Abstract
The present paper gives an overview of the methodology and results of the first decade of research into Internet-based interventions for women’s sexual dysfunction. The interventions, retrieved in a literature search, were mostly well grounded on common theoretical models of sexual dysfunction and psychological disorders, and most ingredients of the interventions were theory-informed. Most interventions offered Web-based therapeutic content within a more or less preprogrammed structure. Most of these also offered prescheduled and/or participant-initiated contact with a sexual health care professional. Comparative effect studies showed improvements in sexual functioning as well as relational functioning at the point of termination of the intervention period. Improvements at posttreatment were generally maintained for several months after termination of the active intervention period. The results of this review seem to warrant further development of Internet-based interventions for women’s sexual dysfunctions.
Similar content being viewed by others
Introduction
The use of the Internet as a service delivery mode in the care for women and men with sexual dysfunctions has a relatively brief history. Internet-based psychotherapeutic interventions for common mental disorders, including anxiety and depressive disorders, have proliferated in recent years [1–3, 4•, 5•]. To a lesser extent, such interventions have also become available in the treatment of sexual dysfunctions. Probably, the first scientific publication was authored by Hall [6] who described the treatment of eight women and men with various sexual difficulties through online task-based psychosexual therapy. The author concluded that the initial outcomes were positive. Since that first publication, several have followed, describing outcome studies of Internet-based interventions for sexual dysfunctions using various research designs. The slow start was notwithstanding the notion that the translation of professionally administered sex therapy to Internet-based delivery modes might have been more easily achieved than for many other common mental health problems [7], given that sex therapy has contained self-help elements ever since its emergence in the 1970s [8], and because the core ingredients of therapeutic change in sex therapy (the sensate focus exercises) were in most cases already performed in the privacy of the couples’ homes [9].
Online help has advantages over face-to-face contact [10]. For some individuals, the anonymity that is sometimes provided during (the initial phase of) online therapy can make it a preferable option compared with face-to-face types of help. The increased accessibility of online help, including the independence of geographic location and, in some modes of delivery, also the asynchronous nature of the contact between client and therapist, may provide a valuable service for those who have difficulties to attend face-to-face meetings due to physical or geographic constraints, or for work-related reasons. Moreover, because treatment is administered in daily-life conditions, generalization of treatment gains to the real-life environment may be less problematic. Finally, improvements in sexual functioning following online interventions might be more attributed to one’s own efforts and competence, and thus boost one’s self-esteem. However, disadvantages and risks are also recognized. One risk factor that Andersson and Titov [10] identified is the currently limited knowledge about who might benefit and who is likely to fail using online help. Treatment outcome predictors that were studied were not very robust. A related topic is that negative outcomes may go undetected, thus leaving sufferers in quandaries.
Reviews and meta-analytic compilations of controlled and randomized outcome studies on thousands of clients have provided abundant evidence for the efficacy and effectiveness of Internet-based care for individuals suffering from anxiety and depressive disorders [11, 12] as well as for health promotion [13••]. Increasingly, evidence is also found for the cost-effectiveness of this approach [11, 14–18]. Thus far, no reviews of the outcome of Internet-based interventions for women’s sexual dysfunctions have been published.
The characteristics of Internet-based interventions can be conceptualized along three main lines [13••]: (a) the theoretical foundation of the intervention and the use of theory-based predictors; (b) the specific strategies and behavior change techniques used in the intervention; and (c) the mode of delivery. In the present paper, the published empirical research of Internet-based therapy for women’s sexual dysfunctions between its introduction and March, 2016 will be reviewed using this conceptual framework.
Theoretical Background of Internet-Based Interventions
Internet-based interventions can be characterized according to the extent to which they are founded on established theory. Although it is thus far unknown whether the effectiveness of Internet-based interventions is significantly impacted by reliance on established theory [19, 20], it is plausible that theoretical considerations may be beneficial when they are used to guide the selection of disorder aspects that need to be targeted (e.g., learning mechanisms, automatic vs deliberate disorder-relevant cognitions, self-efficacy, self-esteem, partner communication patterns), of techniques to address mechanisms underlying particular problem types (e.g., skills deficits), or the selection of target groups of patients that are most likely to benefit from participation (e.g., with specific clinical diagnoses) [13, 20, 21•]. Clear definition and identification procedures of the target group for which an intervention might be beneficial might prevent incorrect self-diagnosis that could lead one to choose an unhelpful strategy [21•].
Specific Strategies and Behavior Change Techniques Used in Internet-Based Interventions
Internet-based interventions for sexual dysfunctions employ specific strategies and behavior change techniques to promote therapeutic change. Such strategies and techniques are mostly typical for the underlying theoretical model that guided intervention development (e.g., cognitive restructuring techniques based on cognitive models of sexual dysfunction, see [22–25]) or masturbation training for primary orgasmic problems in women [26].
