Opinion statement
Infiltrative heart disease is caused by the deposition of abnormal substances in the heart and can lead to abnormalities in cardiac function and electrical conduction. Advances in non-invasive cardiovascular imaging have allowed for improved diagnosis of infiltrative heart disease, as well as ways to track disease progression or regression, thus enabling a mechanism to follow response to therapy. In this review, we provide an overview of the role of imaging in the diagnosis and management of cardiac sarcoidosis (CS) and cardiac amyloidosis (CA), as well as outline a proposed algorithm for using non-invasive cardiovascular imaging for evaluating these conditions.
Similar content being viewed by others
Introduction
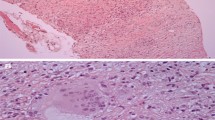
Infiltrative heart disease is caused by the deposition of abnormal substances in the heart [1]. While the myocardium is most often involved, any part of the heart, including the pericardium and valves, can be affected. Advances in non-invasive cardiovascular imaging have allowed for the diagnosis of infiltrative heart disease, sometimes avoiding the need for endomyocardial biopsy. Identifying the cause of infiltrative heart disease is important as prognosis and treatment vary across the different subtypes. A review of all of the causes of infiltrative heart disease and how they can be identified by non-invasive imaging has been done previously [1]. In this review, we will focus on the role of imaging in the diagnosis and management of cardiac sarcoidosis (CS) and cardiac amyloidosis (CA) (Fig. 1).
A proposed algorithm for using non-invasive cardiovascular imaging to make the diagnosis of a cardiac sarcoidosis (CS) or b cardiac amyloidosis (CA). CMR cardiac magnetic resonance imaging, PET positron emission tomography, H&P history and physical examination, ECG electrocardiogram, TTE transthoracic echocardiogram, SPEP serum protein electrophoresis, UPEP urine protein electrophoresis, PYP pyrophosphate, SPECT single-photon emission computed tomography, TTR transthyretin, AL light chain. ** if suspicion for TTR despite monoclonal spike consider PYP SPECT and mass spectrometry.
Cardiac sarcoidosis
Sarcoidosis is a systemic disorder of unknown etiology characterized by the formation of non-caseating granulomas in multiple organs [2]. The annual incidence of sarcoidosis has been estimated at 5 to 40 cases per 100,000 persons in the USA and Europe [3]. CS affects at least 25% of patients with sarcoidosis and may present with heart failure, left ventricular systolic dysfunction, conduction abnormalities, atrial or ventricular arrhythmias, or sudden cardiac death [4••, 5]. Identifying patients with CS is of importance as treatment with glucocorticoids may slow the progression of heart failure and implantable cardiac defibrillators (ICD) may improve survival [6,7,8,9].
Currently, clinical criteria from the Japanese Ministry of Health and Welfare (JMHW) and the Heart Rhythm Society (HRS) can be used to evaluate patients with suspected CS [10••, 11, 12]. However, these criteria have not been adequately validated and are neither sensitive nor specific for diagnosing CS [13]. As a result, in the absence of having a histological diagnosis from myocardial tissues, the HRS consensus statement proposes criteria for having “probable” CS, which is defined as a likelihood greater than 50% [10••]. In addition, in the absence of histological diagnosis from myocardial tissue, these criteria require the presence of extra-cardiac sarcoidosis, and thus cannot adequately evaluate patients who have isolated CS, whereby the disease is confined only to the heart [14]. However, the challenges related to diagnosing CS are not unique to these criteria as there is no reliable “gold reference” that can be used to establish the diagnosis of CS. As a result, both clinical criteria and imaging are often used to estimate the likelihood of CS rather than providing a definitive diagnosis. Given these challenges, there is an even greater role for non-invasive cardiovascular imaging to diagnose (or at least estimate the likelihood of having) cardiac sarcoidosis. In addition, imaging can be used to identify patients who may require additional treatments, such as immunosuppressive therapies, and to follow response to therapy.
Echocardiography
In patients who have extra-cardiac sarcoidosis, an abnormal transthoracic echocardiogram may be useful for diagnosing CS. While having systolic dysfunction, focal wall thinning or thickening, or a regional wall motion abnormality may be indicative of CS, the presence of diastolic dysfunction has been found to occur in patients who have pulmonary sarcoidosis who do not have any CS [15,16,17,18]. However, when compared to other imaging techniques, echocardiography has a limited role in screening patients with suspected CS due its poor sensitivity, particularly in early or localized disease [16]. One study found echocardiographic abnormalities in only 25% of patients who were found to have cardiac magnetic resonance imaging (CMR) or 18F-fluorodeoxyglucose (FDG) positron emission tomographic evidence of CS [19].
The development and advancement of echocardiographic strain imaging may result in an increase in its use for patients with suspected CS. One study evaluated 100 patients with systemic sarcoidosis who did not have known CS and found that when compared with age- and sex-matched controls, patients with sarcoidosis had impaired global longitudinal strain on echocardiography [20]. This finding was associated with a higher rate of cardiovascular events [20]. Strain imaging may also provide a method to assess response to therapy and follow patients with CS in the future [21].
