) Molecular mechanisms of glucocorticoid action: what is important? Thorax 55:603–613
Castro-Rodriguez JA, Rodrigo GJ (2009) Efficacy of inhaled corticosteroids in infants and preschoolers with recurrent wheezing and asthma: a systematic review with meta-analysis. Pediatrics 123:e519–e525
Bacharier LB, Guilbert TW, Zeiger RS et al (2009) Patient characteristics associated with improved outcomes with use of an inhaled corticosteroid in preschool children at risk for asthma. J Allergy Clin Immunol 123:1077–1082, 1082 e1071-1075
Murray CS, Woodcock A, Langley SJ, Morris J, Custovic A, Team I.S. (2006) Secondary prevention of asthma by the use of Inhaled fluticasone propionate in wheezy infants (IFWIN): double-blind, randomised, controlled study. Lancet 368:754–762
Donahue JG, Weiss ST, Livingston JM, Goetsch MA, Greineder DK, Platt R (1997) Inhaled steroids and the risk of hospitalization for asthma. JAMA 277:887–891
Adams, N.P., Bestall, J.B., Malouf, R., Lasserson, T.J. and Jones, P.W. (2005), Inhaled beclomethasone versus placebo for chronic asthma. Cochrane Database Syst Rev. CD002738
Masoli M, Weatherall M, Holt S, Beasley R (2004) Clinical dose–response relationship of fluticasone propionate in adults with asthma. Thorax 59:16–20
Masoli M, Weatherall M, Holt S, Beasley R (2004) Systematic review of the dose–response relation of inhaled fluticasone propionate. Arch Dis Child 89:902–907
Bousquet J, Ben-Joseph R, Messonnier M, Alemao E, Gould AL (2002) A meta-analysis of the dose–response relationship of inhaled corticosteroids in adolescents and adults with mild to moderate persistent asthma. Clin Ther 24:1–20
Szefler SJ, Martin RJ, King TS et al (2002) Significant variability in response to inhaled corticosteroids for persistent asthma. J Allergy Clin Immunol 109:410–418
Martin RJ, Szefler SJ, King TS et al (2007) The Predicting Response to Inhaled Corticosteroid Efficacy (PRICE) trial. J Allergy Clin Immunol 119:73–80
Anderson WJ, Short PM, Williamson PA, Lipworth BJ (2012) Inhaled corticosteroid dose response using domiciliary exhaled nitric oxide in persistent asthma: the FENOtype trial. Chest 142:1553–1561
Harrison TW, Oborne J, Newton S, Tattersfield AE (2004) Doubling the dose of inhaled corticosteroid to prevent asthma exacerbations: randomised controlled trial. Lancet 363:271–275
Reddel HK, Jenkins CR, Marks GB et al (2000) Optimal asthma control, starting with high doses of inhaled budesonide. Eur Respir J 16:226–235
Rank MA, Hagan JB, Park MA et al (2013) The risk of asthma exacerbation after stopping low-dose inhaled corticosteroids: a systematic review and meta-analysis of randomized controlled trials. J Allergy Clin Immunol 131:724–729
Ducharme, F.M., Ni Chroinin, M., Greenstone, I. and Lasserson, T.J. (2010), Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma. Cochrane Database Syst Rev. CD005533
Lazarus SC, Boushey HA, Fahy JV et al (2001) Long-acting beta2-agonist monotherapy vs continued therapy with inhaled corticosteroids in patients with persistent asthma: a randomized controlled trial. JAMA 285:2583–2593
Ducharme, F.M., Lasserson, T.J. and Cates, C.J. (2011), Addition to inhaled corticosteroids of long-acting beta2-agonists versus anti-leukotrienes for chronic asthma. Cochrane Database Syst Rev. CD003137
Lipworth BJ, Short PM, Williamson PA, Clearie KL, Fardon TC, Jackson CM (2012) A randomized primary care trial of steroid titration against mannitol in persistent asthma: STAMINA trial. Chest 141:607–615
Smith AD, Cowan JO, Brassett KP, Herbison GP, Taylor DR (2005) Use of exhaled nitric oxide measurements to guide treatment in chronic asthma. N Engl J Med 352:2163–2173
Jang AS (2012) Steroid response in refractory asthmatics. Korean J Intern Med 27:143–148
Barnes PJ (2013) Corticosteroid resistance in patients with asthma and chronic obstructive pulmonary disease. J Allergy Clin Immunol 131:636–645
Adcock IM, Barnes PJ (2008) Molecular mechanisms of corticosteroid resistance. Chest 134:394–401
Sher ER, Leung DY, Surs W et al (1994) Steroid-resistant asthma. Cellular mechanisms contributing to inadequate response to glucocorticoid therapy. J Clin Invest 93:33–39
