Abstract
Background
Historically, achieving stability for the unstable total hip arthroplasty (THA) with revision surgery has been achieved inconsistently. Most of what we know about this topic comes from reports of high-volume surgeons’ results; the degree to which these results are achieved in the community is largely unknown, but insofar as most joint replacements are done by community surgeons, the issue is important.
Questions/purposes
We used a community joint registry to determine: (1) the frequency of repeat revision after surgery to treat the unstable THA; (2) what surgical approaches to this problem are in common use in the community now; (3) are there differences in repeat revision frequency that vary by approach used; and (4) has the frequency of repeat revision decreased over time as surgical technique and implant options have evolved?
Methods
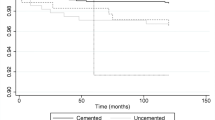
We reviewed 6801 primary THAs performed in our community joint registry over the last 20 years. One hundred eighteen patients (1.7%) with a mean age of 67 years were revised within the registry for instability/dislocation. Failure was defined as a return to the operating room for rerevision surgery for instability. Minimum followup was 2 years (average, 9.4 years; range, 2–20 years) with six patients having incomplete followup. The frequency of rerevisions was calculated and compared using Pearson’s chi-square test. Cumulative rerevision rates were calculated using the Kaplan-Meier method and types of revision procedures were compared using the log-rank test.
Results
The initial revision procedure was successful in 108 patients (92%); 10 patients underwent repeat surgery for recurrent dislocation after their initial revision surgery. The most frequently performed procedure was revision of the head and liner only (35 of 118 [30%]); constrained devices were used in 19% (22 of 118) of the procedures. There was no difference in the cumulative rerevision rates for instability or dislocation by type of revision procedure performed. Six of 22 constrained liners were rerevised for varying indications. There was no difference in frequency of repeat revision for instability between those patients revised for THAs performed before 2003 and those managed more recently.
Conclusions
Revision surgery for unstable THA is successfully managed in the community with a variety of surgical interventions. Identifying the reason for dislocation and addressing the source remain paramount. Constrained liners should be used with caution; although typically used in the most problematic settings, rerevision for a variety of failure modes remains troublesome.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.


Similar content being viewed by others
References
Alberton GM, High WA, Morrey BF. Dislocation after revision total hip arthroplasty: an analysis of risk factors and treatment options. J Bone Joint Surg Am. 2002;84:1788–1792.
Anderson MJ, Murray WR, Skinner HB. Constrained acetabular components. J Arthroplasty. 1994;9:17–23.
Berry DJ, von KM, Schleck CD, Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2456–2463.
Biviji AA, Ezzet KA, Pulido P, Colwell CW Jr. Modular femoral head and liner exchange for the unstable total hip arthroplasty. J Arthroplasty. 2009;24:625–630.
Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:128–133.
D’Angelo F, Murena L, Zatti G, Cherubino P. The unstable total hip replacement. Indian J Orthop. 2008;42:252–259.
Daly PJ, Morrey BF. Operative correction of an unstable total hip arthroplasty. J Bone Joint Surg Am. 1992;74:1334–1343.
Della Valle CJ, Chang D, Sporer S, Berger RA, Rosenberg AG, Paprosky WG. High failure rate of a constrained acetabular liner in revision total hip arthroplasty. J Arthroplasty. 2005;20:103–107.
Dobzyniak M, Fehring TK, Odum S. Early failure in total hip arthroplasty. Clin Orthop Relat Res. 2006;447:76–78.
Earll MD, Fehring TK, Griffin WL, Mason JB, McCoy T, Odum S. Success rate of modular component exchange for the treatment of an unstable total hip arthroplasty. J Arthroplasty. 2002;17:864–869.
Gioe TJ, Killeen KK, Mehle S, Grimm K. Implementation and application of a community total joint registry: a twelve-year history. J Bone Joint Surg Am. 2006;88:1399–1404.
Gioe TJ, Sinner P, Mehle S, Ma W, Killeen KK. Excellent survival of all-polyethylene tibial components in a community joint registry. Clin Orthop Relat Res. 2007;464:88–92.