Cardiac magnetic resonance imaging
CMR can detect areas of wall thinning or aneurysm and regional wall motion abnormalities like echocardiography and also does not use ionizing radiation. However, the main method by which CS can be diagnosed by CMR is the detection of midwall and subepicardial late gadolinium enhancement (LGE) [4••]. It should be noted, however, that LGE in a non-infarct pattern can also be seen when there is fibrosis after myocarditis or from other, often idiopathic, cardiomyopathies. CS can also rarely cause subendocardial LGE, which may mimic an infarct pattern [4••]. Multifocal LGE and LGE of the basal anteroseptum and inferoseptum with contiguous extension into the right ventricle favor the diagnosis of CS [4••].
In a study of 58 patients evaluating the accuracy of CMR in diagnosing CS compared to the JMWH criteria, CMR had a 100% sensitivity as it was able to diagnose all 12 patients who were positive by the clinical criteria [22]. However, among the 58 patients with extra-cardiac sarcoidosis, there were 19 (33%) patients with LGE, reflecting that CMR was much more sensitive at detecting CS [22]. The low specificity of CMR to detect CS in this study is likely secondary to the poor sensitivity of the JMHW criteria. Since the publication of this study, it has been widely recognized that there is no adequate reference standard against which to evaluate the diagnostic accuracy of imaging tests to detect CS. As a result, attention has shifted to identifying patients who are more likely to have adverse events, as it can be argued that regardless of the underlying diagnosis, these individuals may benefit from more aggressive therapies.
CMR, specifically the presence of LGE, has considerable prognostic value in CS. A recent meta-analysis including seven studies of 694 subjects, 199 of whom had LGE on their CMR, found that zero ventricular arrhythmias occurred in patients without LGE on their CMR [23•]. Cardiovascular mortality occurred in 10 LGE-positive versus two LGE-negative subjects (relative risk 10.7 [95% confidence interval, 1.34–86.3]; P = 0.03) [23•]. Thus, the absence of LGE is useful in identifying individuals who have a very low risk of future cardiac events.
Areas of development in CMR that may be of use in CS in the future include T2 mapping to identify and quantify areas of myocardial inflammation [24]. Future studies will need to determine how this technique compares to the use of FDG imaging for identifying and quantifying the amount of myocardial inflammation.
Cardiac positron emission tomography
Cardiac positron emission tomography (PET) involves performing a dedicated imaging scan to assess inflammation (FDG) and a separate scan to assess resting myocardial perfusion (82Rubidium or 13N-Ammonia) [4••]. Importantly, to suppress FDG from areas of normal myocardium, patient preparation using a high-fat/very low-carbohydrate diet is essential [25•, 26]. In early CS, focal areas of increased FDG uptake will be present with or without rest perfusion defects. Rest perfusion defects can signify the presence of scar but can also be seen with intense inflammation which compresses the microvasculature [4••]. The hallmark of CS with active inflammation on cardiac PET is a mismatch between metabolism and perfusion in the same area. Of note, though patient preparation is very different from PET studies that are used to assess for myocardial viability, this type of mismatch can also be seen in patients with obstructive coronary artery disease and hibernating myocardium. In more advanced disease, resting defects may be seen without inflammation, suggesting the presence of scar.
One advantage of PET imaging is that whole-body FDG imaging can be obtained concurrently with cardiac imaging to evaluate for extra-cardiac sarcoidosis [4••]. This information can be used to identify potential extra-cardiac sites for biopsy, as well as quantify the amount of extra-cardiac disease, which at times may be useful when deciding on the role of immunosuppressive therapy.
A meta-analysis that included seven studies and 164 patients found that cardiac PET had a sensitivity of 89% and a specificity of 78% of diagnosing CS when compared to the JMHW criteria [27]. Just as in CMR, the low specificity observed in this study may actually be secondary to the poor sensitivity of the clinical criteria.
Results of cardiac PET carry important prognostic information for patients with CS. In one recent study of 118 patients referred for cardiac PET because of known or suspected CS, those with abnormal myocardial perfusion and metabolism had a fourfold increase in the annual rate of ventricular tachycardia or death [25•]. Another study of 31 patients with suspected sarcoidosis found that the majority of cardiac events occurred in individuals with abnormal FDG uptake [28].
Finally, cardiac PET is currently the preferred modality for following response to therapy in patients with known CS as myocardial FDG uptake can be quantified and serially followed. Cardiac PET, unlike CMR in most cases, can also be performed in patients with CS who have undergone ICD or pacemaker implantation. While a reduction in FDG uptake has been shown to be associated with an improvement in left ventricular ejection fraction, further data are needed regarding how to most optimally incorporate data provided by FDG PET in making patient management decisions [29]. Furthermore, more data are needed regarding the impact of immunosuppressive therapies on patient outcomes.