Boushey HA, Sorkness CA, King TS et al (2005) Daily versus as-needed corticosteroids for mild persistent asthma. N Engl J Med 352:1519–1528
Rodrigo, G.J. and Castro-Rodriguez, J.A. (2013) Daily vs. intermittent inhaled corticosteroids for recurrent wheezing and mild persistent asthma: a systematic review with meta-analysis. Respir Med (in press)
Chauhan BF, Chartrand C, Ducharme FM (2013) Intermittent versus daily inhaled corticosteroids for persistent asthma in children and adults. Cochrane Database Syst Rev 2:CD009611
Turpeinen M, Nikander K, Pelkonen AS et al (2008) Daily versus as-needed inhaled corticosteroid for mild persistent asthma (The Helsinki early intervention childhood asthma study). Arch Dis Child 93:654–659
Paggiaro P (2009) New pharmacologic perspectives in pneumology: beclomethasone-formoterol extrafine. Open Respir Med J 3:38–42
Scichilone N, Battaglia S, Sorino C et al (2010) Effects of extra-fine inhaled beclomethasone/formoterol on both large and small airways in asthma. Allergy 65:897–902
Barnes PJ, Nicolini G, Bizzi A, Spinola M, Singh D (2012) Do inhaled corticosteroid/long-acting beta2-agonist fixed combinations provide superior clinical benefits compared with separate inhalers? A literature reappraisal. Allergy Asthma Proc 33:140–144
Kramer S, Rottier BL, Scholten RJ, Boluyt N (2013) Ciclesonide versus other inhaled corticosteroids for chronic asthma in children. Cochrane Database Syst Rev 2:CD010352
Patel M, Perrin K, Pritchard A et al (2013) Accuracy of patient self-report as a measure of inhaled asthma medication use. Respirology 18:546–552
Murphy AC, Proeschal A, Brightling CE et al (2012) The relationship between clinical outcomes and medication adherence in difficult-to-control asthma. Thorax 67:751–753
Heaney LG, Horne R (2012) Non-adherence in difficult asthma: time to take it seriously. Thorax 67:268–270
Gamble J, Stevenson M, Heaney LG (2011) A study of a multi-level intervention to improve non-adherence in difficult to control asthma. Respir Med 105:1308–1315
Reddel HK, Barnes DJ, Exacerbation Advisory Panel (2006) Pharmacological strategies for self-management of asthma exacerbations. Eur Respir J 28:182–199
FitzGerald JM, Becker A, Sears MR et al (2004) Doubling the dose of budesonide versus maintenance treatment in asthma exacerbations. Thorax 59:550–556
Quon, B.S., Fitzgerald, J.M., Lemiere, C., Shahidi, N. and Ducharme, F.M. (2010) Increased versus stable doses of inhaled corticosteroids for exacerbations of chronic asthma in adults and children. Cochrane Database Syst Rev. CD007524
Rowe, B.H., Spooner, C.H., Ducharme, F.M., Bretzlaff, J.A. and Bota, G.W. (2007) Corticosteroids for preventing relapse following acute exacerbations of asthma. Cochrane Database Syst Rev. CD000195
Edmonds ML, Milan SJ, Camargo CA Jr, Pollack CV, Rowe BH (2012) Early use of inhaled corticosteroids in the emergency department treatment of acute asthma. Cochrane Database Syst Rev 12:CD002308
Rowe, B.H., Spooner, C., Ducharme, F.M., Bretzlaff, J.A. and Bota, G.W. (2001) Early emergency department treatment of acute asthma with systemic corticosteroids. Cochrane Database Syst Rev. CD002178
Smith, M., Iqbal, S., Elliott, T.M., Everard, M. and Rowe, B.H. (2003) Corticosteroids for hospitalised children with acute asthma. Cochrane Database Syst Rev. CD002886
Manser, R., Reid, D. and Abramson, M. (2001) Corticosteroids for acute severe asthma in hospitalised patients. Cochrane Database Syst Rev. CD001740
Harrison BD, Stokes TC, Hart GJ, Vaughan DA, Ali NJ, Robinson AA (1986) Need for intravenous hydrocortisone in addition to oral prednisolone in patients admitted to hospital with severe asthma without ventilatory failure. Lancet 1:181–184
Ratto D, Alfaro C, Sipsey J, Glovsky MM, Sharma OP (1988) Are intravenous corticosteroids required in status asthmaticus? JAMA 260:527–529
Dembla G, Mundle RP, Salkar HR, Doifoide DV (2011) Oral versus intravenous steroids in acute exacerbation of asthma—randomized controlled study. J Assoc Physicians India 59:621–623
Chan JS, Cowie RL, Lazarenko GC, Little C, Scott S, Ford GT (2001) Comparison of intramuscular betamethasone and oral prednisone in the prevention of relapse of acute asthma. Can Respir J 8:147–152