Modes of Delivery of Internet-Based Interventions
Internet-based interventions may be fully self-directed and work as a self-help approach, comparable to unassisted bibliotherapy [27, 28], with a structured therapy program encapsulated in a computer algorithm. Others are augmented with varying levels of therapeutic assistance. Furthermore, variations in the use of Internet technology for therapeutic assistance are found: video conferencing utilities are used, as well as text-based technology, both through Internet (e-mail, Whatsapp, snapchat) and telephone, including SMS. Client-therapist contact may be synchronous, such as in video conferencing, or asynchronous, including exchange of both text and video recordings. Internet-based interventions may be implemented as stand-alone interventions or may be blended with other, face-to-face interventions. Additional techniques can involve the use of mobile phone-based data collection (“ecological momentary assessment” [29, 30]) and conditional feedback on mobile monitoring data in both standardized and tailored formats. A coding matrix for assessing mode of delivery in Internet-based interventions developed by Webb and colleagues [13••] will be used to guide the discussion of included interventions.
Method
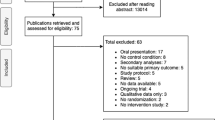
In March 2016, a search was conducted using Web of Science, PubMed, and Psychinfo. Search terms in the publication title, combined using Boolean operators, were as follows: (sexual dysfunction* OR sexual disorder* OR sexual difficult* OR sexual problem* OR sexual complaint*) AND (women* OR female OR woman*) AND (Internet OR online OR www OR world wide web) AND (treatment OR therap* OR intervention OR controlled trial OR RCT). This search yielded 16 publications. The reference lists of the retrieved papers were searched for publications meeting the inclusion criteria. One more paper was identified. After reading the abstracts, eight publications were retained for the review. Inclusion criteria were as follows: the study addressed female sexual dysfunctions; the major part of the intervention was delivered via the Internet; participants were allocated using a randomization technique to an active intervention group or to a comparison group receiving a control intervention or no intervention; and a measure of sexual functioning or sexual dysfunction after termination of the intervention was performed. The included publications were searched for details on the treated population, study characteristics, intervention characteristics, assessment instruments used, and treatment effects.
Results
Eight publications were included [31–36, 37••, 38]. Seven of these reported on four completed RCTs; one paper reported the design of an RCT of which the data collection was still ongoing [34]. Two studies, reported in five publications [31–33, 35, 36], included women from the general population with mixed sexual difficulties, related to sexual desire, arousal, orgasm, or sexual pain and who were living in a stable heterosexual relationship. One study included women with either localized breast or gynecological cancer [37••] and who scored as sexually dysfunctional (under 26.5) on the Female Sexual Function Index [39]. One paper collected qualitative data from gynecologic cancer patients who were randomized to the immediate start of a Web-based support group or a waitlist control group [38]. Other characteristics of the included studies are summarized in Table 1. Characteristics of the study interventions are summarized in Table 2.
Theoretical Background and Theory-Based Strategies and Behavior Change Techniques Used in Internet-Based Interventions
The theoretical foundations of three of five interventions [31, 34, 35] in the included studies align with the mainstream of current interventions for common mental disorders: cognitive theory and learning theory [40, 41]. Intervention ingredients in these studies were derived from these conceptual frameworks, including challenging negative automatic thoughts, relapse prevention, role playing exercises, exposure techniques, and provision of feedback on performance in homework (see Table 2). Sexual response cycle theory [8, 42] was used as an important theoretical background in four interventions [31, 34, 35, 37••]; the central position in these interventions of progressive sensate focus exercises traces back to this—specifically sexological—theoretical model. One intervention [31] had a significant background in mindfulness theory, which is often integrated with cognitive-behavioral approaches [43, 44]. One RCT using qualitative methods of evaluation [38] was based on the supportive–expressive group therapy model for cancer survivors [45]. Some therapeutic elements were included in several interventions without an explicit rationale provided. Communication skills training or instruction for improved communication with the partner were included in four interventions, without any specific reference to a theoretical background, such as cybernetics or systems theory. Psychoeducation was mentioned in three interventions, and relapse prevention in two interventions.