Cardiac amyloidosis
CA is an infiltrative disease characterized by extracellular deposition of an amorphous protein called amyloid. The most common amyloid subtypes affecting the heart are light chain amyloid (AL) and transthyretin amyloid (ATTR). Deposition of amyloid in the cardiac interstitium, irrespective of the type, can lead to diastolic dysfunction and congestive heart failure. CA of the AL subtype portends a poorer prognosis than ATTR, with a median untreated survival of approximately 6 months compared to several years in ATTR amyloidosis, probably owing to light chain myocardial toxicity observed in AL amyloidosis [30]. Although subtle differences in presentation of the two types have been described, in most cases, clinicians rely on advanced imaging or sophisticated laboratory techniques to accurately determine the amyloid subtype. The increase in cases of CA is likely reflective of advances in diagnostic modalities outlined below rather than a true increase in incidence [31].
Echocardiography
Echocardiography is the most widely used and is the initial modality of choice for the assessment of suspected CA [32••]. CA should be suspected in patients with increased left ventricular wall thickness and low voltage on the electrocardiogram. A high degree of clinical suspicion should exist in patients with increased left ventricular wall thickness on echocardiography in the absence of risk factors such as hypertension or aortic stenosis or when the degree of increased wall thickness is disproportionate to the degree of the patient’s known medical conditions.
The classic echocardiographic presentation of CA is increased left ventricular wall thickness biatrial enlargement, and a restrictive left ventricular diastolic filling pattern. Increased right ventricular wall thickness can be an important clue to differentiate CA from hypertrophic cardiomyopathy. Left ventricular wall thickness is usually higher in ATTR compared to AL, perhaps related to the indolent nature of amyloid deposition in the former [32••]. The speckled appearance of the myocardium that has been previously described is now less commonly encountered, owing to harmonic imaging used in current machines [33].
Assessment of myocardial deformation has evolved from tissue Doppler-based strain to user-friendly and reproducible speckle tracking echocardiography (STE) [32••, 34]. This is perhaps the most important addition to amyloid echocardiography in recent years. Though strain is reduced in several cardiomyopathies, the distribution of regional variations can be quite specific [35]. A characteristic “bull’s eye” pattern of the longitudinal strain (LS) map is observed in CA due to relative sparing of apical strain, compared to major decrements in basal strain. Quantification of this regional strain sparing has been attempted with the relative regional strain ratio (RRSR), calculated as average apical LS/sum of average basal and mid LS [35]. A recent study evaluated RRSR in 59 AL and 39 ATTR CA patients and described the adverse prognostic impact of increased RRSR (HR 2.33, 95% CI 1.16–4.69) on the combined outcome of death and cardiac transplant [36•]. Another novel marker called myocardial contraction fraction (MCF) is derived from measures routinely obtained during echocardiography (MCF = stroke volume/myocardial volume), does not require specialized software, and has been shown to have prognostic significance, performing better than ejection fraction [37].
Atrial function in CA is severely reduced, as evidenced by reductions in transmitral A-waves and atrial LS. A recent study assessed LS in all four chambers and reported that right atrial LS was significantly lower in CA than those with non-obstructive hypertrophic cardiomyopathy and strain abnormalities in all chambers were predictive of mortality [38]. The presence of these features warrants consideration for anticoagulation, even in sinus rhythm.
Cardiac magnetic resonance imaging
CMR with gadolinium has excellent sensitivity and specificity to diagnose CA and can help differentiate amyloidosis from other cardiomyopathies. Classically, a pattern of global subendocardial LGE was thought to be pathognomonic of CA. However, in the largest CMR study in CA which included 119 patients with AL CA, 122 with wild-type TTR (TTRwt), and nine asymptomatic TTR mutation carriers (TTRm), the authors describe a continuum of amyloid deposition ranging from no LGE to subendocardial LGE and transmural LGE in advanced disease [39•]. They also highlighted the use of phase sensitive inversion recovery sequence (PSIR), a more reproducible technique that is less operator-independent, to overcome the problem of accurately nulling signal from the myocardium in CA [39•]. Subtype-specific differences were also illustrated, with subendocardial LGE being more prevalent in AL and transmural LGE in ATTR [39•]. This seminal work also pointed out the prognostic significance of transmural LGE, which was an independent predictor on multivariate analysis and was valid for both subtypes of CA (HR 5.4; 95% CI 2.1–13.7) [39•]. This was also validated in a meta-analysis of seven studies with 425 patients that showed that LGE-positive patients had increased overall mortality compared with those without LGE (pooled odds ratio: 4.96; 95% confidence interval: 1.90 to 12.93; P = 0.001) [40].
One study evaluated the extent of atrial LGE in CA and reported that a left atrial LGE extent of >33% had a 94% specificity for the diagnosis of CA and marked reductions in left atrial contractile emptying function [41]. In another study, a left atrial emptying fraction of <16% was an independent predictor of mortality in AL CA patients [42].