Schuckman H, DeJulius DP, Blanda M, Gerson LW, DeJulius AJ, Rajaratnam M (1998) Comparison of intramuscular triamcinolone and oral prednisone in the outpatient treatment of acute asthma: a randomized controlled trial. Ann Emerg Med 31:333–338
Gries DM, Moffitt DR, Pulos E, Carter ER (2000) A single dose of intramuscularly administered dexamethasone acetate is as effective as oral prednisone to treat asthma exacerbations in young children. J Pediatr 136:298–303
Lahn M, Bijur P, Gallagher EJ (2004) Randomized clinical trial of intramuscular vs oral methylprednisolone in the treatment of asthma exacerbations following discharge from an emergency department. Chest 126:362–368
Rowe BH, Bota GW, Fabris L, Therrien SA, Milner RA, Jacono J (1999) Inhaled budesonide in addition to oral corticosteroids to prevent asthma relapse following discharge from the emergency department: a randomized controlled trial. JAMA 281:2119–2126
Edmonds ML, Milan SJ, Brenner BE, Camargo CA Jr, Rowe BH (2012) Inhaled steroids for acute asthma following emergency department discharge. Cochrane Database Syst Rev 12:CD002316
Rossi GA, Cerasoli F, Cazzola M (2007) Safety of inhaled corticosteroids: room for improvement. Pulm Pharmacol Ther 20:23–35
Dahl R (2006) Systemic side effects of inhaled corticosteroids in patients with asthma. Respir Med 100:1307–1317
Martin RJ, Szefler SJ, Chinchilli VM et al (2002) Systemic effect comparisons of six inhaled corticosteroid preparations. Am J Respir Crit Care Med 165:1377–1383
Shepherd, J., Rogers, G., Anderson, R., et al. (2008) Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in adults and children aged 12 years and over. Health Technol Assess. 12, iii–iv, 1–360
Patel M, Pilcher J, Pritchard A et al (2013) Efficacy and safety of maintenance and reliever combination budesonide-formoterol inhaler in patients with asthma at risk of severe exacerbations: a randomised controlled trial. Lancet Respir Med 1:32–42
Rogers L, Reibman J (2011) Pharmacologic approaches to life-threatening asthma. Ther Adv Respir Dis 5:397–408
Blake KV (1999) Montelukast: data from clinical trials in the management of asthma. Ann Pharmacother 33:1299–1314
Yuksel B, Aydemir C, Ustundag G et al (2009) The effect of treatment with montelukast on levels of serum interleukin-10, eosinophil cationic protein, blood eosinophil counts, and clinical parameters in children with asthma. Turk J Pediatr 51:460–465
Bisgaard H, Nielsen KG (2000) Bronchoprotection with a leukotriene receptor antagonist in asthmatic preschool children. Am J Respir Crit Care Med 162:187–190
Garcia Garcia ML, Wahn U, Gilles L, Swern A, Tozzi CA, Polos P (2005) Montelukast, compared with fluticasone, for control of asthma among 6- to 14-year-old patients with mild asthma: the MOSAIC study. Pediatrics 116:360–369
Zeiger RS, Bird SR, Kaplan MS et al (2005) Short-term and long-term asthma control in patients with mild persistent asthma receiving montelukast or fluticasone: a randomized controlled trial. Am J Med 118:649–657
Zeiger RS, Szefler SJ, Phillips BR et al (2006) Response profiles to fluticasone and montelukast in mild-to-moderate persistent childhood asthma. J Allergy Clin Immunol 117:45–52
Busse W, Raphael GD, Galant S et al (2001) Low-dose fluticasone propionate compared with montelukast for first-line treatment of persistent asthma: a randomized clinical trial. J Allergy Clin Immunol 107:461–468
Malmstrom K, Rodriguez-Gomez G, Guerra J et al (1999) Oral montelukast, inhaled beclomethasone, and placebo for chronic asthma. A randomized, controlled trial. Montelukast/Beclomethasone Study Group. Ann Intern Med 130:487–495
Ducharme FM, Noya FJ, Allen-Ramey FC, Maiese EM, Gingras J, Blais L (2012) Clinical effectiveness of inhaled corticosteroids versus montelukast in children with asthma: prescription patterns and patient adherence as key factors. Curr Med Res Opin 28:111–119
Szefler SJ, Phillips BR, Martinez FD et al (2005) Characterization of within-subject responses to fluticasone and montelukast in childhood asthma. J Allergy Clin Immunol 115:233–242