Modes of Delivery of Internet-Based Interventions
In four interventions [31, 34, 35, 37••], participants could use therapeutic elements that were accessible on a secured Web site. The Web-based part of one intervention [37••] contained information on a wide variation of problem-related topics but did not give specific instructions on how to use this information. Three interventions [31, 34, 35] comprised a series of therapeutic modules, containing psychoeducation about specific problem elements. They also provided instructions for the use of techniques to modify cognitions or behaviors that serve to maintain the sexual problem, such as challenging negative automatic thoughts, or reducing performance demand by performing sensate focus exercises. One intervention [38] did not offer “stand-alone” Web site content but relied fully on the exchange of information among participants in asynchronous text chats (discussion board/forum), moderated by sexual health care professionals.
All interventions, except for the Wiljer et al. [38] intervention, included scheduled meetings with a professional to provide guidance and support for the use of the Web-based content. In addition, two interventions [34, 35] allowed participants unlimited text-based contact with the therapist on the participant’s initiative. All interventions allowed some form of access to a professional for requesting advice. Peer-to-peer interaction was enabled in one study [38] using a group text chat facility.
Effects of Internet-Based Interventions for Women’s Sexual Dysfunctions
The efficacy of three interventions was compared with delayed treatment or waitlist [31, 34, 35]. Of two interventions [31, 35], comparison of posttreatment gains suggested that different aspects of sexual functioning (FSFI: η2part = 0.56; PAIR sexual intimacy: η2part = 0.26) and relational functioning (PAIR: η2part = 0.39; PAIR emotional intimacy: η2part = 0.08; PAIR communication: η2part = 0.08) were improved during the active intervention. In one study [35], no effects of the intervention on anxiety and mood were found, suggesting that this, dedicated, intervention only had effect on the specific, targeted problem areas. Posttreatment gains regarding sexual and relational functioning were generally maintained until follow-up assessment. Of the third intervention [34], no effect data is yet available.
Of the interventions for women with cancer [37••], two different versions were compared, respectively, with and without additional face-to-face counseling sessions. Both versions were found to have beneficial effects on sexual functioning (FSFI: p < 0.001), menopausal complaints (MSIQ: p < 0.001), general psychological well-being (BSI-18: p = 0.001), and quality of life (QLACS: p < 0.001). The blended version was found to have stronger effects on sexual functioning (FSFI: p < 0.001), compared to the unassisted version, but the latter had stronger effects on general psychological well-being (BSI-18: p = 0.01) and quality of life (QLACS: p = 0.008). Posttreatment gains were generally maintained through follow-up measurement at both 3 and 6 months, except for sexual functioning in the unassisted version of the intervention, which deteriorated again at 3-month follow-up (FSFI: p = 0.05).
Conclusions
In a search of the literature for this review of Internet-based interventions for women’s sexual dysfunctions, five interventions were identified, reported in a total of eight publications. The included interventions aimed to offer help to women suffering from a broad range of sexual dysfunctions. Both women who were treated after receiving a diagnosis of breast cancer or gynecological cancer and women in the community without comorbid disease were included in the studies investigating the efficacy of treatment. The interventions were all based on common theoretical models of sexual dysfunction and psychological disorders, or on a theory of group counseling [45], and most ingredients of the interventions were theory-informed. Except for one [38], all interventions offered therapeutic content on a secured Web site that could be utilized within a more or less preprogrammed structure. These same interventions also offered prescheduled and/or participant-initiated contact with a sexual health care professional. Comparisons of the active interventions with a control group showed improvements in sexual functioning as well as relational functioning at the point of termination of the treatment period, whereas the beneficial effects on other domains of (psychological and physical) functioning were equivocal. Improvements at posttreatment were generally maintained for several months after termination of the active intervention period. One intervention [37••] included a face-to-face component, three counseling sessions, whereas all others only employed text exchange, either asynchronous through email [35] or using an online peer-to-peer discussion board [38], or synchronous through real-time text chat [31, 34]. The results of the face-to-face intervention that was blended with a Web-based algorithm were directly compared to the use of the algorithm as a self-help intervention. The direct effects of the blended combination had a stronger effect on sexual functioning at post-treatment and were better maintained after 3-month follow-up than the effects of the self-help intervention. The self-help version, however, had larger effects on general well-being and quality of life that were sustained at 3- and 6-month follow-up. These findings are in line with the outcomes of Internet-based interventions for other mental disorders [4•]. Supplementing Web-based algorithms with some face-to-face support, therefore, seems important for obtaining maximal results, although this issue deserves further investigation. The results of the present review seem to warrant further development of Internet-based interventions for women’s sexual dysfunctions and rigorous investigation of the benefits and risks of this approach. Specifically, investigator’s attention should be directed at identifying predictive factors that help protect potential users of this type of interventions against incorrect self-diagnosis and subsequent failures in finding adequate help for their suffering. These shortcomings suggest that the current potential for dissemination of Internet-based interventions for women’s sexual dysfunctions outside of research settings is still limited. However, this has not withheld service providers, at least in Europe, to offer such interventions on a large scale to the public seeking help for sexual problems. Both in the USA and elsewhere ethical, legal and jurisdictional issues still need to be worked out. The creation of professional guidelines based on solid scientific evidence of the efficacy of interventions, the demarcation of target groups for whom online help is likely to be beneficial, the provision of adequate information to the target populations, and the adherence to such guidelines for reimbursement of treatment by health insurance companies might be helpful in maximizing the efficacy of Internet-based health care and its safe use in the field of sexual dysfunctions.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Emmelkamp PM, David D, Beckers T, et al. Advancing psychotherapy and evidence-based psychological interventions. Int J Meth Psychiatr Res. 2014;23 Suppl 1:58–91.