T1 signal from the myocardium can be quantified, pre- and post-contrast, and represented in color-coded maps. The ratio of change of T1 in myocardium and blood after gadolinium administration can be used to calculate the extracellular volume (ECV) fraction. ECV can provide an objective assessment of the burden of amyloid, and this is an advantage over LGE as LGE is more difficult to quantify and is more prone to artifacts. While ECV correlates directly with increasing LGE, a quantitative assessment of ECV may offer other advantages. For instance, while further validation is required, ECV may help differentiate CA from other cardiomyopathies, as well as serve as a prognostic marker [39,44,•, 43–45]. These techniques can detect CA early in the disease course, even prior to development of LGE [39•].
In summary, CMR can provide a robust initial evaluation for patients with suspected CA or heart failure of unknown origin after history and physical, ECG, and transthoracic echocardiography have been obtained. It can accurately distinguish CA from other cardiomyopathies and can provide a detailed assessment of cardiac morphology and function. It can detect CA early in the disease course and can potentially aid in identifying the subtype of CA. ECV and T1 signal may also be able to serve as objective imaging endpoints in assessing response to treatment in the future.
Single-photon emission computed tomography with Tc-99 m pyrophosphate
Single-photon emission computed tomography (SPECT) has had a tremendous impact on diagnosing CA. It is the only currently available non-invasive modality to definitively differentiate AL from ATTR, with intense uptake in both ATTRwt and ATTRm, compared to none/minimal uptake in AL CA [46]. Tc-99 m pyrophosphate (PYP) is the tracer used in North America, and a recent consensus statement describes its diagnostic utility, reporting both a positive predictive value and specificity of 100% for detecting ATTR (in the absence of MGUS), obviating the need for an endomyocardial biopsy [47••]. The FDA has also accepted this recommendation as inclusion criteria in clinical trials of much needed novel therapies for TTR CA. A similar tracer, Tc-99 m-3,3-diphosphono-1,2-propanodicarboxylic acid (DPD) is widely used in Europe [48]. Asymptomatic carriers of TTR mutations also exhibit avidity to Tc-99 m PYP, entertaining the possibility that it can be used as a screening test for early diagnosis prior to onset of heart failure symptoms [49]. It may also be possible to risk stratify patients with quantitative estimates from Tc-99 m PYP or DPD scanning. A multicenter retrospective study reported a significantly worse survival in ATTR CA patients with a heart to contralateral ratio of 1.6 or greater on Tc-99 m PYP scan [50•].
Cardiac positron emission tomography
PET tracers that were initially developed to image amyloid in the brain for Alzheimer’s dementia have serendipitously found to also be useful for evaluating CA [51]. The most widely researched tracer has been 11C-Pittsburgh Compound B (11C-PiB), first used in imaging CA in 2011 with avid uptake in all 10 CA patients and none in healthy controls [52]. A subsequent study observed uptake in 13/15 biopsy proven CA patients [53]. Compared to Tc-99 m PYP SPECT, PET has the advantage of absolute quantification of uptake, thereby having the potential to accurately assess burden of disease and any response to therapy. Moreover, one study reported that activity of Tc-99 m PYP SPECT remains constant over 1.5 years, despite disease progression [54]. However, whether 11C-PiB can be used to follow response to therapy remains to be validated, as one study described lower uptake of 11C-PiB in treated versus chemotherapy naive patients, but another did not [52,53,54].
18F florbetapir is an FDA-approved tracer for amyloid neuroimaging but has been shown to demonstrate excellent uptake in both types of CA as well [55]. The myocardial retention index was reported to be higher in AL versus TTR, although the difference did not reach statistical significance (p = 0.057) in this small pilot study [55]. A recent study using 18F florbetaben, a tracer similar to 18F florbetapir, reported a myocardial 18F florbetaben retention of >40%, accurately distinguished CA patients from hypertensive controls [56]. In addition, the authors described a strong relationship between 18F florbetaben uptake and myocardial dysfunction, as assessed by strain. These tracers, which produce strong uptake in both types of CA, may serve as the initial screening test for suspected CA, especially in patients who cannot undergo CMR.
In one pilot study, the use of 18F-NaF PET/CT was evaluated to differentiate AL from ATTR CA and reported positive myocardial uptake in a patient with Val122Ile TTR mutation and no uptake in the AL patient [57]. Subsequently, one study evaluated a patient with wild-type TTR and another with Ile68Leu TTR mutation and found no myocardial uptake in either [58]. The use of 18F-NaF PET/CT warrants further investigation in CA.
Metaiodobenzylguanidine nuclear medicine scan
Metaiodobenzylguanidine (I-123 MIBG) can be used to image cardiac sympathetic innervation and may be of more clinical significance in the future. Cardiac dysautonomia is a common feature of certain neuropathy-predominant TTR mutations (Val30Met) and I-123 MIBG uptake may be decreased in these patients. This finding can occur before echocardiographic signs of cardiac involvement [59]. One study reported its prognostic significance in a group of Val30Met mutant TTR patients: a delayed heart to mediastinum MIBG uptake ratio of <1.6 was an independent predictor of mortality [60]. Currently, I-123 MIBG scanning is approved in the US only for assessing cardiac sympathetic innervation in patients with NYHA class II or III heart failure with a left ventricular ejection fraction of <35%.