Jenkins CR, Thien FC, Wheatley JR, Reddel HK (2005) Traditional and patient-centred outcomes with three classes of asthma medication. Eur Respir J 26:36–44
Jartti T (2008) Inhaled corticosteroids or montelukast as the preferred primary long-term treatment for pediatric asthma? Eur J Pediatr 167:731–736
Price D, Popov TA, Bjermer L et al (2013) Effect of montelukast for treatment of asthma in cigarette smokers. J Allergy Clin Immunol 131:763–771
Lipworth BJ, Basu K, Donald HP et al (2013) Tailored second-line therapy in asthmatic children with the Arg(16) genotype. Clin Sci (Lond) 124:521–528
Cuevas Hernandez MM, Arias Hernandez RM (2004) Therapeutic effects of an antileukotriene in children with moderate-severe persistent asthma. Rev Alerg Mex 51:206–209
Cakmak G, Demir T, Gemicioglu B, Aydemir A, Serdaroglu E, Donma O (2004) The effects of add-on zafirlukast treatment to budesonide on bronchial hyperresponsiveness and serum levels of eosinophilic cationic protein and total antioxidant capacity in asthmatic patients. Tohoku J Exp Med 204:249–256
Matsuse H, Fukahori S, Tsuchida T et al (2012) Effects of a short course of pranlukast combined with systemic corticosteroid on acute asthma exacerbation induced by upper respiratory tract infection. J Asthma 49:637–641
Bleecker ER, Welch MJ, Weinstein SF et al (2000) Low-dose inhaled fluticasone propionate versus oral zafirlukast in the treatment of persistent asthma. J Allergy Clin Immunol 105:1123–1129
Busse W, Wolfe J, Storms W et al (2001) Fluticasone propionate compared with zafirlukast in controlling persistent asthma: a randomized double-blind, placebo-controlled trial. J Fam Pract 50:595–602
Nathan RA, Bleecker ER, Kalberg C, Fluticasone Propionate Study, G (2001) A comparison of short-term treatment with inhaled fluticasone propionate and zafirlukast for patients with persistent asthma. Am J Med 111:195–202
Brabson JH, Clifford D, Kerwin E et al (2002) Efficacy and safety of low-dose fluticasone propionate compared with zafirlukast in patients with persistent asthma. Am J Med 113:15–21
Twaites BR, Wilton LV, Shakir SA (2007) Safety of zafirlukast: results of a postmarketing surveillance study on 7976 patients in England. Drug Saf 30:419–429
Watts K, Chavasse RJ (2012) Leukotriene receptor antagonists in addition to usual care for acute asthma in adults and children. Cochrane Database Syst Rev 5:CD006100
Lazarus SC, Lee T, Kemp JP et al (1998) Safety and clinical efficacy of zileuton in patients with chronic asthma. Am J Manag Care 4:841–848
Kubavat AH, Khippal N, Tak S et al (2013) A randomized, comparative, multicentric clinical trial to assess the efficacy and safety of zileuton extended-release tablets with montelukast sodium tablets in patients suffering from chronic persistent asthma. Am J Ther 20:154–162
O’Connor BJ, Lofdahl CG, Balter M, Szczeklik A, Boulet LP, Cairns CB (2007) Zileuton added to low-dose inhaled beclomethasone for the treatment of moderate to severe persistent asthma. Respir Med 101:1088–1096
Gelb AF, Taylor CF, Simmons M, Shinar C (2009) Role of add-on zileuton on total exhaled, large airway, and small airway/alveolar nitric oxide in moderate-severe persistent adult asthmatics on fluticasone 250 microg/Salmeterol 50 microg. Pulm Pharmacol Ther 22:516–521
Tantisira KG, Lima J, Sylvia J, Klanderman B, Weiss ST (2009) 5-lipoxygenase pharmacogenetics in asthma: overlap with Cys-leukotriene receptor antagonist loci. Pharmacogenet Genomics 19:244–247
Nelson H, Kemp J, Berger W et al (2007) Efficacy of zileuton controlled-release tablets administered twice daily in the treatment of moderate persistent asthma: a 3-month randomized controlled study. Ann Allergy Asthma Immunol 99:178–184
Chauhan BF, Ducharme FM (2012) Anti-leukotriene agents compared to inhaled corticosteroids in the management of recurrent and/or chronic asthma in adults and children. Cochrane Database Syst Rev 5:CD002314
Garcia-Marcos L, Schuster A, Perez-Yarza EG (2003) Benefit-risk assessment of antileukotrienes in the management of asthma. Drug Saf 26:483–518