Howie DW, Holubowycz OT, Middleton R; Large Articulation Study Group. Large femoral heads decrease the incidence of dislocation after total hip arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2012;94:1095–1102.
Jacobs JJ. Large (36 or 40-mm) femoral heads decreased the rate of dislocation after revision total hip arthroplasty. J Bone Joint Surg Am. 2012;94:2095.
Jafari SM, Coyle C, Mortazavi SM, Sharkey PF, Parvizi J. Revision hip arthroplasty: infection is the most common cause of failure. Clin Orthop Relat Res. 2010;468:2046–2051.
Jameson SS, Lees D, James P, Serrano-Pedraza I, Partington PF, Muller SD, Meek RM, Reed MR. Lower rates of dislocation with increased femoral head size after primary total hip replacement: a five-year analysis of NHS patients in England. J Bone Joint Surg Br. 2011;93:876–880.
Katz JN, Losina E, Barrett J, Phillips CB, Mahomed NN, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States Medicare population. J Bone Joint Surg Am. 2001;83:1622–1629.
Kostensalo I, Junnila M, Virolainen P, Remes V, Matilainen M, Vahlberg T, Pulkkinen P, Eskelinen A, Mäkelä KT. Effect of femoral head size on risk of revision for dislocation after total hip arthroplasty. Acta Orthop. 2013;84:342–347.
Lachiewicz PF, Soileau E, Ellis J. Modular revision for recurrent dislocation of primary or revision total hip arthroplasty. J Arthroplasty. 2004;19:424–429.
Li E, Meding JB, Ritter MA, Keating EM, Faris PM. The natural history of a posteriorly dislocated total hip replacement. J Arthroplasty. 1999;14:964–968.
Malchau H, Herberts P, Eisler T, Garellick G, Soderman P. The Swedish Total Hip Replacement Register. J Bone Joint Surg Am. 2002;84(Suppl 2):2–20.
Nadaud MC, Fehring TK, Odum S, Mason JB, Griffin WL, McCoy TH. Bipolar reconstruction for recurrent instability of the hip. Orthopedics. 2004;27:746–751.
Sanchez-Sotelo J, Berry DJ. Epidemiology of instability after total hip replacement. Orthop Clin North Am. 2001;32:543–552, vii.
Schneider L, Philippot R, Boyer B, Farizon F. Revision total hip arthroplasty using a reconstruction cage device and a cemented dual mobility cup. Orthop Traumatol Surg Res. 2011;97:807–813.
Sikes CV, Lai LP, Schreiber M, Mont MA, Jinnah RH, Seyler TM. Instability after total hip arthroplasty: treatment with large femoral heads vs constrained liners. J Arthroplasty. 2008;23:59–63.
Skeels MD, Berend KR, Lombardi AV Jr. The dislocator, early and late: the role of large heads. Orthopedics. 2009;32:9.
Stroh DA, Issa K, Johnson AJ, Delanois RE, Mont MA. Reduced dislocation rates and excellent functional outcomes with large-diameter femoral heads. J Arthroplasty. 2013;28:1415–1420.
Tarasevicius S, Kesteris U, Robertsson O, Wingstrand H. Femoral head diameter affects the revision rate in total hip arthroplasty: an analysis of 1,720 hip replacements with 9–21 years of follow-up. Acta Orthop. 2006;77:706–709.
Wetters NG, Murray TG, Moric M, Sporer SM, Paprosky WG, Della Valle CJ. Risk factors for dislocation after revision total hip arthroplasty. Clin Orthop Relat Res. 2013;471:410–416.
Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295–1306.
Acknowledgments
We thank Lisa Courneya for her assistance with the database and her work with the surgeons’ office staff.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at HealthEast Care System, St Paul, MN, USA.
About this article
Cite this article
Salassa, T., Hoeffel, D., Mehle, S. et al. Efficacy of Revision Surgery for the Dislocating Total Hip Arthroplasty: Report From a Large Community Registry. Clin Orthop Relat Res 472, 962–967 (2014). https://doi.org/10.1007/s11999-013-3344-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-013-3344-5