Conclusion
Advances in non-invasive cardiovascular imaging have resulted in more sophisticated and accurate ways of diagnosing patients with infiltrative heart disease, as well as track their progression over time with or without treatment. Ongoing and future advancements in the field will allow for even more accurate assessment while ideally obviating the need for more invasive testing. Future clinical criteria for the diagnosis of infiltrative heart disease should include suggestive findings on non-invasive cardiovascular imaging, particularly as these findings are often outperforming current clinical criteria.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Seward JB, Casaclang-Verzosa G. Infiltrative cardiovascular diseases: cardiomyopathies that look alike. J Am Coll Cardiol. 2010;55(17):1769–79. doi:10.1016/j.jacc.2009.12.040.
Iannuzzi MC, Fontana JR. Sarcoidosis: clinical presentation, immunopathogenesis, and therapeutics. JAMA. 2011;305(4):391–9. doi:10.1001/jama.2011.10.
Rybicki BA, Major M, Popovich J, Maliarik MJ, Iannuzzi MC. Racial differences in sarcoidosis incidence: a 5-year study in a health maintenance organization. Am J Epidemiol. 1997;145(3):234–41.
•• Blankstein R, Waller AH. Evaluation of known or suspected cardiac sarcoidosis. Circ Cardiovasc Imaging. 2016;9(3):e000867. doi:10.1161/CIRCIMAGING.113.000867. Comprehensive review of the use of multi-modality imaging in cardiac sarcoidosis.
Silverman KJ, Hutchins GM, Bulkley BH. Cardiac sarcoid: a clinicopathologic study of 84 unselected patients with systemic sarcoidosis. Circulation. 1978;58(6):1204–11.
Cooper LT, Baughman KL, Feldman AM, Frustaci A, Jessup M, Kuhl U, et al. The role of endomyocardial biopsy in the management of cardiovascular disease: a scientific statement from the American Heart Association, the American College Of Cardiology, and the European Society Of Cardiology Endorsed by the Heart Failure Society of America and the Heart Failure Association of the European Society Of Cardiology. Eur Heart J. 2007;28(24):3076–93. doi:10.1093/eurheartj/ehm456.
Yazaki Y, Isobe M, Hiroe M, Morimoto S, Hiramitsu S, Nakano T, et al. Prognostic determinants of long-term survival in Japanese patients with cardiac sarcoidosis treated with prednisone. Am J Cardiol. 2001;88(9):1006–10.
Grutters JC, van den Bosch JM. Corticosteroid treatment in sarcoidosis. Eur Respir J. 2006;28(3):627–36. doi:10.1183/09031936.06.00105805.
Paz HL, McCormick DJ, Kutalek SP, Patchefsky A. The automated implantable cardiac defibrillator. Prophylaxis in cardiac sarcoidosis. Chest. 1994;106(5):1603–7.
•• Birnie DH, Sauer WH, Bogun F, Cooper JM, Culver DA, Duvernoy CS, et al. HRS expert consensus statement on the diagnosis and management of arrhythmias associated with cardiac sarcoidosis. Heart Rhythm. 2014;11(7):1305–23. doi:10.1016/j.hrthm.2014.03.043. Heart Rhythm Society expert consensus statement on cardiac sarcoidosis.
Hiraga H, Iwai K, Hiroe M, Omori F, Sekiguchi M, Tachibana T. Guideline for diagnosis of cardiac sarcoidosis: study report on diffuse pulmonary diseases from the Japanese Ministry Of Health And Welfare. Tokyo: Japanese Ministry of Health and Welfare; 1993. p. 23–4.
Hiraga H, Yuwai K, Hiroe M. Diagnostic standard and guidelines for sarcoidosis. Jpn J Sarcoidosis Granulomatous Disord. 2007;89–102.
Hulten E, Aslam S, Osborne M, Abbasi S, Bittencourt MS, Blankstein R. Cardiac sarcoidosis-state of the art review. Cardiovasc Diagn Ther. 2016;6(1):50–63. doi:10.3978/j.issn.2223-3652.2015.12.13.
Okada DR, Bravo PE, Vita T, Agarwal V, Osborne MT, Taqueti VR, et al. Isolated cardiac sarcoidosis: a focused review of an under-recognized entity. J Nucl Cardiol. 2016. doi:10.1007/s12350-016-0658-1.
Lewin RF, Mor R, Spitzer S, Arditti A, Hellman C, Agmon J. Echocardiographic evaluation of patients with systemic sarcoidosis. Am Heart J. 1985;110(1 Pt 1):116–22.
Burstow DJ, Tajik AJ, Bailey KR, DeRemee RA, Taliercio CP. Two-dimensional echocardiographic findings in systemic sarcoidosis. Am J Cardiol. 1989;63(7):478–82.
Fahy GJ, Marwick T, McCreery CJ, Quigley PJ, Maurer BJ. Doppler echocardiographic detection of left ventricular diastolic dysfunction in patients with pulmonary sarcoidosis. Chest. 1996;109(1):62–6.