Wenzel S, Busse W, Calhoun W et al (2007) The safety and efficacy of zileuton controlled-release tablets as adjunctive therapy to usual care in the treatment of moderate persistent asthma: a 6-month randomized controlled study. J Asthma 44:305–310
Watkins PB, Dube LM, Walton-Bowen K, Cameron CM, Kasten LE (2007) Clinical pattern of zileuton-associated liver injury: results of a 12-month study in patients with chronic asthma. Drug Saf 30:805–815
Bush A, Saglani S (2010) Management of severe asthma in children. Lancet 376:814–825
Netzer NC, Kupper T, Voss HW, Eliasson AH (2012) The actual role of sodium cromoglycate in the treatment of asthma—a critical review. Sleep Breath 16:1027–1032
Adams RJ, Fuhlbrigge A, Finkelstein JA et al (2001) Impact of inhaled antiinflammatory therapy on hospitalization and emergency department visits for children with asthma. Pediatrics 107:706–711
Guevara, J.P., Ducharme, F.M., Keren, R., Nihtianova, S. and Zorc, J. (2006), Inhaled corticosteroids versus sodium cromoglycate in children and adults with asthma. Cochrane Database Syst Rev. CD003558
Tasche MJ, Uijen JH, Bernsen RM, de Jongste JC, van der Wouden JC (2000) Inhaled disodium cromoglycate (DSCG) as maintenance therapy in children with asthma: a systematic review. Thorax 55:913–920
van der Wouden, J.C., Uijen, J.H., Bernsen, R.M., Tasche, M.J., de Jongste, J.C. and Ducharme, F. (2008), Inhaled sodium cromoglycate for asthma in children. Cochrane Database Syst Rev. CD002173
Keller M, Schierholz J (2011) Have inadequate delivery systems hampered the clinical success of inhaled disodium cromoglycate? Time for reconsideration. Expert Opin Drug Deliv 8:1–17
Katayama H, Yokoyama A, Fujino S et al (1996) Near-death asthmatic reaction induced by disodium cromoglycate. Intern Med 35:976–978
Barnes, P.J. (2013) Theophylline. Am J Respir Crit Care Med. doi: 10.1164/rccm.201302-0388PP
Kidney J, Dominguez M, Taylor PM, Rose M, Chung KF, Barnes PJ (1995) Immunomodulation by theophylline in asthma. Demonstration by withdrawal of therapy. Am J Respir Crit Care Med 151:1907–1914
MacLeod D, Djukanovic R (1996) Low-dose theophylline: a new anti-inflammatory role in asthma management? Monaldi Arch Chest Dis 51:30–34
Jaffar ZH, Sullivan P, Page C, Costello J (1996) Low-dose theophylline modulates T-lymphocyte activation in allergen-challenged asthmatics. Eur Respir J 9:456–462
Huang SD, Yang J, Zhang SY, Tian LQ, Pan QH (2006) Clinical efficacy of low-dose oral theophylline for treating mild asthma. Nan Fang Yi Ke Da Xue Xue Bao 26:325–327
Lim S, Tomita K, Caramori G et al (2001) Low-dose theophylline reduces eosinophilic inflammation but not exhaled nitric oxide in mild asthma. Am J Respir Crit Care Med 164:273–276
Barnes PJ (2009) Histone deacetylase-2 and airway disease. Ther Adv Respir Dis 3:235–243
Nakano J, Yano T, Yamamura K et al (2006) Aminophilline suppress the release of chemical mediators in treatment of acute asthma. Respir Med 100:542–550
Yung M, South M (1998) Randomised controlled trial of aminophylline for severe acute asthma. Arch Dis Child 79:405–410
D’Avila RS, Piva JP, Marostica PJ, Amantea SL (2008) Early administration of two intravenous bolus of aminophylline added to the standard treatment of children with acute asthma. Respir Med 102:156–161
Wheeler DS, Jacobs BR, Kenreigh CA, Bean JA, Hutson TK, Brilli RJ (2005) Theophylline versus terbutaline in treating critically ill children with status asthmaticus: a prospective, randomized, controlled trial. Pediatr Crit Care Med 6:142–147
Littenberg B (1988) Aminophylline treatment in severe, acute asthma. A meta-analysis. JAMA 259:1678–1684
Parameswaran, K., Belda, J. and Rowe, B.H. (2000), Addition of intravenous aminophylline to beta2-agonists in adults with acute asthma. Cochrane Database Syst Rev. CD002742
Reed CE, Offord KP, Nelson HS, Li JT, Tinkelman DG (1998) Aerosol beclomethasone dipropionate spray compared with theophylline as primary treatment for chronic mild-to-moderate asthma. The American Academy of Allergy, Asthma and Immunology Beclomethasone Dipropionate-Theophylline Study Group. J Allergy Clin Immunol 101:14–23
Spears M, Donnelly I, Jolly L et al (2009) Effect of low-dose theophylline plus beclometasone on lung function in smokers with asthma: a pilot study. Eur Respir J 33:1010–1017