Patel AR, Klein MR, Chandra S, Spencer KT, Decara JM, Lang RM, et al. Myocardial damage in patients with sarcoidosis and preserved left ventricular systolic function: an observational study. Eur J Heart Fail. 2011;13(11):1231–7. doi:10.1093/eurjhf/hfr099.
Mehta D, Lubitz SA, Frankel Z, Wisnivesky JP, Einstein AJ, Goldman M, et al. Cardiac involvement in patients with sarcoidosis: diagnostic and prognostic value of outpatient testing. Chest. 2008;133(6):1426–35. doi:10.1378/chest.07-2784.
Joyce E, Ninaber MK, Katsanos S, Debonnaire P, Kamperidis V, Bax JJ, et al. Subclinical left ventricular dysfunction by echocardiographic speckle-tracking strain analysis relates to outcome in sarcoidosis. Eur J Heart Fail. 2015;17(1):51–62. doi:10.1002/ejhf.205.
Lo A, Foder K, Martin P, Younger JF. Response to steroid therapy in cardiac sarcoidosis: insights from myocardial strain. Eur Heart J Cardiovasc Imaging. 2012;13(2):E3. doi:10.1093/ejechocard/jer184.
Smedema JP, Snoep G, van Kroonenburgh MP, van Geuns RJ, Dassen WR, Gorgels AP, et al. Evaluation of the accuracy of gadolinium-enhanced cardiovascular magnetic resonance in the diagnosis of cardiac sarcoidosis. J Am Coll Cardiol. 2005;45(10):1683–90. doi:10.1016/j.jacc.2005.01.047.
• Hulten E, Agarwal V, Cahill M, Cole G, Vita T, Parrish S, et al. Presence of late gadolinium enhancement by cardiac magnetic resonance among patients with suspected cardiac sarcoidosis is associated with adverse cardiovascular prognosis: a systematic review and meta-analysis. Circ Cardiovasc Imaging. 2016;9(9):e005001. doi:10.1161/CIRCIMAGING.116.005001. Meta analysis which describes the prognostic importance of LGE on CMR among patients with suspected cardiac sarcoidosis.
Crouser ED, Ono C, Tran T, He X, Raman SV. Improved detection of cardiac sarcoidosis using magnetic resonance with myocardial T2 mapping. Am J Respir Crit Care Med. 2014;189(1):109–12. doi:10.1164/rccm.201309-1668LE.
• Blankstein R, Osborne M, Naya M, Waller A, Kim CK, Murthy VL, et al. Cardiac positron emission tomography enhances prognostic assessments of patients with suspected cardiac sarcoidosis. J Am Coll Cardiol. 2014;63(4):329–36. doi:10.1016/j.jacc.2013.09.022. Describes the prognostic importance of cardiac PET findings among patients with suspected cardiac sarcoidosis.
Osborne MT, Hulten EA, Murthy VL, Skali H, Taqueti VR, Dorbala S, et al. Patient preparation for cardiac fluorine-18 fluorodeoxyglucose positron emission tomography imaging of inflammation. J Nucl Cardiol. 2016. doi:10.1007/s12350-016-0502-7.
Youssef G, Leung E, Mylonas I, Nery P, Williams K, Wisenberg G, et al. The use of 18F-FDG PET in the diagnosis of cardiac sarcoidosis: a systematic review and metaanalysis including the Ontario experience. J Nucl Med. 2012;53(2):241–8. doi:10.2967/jnumed.111.090662.
Ahmadian A, Brogan A, Berman J, Sverdlov AL, Mercier G, Mazzini M, et al. Quantitative interpretation of FDG PET/CT with myocardial perfusion imaging increases diagnostic information in the evaluation of cardiac sarcoidosis. J Nucl Cardiol. 2014;21(5):925–39. doi:10.1007/s12350-014-9901-9.
Osborne MT, Hulten EA, Singh A, Waller AH, Bittencourt MS, Stewart GC, et al. Reduction in 18F-fluorodeoxyglucose uptake on serial cardiac positron emission tomography is associated with improved left ventricular ejection fraction in patients with cardiac sarcoidosis. J Nucl Cardiol. 2014;21(1):166–74. doi:10.1007/s12350-013-9828-6.
Falk RH, Alexander KM, Liao R, Dorbala S. AL (light-chain) cardiac amyloidosis: a review of diagnosis and therapy. J Am Coll Cardiol. 2016;68(12):1323–41. doi:10.1016/j.jacc.2016.06.053.
Gonzalez-Lopez E, Gallego-Delgado M, Guzzo-Merello G, de Haro-Del Moral FJ, Cobo-Marcos M, Robles C, et al. Wild-type transthyretin amyloidosis as a cause of heart failure with preserved ejection fraction. Eur Heart J. 2015;36(38):2585–94. doi:10.1093/eurheartj/ehv338.
•• Falk RH, Quarta CC, Dorbala S. How to image cardiac amyloidosis. Circ Cardiovasc Imaging. 2014;7(3):552–62. doi:10.1161/CIRCIMAGING.113.001396. Review on how to image cardiac amyloidosis.
White JA, Fine NM. Recent advances in cardiovascular imaging relevant to the management of patients with suspected cardiac amyloidosis. Curr Cardiol Rep. 2016;18(8):77. doi:10.1007/s11886-016-0752-7.
Costa SP, Beaver TA, Rollor JL, Vanichakarn P, Magnus PC, Palac RT. Quantification of the variability associated with repeat measurements of left ventricular two-dimensional global longitudinal strain in a real-world setting. J Am Soc Echocardiogr. 2014;27(1):50–4. doi:10.1016/j.echo.2013.08.021.
Phelan D, Collier P, Thavendiranathan P, Popovic ZB, Hanna M, Plana JC, et al. Relative apical sparing of longitudinal strain using two-dimensional speckle-tracking echocardiography is both sensitive and specific for the diagnosis of cardiac amyloidosis. Heart. 2012;98(19):1442–8. doi:10.1136/heartjnl-2012-302353.
• Senapati A, Sperry BW, Grodin JL, Kusunose K, Thavendiranathan P, Jaber W, et al. Prognostic implication of relative regional strain ratio in cardiac amyloidosis. Heart. 2016;102(10):748–54. doi:10.1136/heartjnl-2015-308657. Describes the prognostic importance of relative regional strain ratio in cardiac amyloidosis.
Tendler A, Helmke S, Teruya S, Alvarez J, Maurer MS. The myocardial contraction fraction is superior to ejection fraction in predicting survival in patients with AL cardiac amyloidosis. Amyloid. 2015;22(1):61–6. doi:10.3109/13506129.2014.994202.
Kado Y, Obokata M, Nagata Y, Ishizu T, Addetia K, Aonuma K, et al. Cumulative burden of myocardial dysfunction in cardiac amyloidosis assessed using four-chamber cardiac strain. J Am Soc Echocardiogr. 2016. doi:10.1016/j.echo.2016.07.017.
• Fontana M, Pica S, Reant P, Abdel-Gadir A, Treibel TA, Banypersad SM, et al. Prognostic value of late gadolinium enhancement cardiovascular magnetic resonance in cardiac amyloidosis. Circulation. 2015;132(16):1570–9. doi:10.1161/CIRCULATIONAHA.115.016567. Describes the prognostic value of LGE on CMR in patients with systemic amyloidosis.
Raina S, Lensing SY, Nairooz RS, Pothineni NV, Hakeem A, Bhatti S, et al. Prognostic value of late gadolinium enhancement CMR in systemic amyloidosis. JACC Cardiovasc Imaging. 2016. doi:10.1016/j.jcmg.2016.01.036.
Kwong RY, Heydari B, Abbasi S, Steel K, Al-Mallah M, Wu H, et al. Characterization of cardiac amyloidosis by atrial late gadolinium enhancement using contrast-enhanced cardiac magnetic resonance imaging and correlation with left atrial conduit and contractile function. Am J Cardiol. 2015;116(4):622–9. doi:10.1016/j.amjcard.2015.05.021.
Mohty D, Boulogne C, Magne J, Varroud-Vial N, Martin S, Ettaif H, et al. Prognostic value of left atrial function in systemic light-chain amyloidosis: a cardiac magnetic resonance study. Eur Heart J Cardiovasc Imaging. 2016;17(9):961–9. doi:10.1093/ehjci/jew100.
Fontana M, Banypersad SM, Treibel TA, Abdel-Gadir A, Maestrini V, Lane T, et al. Differential myocyte responses in patients with cardiac transthyretin amyloidosis and light-chain amyloidosis: a cardiac MR imaging study. Radiology. 2015;277(2):388–97. doi:10.1148/radiol.2015141744.
Banypersad SM, Fontana M, Maestrini V, Sado DM, Captur G, Petrie A, et al. T1 mapping and survival in systemic light-chain amyloidosis. Eur Heart J. 2015;36(4):244–51. doi:10.1093/eurheartj/ehu444.
Mongeon FP, Jerosch-Herold M, Coelho-Filho OR, Blankstein R, Falk RH, Kwong RY. Quantification of extracellular matrix expansion by CMR in infiltrative heart disease. JACC Cardiovasc Imaging. 2012;5(9):897–907. doi:10.1016/j.jcmg.2012.04.006.
Bokhari S, Castano A, Pozniakoff T, Deslisle S, Latif F, Maurer MS. (99m)Tc-pyrophosphate scintigraphy for differentiating light-chain cardiac amyloidosis from the transthyretin-related familial and senile cardiac amyloidoses. Circ Cardiovasc Imaging. 2013;6(2):195–201. doi:10.1161/CIRCIMAGING.112.000132.
•• Gillmore JD, Maurer MS, Falk RH, Merlini G, Damy T, Dispenzieri A, et al. Nonbiopsy diagnosis of cardiac transthyretin amyloidosis. Circulation. 2016;133(24):2404–12. doi:10.1161/CIRCULATIONAHA.116.021612. Review on non-biopsy-dependent diagnosis of TTR cardiac amyloidosis.