American Lung Association Asthma Clinical Research Center (2007) Clinical trial of low-dose theophylline and montelukast in patients with poorly controlled asthma. Am J Respir Crit Care Med 175:235–242
Tinkelman DG, Reed CE, Nelson HS, Offord KP (1993) Aerosol beclomethasone dipropionate compared with theophylline as primary treatment of chronic, mild to moderately severe asthma in children. Pediatrics 92:64–77
Evans DJ, Taylor DA, Zetterstrom O, Chung KF, O’Connor BJ, Barnes PJ (1997) A comparison of low-dose inhaled budesonide plus theophylline and high-dose inhaled budesonide for moderate asthma. N Engl J Med 337:1412–1418
Dahl R, Larsen BB, Venge P (2002) Effect of long-term treatment with inhaled budesonide or theophylline on lung function, airway reactivity and asthma symptoms. Respir Med 96:432–438
Suessmuth S, Freihorst J, Gappa M (2003) Low-dose theophylline in childhood asthma: a placebo-controlled, double-blind study. Pediatr Allergy Immunol 14:394–400
Dombrowski MP, Schatz M, Wise R et al (2004) Randomized trial of inhaled beclomethasone dipropionate versus theophylline for moderate asthma during pregnancy. Am J Obstet Gynecol 190:737–744
Adachi M, Aizawa H, Ishihara K et al (2008) Comparison of salmeterol/fluticasone propionate (FP) combination with FP + sustained release theophylline in moderate asthma patients. Respir Med 102:1055–1064
Holimon TD, Chafin CC, Self TH (2001) Nocturnal asthma uncontrolled by inhaled corticosteroids: theophylline or long-acting beta2 agonists? Drugs 61:391–418
Yurdakul AS, Taci N, Eren A, Sipit T (2003) Comparative efficacy of once-daily therapy with inhaled corticosteroid, leukotriene antagonist or sustained-release theophylline in patients with mild persistent asthma. Respir Med 97:1313–1319
Seddon, P., Bara, A., Ducharme, F.M. and Lasserson, T.J. (2006) Oral xanthines as maintenance treatment for asthma in children. Cochrane Database Syst Rev. CD002885
Fan Chung K (2006) Phosphodiesterase inhibitors in airways disease. Eur J Pharmacol 533:110–117
Page CP, Spina D (2012) Selective PDE inhibitors as novel treatments for respiratory diseases. Curr Opin Pharmacol 12:275–286
Hatzelmann A, Morcillo EJ, Lungarella G et al (2010) The preclinical pharmacology of roflumilast—a selective, oral phosphodiesterase 4 inhibitor in development for chronic obstructive pulmonary disease. Pulm Pharmacol Ther 23:235–256
van Schalkwyk E, Strydom K, Williams Z et al (2005) Roflumilast, an oral, once-daily phosphodiesterase 4 inhibitor, attenuates allergen-induced asthmatic reactions. J Allergy Clin Immunol 116:292–298
Louw C, Williams Z, Venter L et al (2007) Roflumilast, a phosphodiesterase 4 inhibitor, reduces airway hyperresponsiveness after allergen challenge. Respiration 74:411–417
Gauvreau GM, Boulet LP, Schmid-Wirlitsch C et al (2011) Roflumilast attenuates allergen-induced inflammation in mild asthmatic subjects. Respir Res 12:140
Timmer W, Leclerc V, Birraux G et al (2002) The new phosphodiesterase 4 inhibitor roflumilast is efficacious in exercise-induced asthma and leads to suppression of LPS-stimulated TNF-alpha ex vivo. J Clin Pharmacol 42:297–303
Bousquet J, Aubier M, Sastre J et al (2006) Comparison of roflumilast, an oral anti-inflammatory, with beclomethasone dipropionate in the treatment of persistent asthma. Allergy 61:72–78
Bateman ED, Izquierdo JL, Harnest U et al (2006) Efficacy and safety of roflumilast in the treatment of asthma. Ann Allergy Asthma Immunol 96:679–686
Holgate ST, Polosa R (2008) Treatment strategies for allergy and asthma. Nat Rev Immunol 8:218–230
Abramson, M.J., Puy, R.M. and Weiner, J.M. (2010), Injection allergen immunotherapy for asthma. Cochrane Database Syst Rev. CD001186
Lin SY, Erekosima N, Kim JM et al (2013) Sublingual immunotherapy for the treatment of allergic rhinoconjunctivitis and asthma: a systematic review. JAMA 309:1278–1288
Busse W, Corren J, Lanier BQ et al (2001) Omalizumab, anti-IgE recombinant humanized monoclonal antibody, for the treatment of severe allergic asthma. J Allergy Clin Immunol 108:184–190