Rapezzi C, Quarta CC, Guidalotti PL, Pettinato C, Fanti S, Leone O, et al. Role of (99m)Tc-DPD scintigraphy in diagnosis and prognosis of hereditary transthyretin-related cardiac amyloidosis. JACC Cardiovasc Imaging. 2011;4(6):659–70. doi:10.1016/j.jcmg.2011.03.016.
Haq M, Pawar S, Berk JL, Miller EJ, Ruberg FL. Can 99m-Tc-pyrophosphate aid in early detection of cardiac involvement in asymptomatic variant TTR amyloidosis? JACC Cardiovasc Imaging. 2016. doi:10.1016/j.jcmg.2016.06.003.
• Castano A, Haq M, Narotsky DL, Goldsmith J, Weinberg RL, Morgenstern R, et al. Multicenter study of planar technetium 99m pyrophosphate cardiac imaging: predicting survival for patients with ATTR cardiac amyloidosis. JAMA Cardiol. 2016. doi:10.1001/jamacardio.2016.2839. Describes the prognostic value of Tc-99m- Pyrophosphate scanning.
Chen W, Dilsizian V. Molecular imaging of amyloidosis: will the heart be the next target after the brain? Curr Cardiol Rep. 2012;14(2):226–33. doi:10.1007/s11886-011-0239-5.
Antoni G, Lubberink M, Estrada S, Axelsson J, Carlson K, Lindsjo L, et al. In vivo visualization of amyloid deposits in the heart with 11C-PIB and PET. J Nucl Med. 2013;54(2):213–20. doi:10.2967/jnumed.111.102053.
Lee SP, Lee ES, Choi H, Im HJ, Koh Y, Lee MH, et al. 11C-Pittsburgh B PET imaging in cardiac amyloidosis. JACC Cardiovasc Imaging. 2015;8(1):50–9. doi:10.1016/j.jcmg.2014.09.018.
Castano A, DeLuca A, Weinberg R, Pozniakoff T, Blaner WS, Pirmohamed A, et al. Serial scanning with technetium pyrophosphate (99mTc-PYP) in advanced ATTR cardiac amyloidosis. J Nucl Cardiol. 2015. doi:10.1007/s12350-015-0261-x.
Dorbala S, Vangala D, Semer J, Strader C, Bruyere Jr JR, Di Carli MF, et al. Imaging cardiac amyloidosis: a pilot study using (1)(8)F-florbetapir positron emission tomography. Eur J Nucl Med Mol Imaging. 2014;41(9):1652–62. doi:10.1007/s00259-014-2787-6.
Law WP, Wang WY, Moore PT, Mollee PN, Ng AC. Cardiac amyloid imaging with 18F-florbetaben positron emission tomography: a pilot study. J Nucl Med. 2016. doi:10.2967/jnumed.115.169870.
Van Der Gucht A, Galat A, Rosso J, Guellich A, Garot J, Bodez D, et al. [18F]-NaF PET/CT imaging in cardiac amyloidosis. J Nucl Cardiol. 2016;23(4):846–9. doi:10.1007/s12350-015-0287-0.
Gagliardi C, Tabacchi E, Bonfiglioli R, Diodato S, Nanni C, Guidalotti P, et al. Does the etiology of cardiac amyloidosis determine the myocardial uptake of [18F]-NaF PET/CT? J Nucl Cardiol. 2016. doi:10.1007/s12350-016-0457-8.
Noordzij W, Glaudemans AW, van Rheenen RW, Hazenberg BP, Tio RA, Dierckx RA, et al. (123)I-Labelled metaiodobenzylguanidine for the evaluation of cardiac sympathetic denervation in early stage amyloidosis. Eur J Nucl Med Mol Imaging. 2012;39(10):1609–17. doi:10.1007/s00259-012-2187-8.
Coutinho MC, Cortez-Dias N, Cantinho G, Conceicao I, Oliveira A, Bordalo e Sa A, et al. Reduced myocardial 123-iodine metaiodobenzylguanidine uptake: a prognostic marker in familial amyloid polyneuropathy. Circ Cardiovasc Imaging. 2013;6(5):627–36. doi:10.1161/CIRCIMAGING.112.000367.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Sanjay Divakaran, Bradley Collins, Tomas Vita, Marcelo F. Di Carli, and Ron Blankstein each declare no potential conflicts of interest.
Avinainder Singh is supported by the Janet and Stanley Cohen Cardiac Amyloidosis Fellowship.
Rodney H. Falk was supported by the Friends of Burt Glazov Cardiac Amyloidosis Fund and the Demarest Lloyd Jr. Foundation. Dr. Falk receives funds for consulting from Ionis Pharmaceuticals and Alnylam Pharmaceuticals and research support from GlaxoSmithKline.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Imaging
Rights and permissions
About this article
Cite this article
Divakaran, S., Singh, A., Collins, B. et al. Role of Imaging in Evaluating Infiltrative Heart Disease. Curr Treat Options Cardio Med 19, 3 (2017). https://doi.org/10.1007/s11936-017-0500-3
Published:
DOI: https://doi.org/10.1007/s11936-017-0500-3