Soler M, Matz J, Townley R et al (2001) The anti-IgE antibody omalizumab reduces exacerbations and steroid requirement in allergic asthmatics. Eur Respir J 18:254–261
Humbert M, Beasley R, Ayres J et al (2005) Benefits of omalizumab as add-on therapy in patients with severe persistent asthma who are inadequately controlled despite best available therapy (GINA 2002 step 4 treatment): INNOVATE. Allergy 60:309–316
Hanania NA, Alpan O, Hamilos DL et al (2011) Omalizumab in severe allergic asthma inadequately controlled with standard therapy: a randomized trial. Ann Intern Med 154:573–582
Walker, S., Monteil, M., Phelan, K., Lasserson, T.J. and Walters, E.H. (2006), Anti-IgE for chronic asthma in adults and children. Cochrane Database Syst Rev. CD003559
Burch J, Griffin S, McKenna C et al (2012) Omalizumab for the treatment of severe persistent allergic asthma in children aged 6–11 years: a NICE single technology appraisal. Pharmacoeconomics 30:991–1004
Walker S, Burch J, McKenna C, Wright K, Griffin S, Woolacott N (2011) Omalizumab for the treatment of severe persistent allergic asthma in children aged 6–11 years. Health Technol Assess 15(Suppl 1):13–21
Jones J, Shepherd J, Hartwell D et al (2009) Omalizumab for the treatment of severe persistent allergic asthma. Health Technol Assess 13(Suppl 2):31–39
Diaz R, Charles Z, George E, Adler A (2013) NICE guidance on omalizumab for severe asthma. Lancet Respir Med 1:189–190
Rambasek TE, Lang DM, Kavuru MS (2004) Omalizumab: where does it fit into current asthma management? Cleve Clin J Med 71:251–261
Busse W, Buhl R, Fernandez Vidaurre C et al (2012) Omalizumab and the risk of malignancy: results from a pooled analysis. J Allergy Clin Immunol 129(983–989):e986
Rowe BH, Camargo CA Jr (2008) The role of magnesium sulfate in the acute and chronic management of asthma. Curr Opin Pulm Med 14:70–76
Song WJ, Chang YS (2012) Magnesium sulfate for acute asthma in adults: a systematic literature review. Asia Pac Allergy 2:76–85
Shan Z, Rong Y, Yang W et al (2013) Intravenous and nebulized magnesium sulfate for treating acute asthma in adults and children: a systematic review and meta-analysis. Respir Med 107:321–330
Fogarty A, Lewis SA, Scrivener SL et al (2003) Oral magnesium and vitamin C supplements in asthma: a parallel group randomized placebo-controlled trial. Clin Exp Allergy 33:1355–1359
Gontijo-Amaral C, Ribeiro MA, Gontijo LS, Condino-Neto A, Ribeiro JD (2007) Oral magnesium supplementation in asthmatic children: a double-blind randomized placebo-controlled trial. Eur J Clin Nutr 61:54–60
Kazaks AG, Uriu-Adams JY, Albertson TE, Shenoy SF, Stern JS (2010) Effect of oral magnesium supplementation on measures of airway resistance and subjective assessment of asthma control and quality of life in men and women with mild to moderate asthma: a randomized placebo controlled trial. J Asthma 47:83–92
Mohammed S, Goodacre S (2007) Intravenous and nebulised magnesium sulphate for acute asthma: systematic review and meta-analysis. Emerg Med J 24:823–830
Torres S, Sticco N, Bosch JJ et al (2012) Effectiveness of magnesium sulfate as initial treatment of acute severe asthma in children, conducted in a tertiary-level university hospital: a randomized, controlled trial. Arch Argent Pediatr 110:291–296
Blitz M, Blitz S, Hughes R et al (2005) Aerosolized magnesium sulfate for acute asthma: a systematic review. Chest 128:337–344
Powell C, Dwan K, Milan SJ et al (2012) Inhaled magnesium sulfate in the treatment of acute asthma. Cochrane Database Syst Rev 12:CD003898
Villeneuve EJ, Zed PJ (2006) Nebulized magnesium sulfate in the management of acute exacerbations of asthma. Ann Pharmacother 40:1118–1124
Zervas E, Papatheodorou G, Psathakis K, Panagou P, Georgatou N, Loukides S (2003) Reduced intracellular Mg concentrations in patients with acute asthma. Chest 123:113–118
Hess DR, Fink JB, Venkataraman ST, Kim IK, Myers TR, Tano BD (2006) The history and physics of heliox. Respir Care 51:608–612
Fink JB (2006) Opportunities and risks of using heliox in your clinical practice. Respir Care 51:651–660
Kim IK, Saville AL, Sikes KL, Corcoran TE (2006) Heliox-driven albuterol nebulization for asthma exacerbations: an overview. Respir Care 51:613–618
Brandao DC, Britto MC, Pessoa MF et al (2011) Heliox and forward-leaning posture improve the efficacy of nebulized bronchodilator in acute asthma: a randomized trial. Respir Care 56:947–952
Alcoforado, L., Brandao, S., Rattes, C., et al. (2013), Evaluation of lung function and deposition of aerosolized bronchodilators carried by heliox associated with positive expiratory pressure in stable asthmatics: a randomized clinical trial. Respir Med (in press)
Bigham MT, Jacobs BR, Monaco MA et al (2010) Helium/oxygen-driven albuterol nebulization in the management of children with status asthmaticus: a randomized, placebo-controlled trial. Pediatr Crit Care Med 11:356–361
Colebourn CL, Barber V, Young JD (2007) Use of helium-oxygen mixture in adult patients presenting with exacerbations of asthma and chronic obstructive pulmonary disease: a systematic review. Anaesthesia 62:34–42
Kass JE, Castriotta RJ (1995) Heliox therapy in acute severe asthma. Chest 107:757–760
Kass JE, Terregino CA (1999) The effect of heliox in acute severe asthma: a randomized controlled trial. Chest 116:296–300
Ho AM, Lee A, Karmakar MK, Dion PW, Chung DC, Contardi LH (2003) Heliox vs air-oxygen mixtures for the treatment of patients with acute asthma: a systematic overview. Chest 123:882–890
Rodrigo, G., Pollack, C., Rodrigo, C. and Rowe, B.H. (2006) Heliox for nonintubated acute asthma patients. Cochrane Database Syst Rev. CD002884
Apter AJ (2013) Advances in adult asthma diagnosis and treatment in 2012: potential therapeutics and gene-environment interactions. J Allergy Clin Immunol 131:47–54
Barnes PJ (2006) New therapies for asthma. Trends Mol Med 12:515–520
Portelli M, Sayers I (2012) Genetic basis for personalized medicine in asthma. Expert Rev Respir Med 6:223–236
Pelaia G, Vatrella A, Maselli R (2012) The potential of biologics for the treatment of asthma. Nat Rev Drug Discov 11:958–972
Ingram JL, Kraft M (2012) IL-13 in asthma and allergic disease: asthma phenotypes and targeted therapies. J Allergy Clin Immunol 130:829–842, quiz 843–824
Corren J, Lemanske RF, Hanania NA et al (2011) Lebrikizumab treatment in adults with asthma. N Engl J Med 365:1088–1098
Woodruff PG, Modrek B, Choy DF et al (2009) T-helper type 2-driven inflammation defines major subphenotypes of asthma. Am J Respir Crit Care Med 180:388–395
Wenzel S, Ford L, Pearlman D et al (2013) Dupilumab in persistent asthma with elevated eosinophil levels. N Engl J Med 368:2455–2466
Haldar P, Brightling CE, Hargadon B et al (2009) Mepolizumab and exacerbations of refractory eosinophilic asthma. N Engl J Med 360:973–984
Pavord ID, Korn S, Howarth P et al (2012) Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial. Lancet 380:651–659
Beeh KM, Kanniess F, Wagner F et al (2013) The novel TLR-9 agonist QbG10 shows clinical efficacy in persistent allergic asthma. J Allergy Clin Immunol 131:866–874
Desai D, Brightling C (2010) TNF-alpha antagonism in severe asthma? Recent Pat Inflamm Allergy Drug Discov 4:193–200
Matera MG, Calzetta L, Cazzola M (2010) TNF-alpha inhibitors in asthma and COPD: we must not throw the baby out with the bath water. Pulm Pharmacol Ther 23:121–128
Hahn DL, Grasmick M, Hetzel S, Yale S, AZMATICS (Azithromycin-Asthma Trial in Community Settings) Study Group (2012) Azithromycin for bronchial asthma in adults: an effectiveness trial. J Am Board Fam Med 25:442–459
Silva D, Couto M, Delgado L, Moreira A (2012) A systematic review of statin efficacy in asthma. J Asthma 49:885–894
Jat KR, Chawla D (2012) Ketamine for management of acute exacerbations of asthma in children. Cochrane Database Syst Rev 11:CD009293
Silverman RA, Foley F, Dalipi R, Kline M, Lesser M (2012) The use of rhDNAse in severely ill, non-intubated adult asthmatics refractory to bronchodilators: a pilot study. Respir Med 106:1096–1102
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Albertson, T.E., Schivo, M., Gidwani, N. et al. Pharmacotherapy of Critical Asthma Syndrome: Current and Emerging Therapies. Clinic Rev Allerg Immunol 48, 7–30 (2015). https://doi.org/10.1007/s12016-013-8393-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-013-8393-8