Lovejoy TI, Demireva PD, Grayson JL, et al. Advancing the practice of online psychotherapy: an application of Rogers’ diffusion of innovations theory. Psychother. 2009;46:112–24.
Månsson KNT, Ruiz ES, Gervind E, et al. Development and initial evaluation of an internet-based support system for face-to-face cognitive behavior therapy: a proof of concept study. J Med Internet Res. 2013;15:220–33.
Palmqvist B, Carlbring P, Andersson G. Internet-delivered treatments with or without therapist input: does the therapist factor have implications for efficacy and cost? Exp Rev Pharmacoecon Outcomes Res. 2007;7:291–7. This study addresses the important issue of the added value of professional guidance beyond the effects of a self-help version on Internet-based treatment.
Andersson G. Internet-delivered psychological treatments. Annu Rev Clin Psychol. 2015; doi:10.1146/annurev-clinpsy-021815-093006. This recent review provides a comprehensive overview of Internet-based interventions for common mental disorders.
Hall P. Online psychosexual therapy: a summary of pilot study findings. Sex Rel Ther. 2004;19:167–78.
van Lankveld J, Mevissen FEF. Bibliotherapy and internet-based programs for sexual problems. In: Wylie KR, editor. ABC of sexual health. 3rd ed. Chichester, UK: John Wiley & Sons; 2015. p. 118–20.
Masters WH, Johnson VE. Human sexual inadequacy. Boston: Little, Brown; 1970.
van Lankveld J. Self-help therapies for sexual dysfunctions. In: Watkins PL, Clum GA, editors. Handbook of self-help therapies. New York: Routledge; 2008. p. 187–213.
Andersson G, Titov N. Advantages and limitations of internet-based interventions for common mental disorders. World Psychiatr. 2014;13:4–11.
Andersson G, Cuijpers P, Carlbring P, et al. Guided internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: a systematic review and meta-analysis. World Psychiatr. 2014;13:288–95.
Arnberg FK, Linton SJ, Hultcrantz M, et al. Internet-delivered psychological treatments for mood and anxiety disorders: a systematic review of their efficacy, safety, and cost-effectiveness. PLoS One. 2014;9, e98118.
Webb TL, Joseph J, Yardley L, et al. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res. 2010;12:e4. This study provides a new theoretical framework for Internet-based interventions.
Hedman E, Ljotsson B, Lindefors N. Cognitive behavior therapy via the Internet: a systematic review of applications, clinical efficacy and cost-effectiveness. Exp Rev Pharmacoecon Outcomes Res. 2012;12:745–64.
Nordgren LB, Hedman E, Etienne J, et al. Effectiveness and cost-effectiveness of individually tailored internet-delivered cognitive behavior therapy for anxiety disorders in a primary care population: a randomized controlled trial. Behav Res Ther. 2014;59:1–11.
Warmerdam L, Smit F, van Straten A, et al. Cost-utility and cost-effectiveness of internet-based treatment for adults with depressive symptoms: randomized trial. J Med Internet Res. 2010;12, e53.
Hedman E, Andersson E, Lindefors N, et al. Cost-effectiveness and long-term effectiveness of internet-based cognitive behaviour therapy for severe health anxiety. Psychol Med. 2013;43:363–74.
Gerhards SA, de Graaf LE, Jacobs LE, et al. Economic evaluation of online computerised cognitive-behavioural therapy without support for depression in primary care: randomised trial. Br J Psychiatr. 2010;196:310–8.
Borrelli B, Ritterband LM. Special issue on ehealth and mhealth: Challenges and future directions for assessment, treatment, and dissemination. Health Psychol. 2015;34(Suppl):1205–8.
Andersson G, Carlbring P, Berger T, et al. What makes internet therapy work? Cogn Behav Ther. 2009;38 Suppl 1:55–60.
Boettcher J, Berger T, Renneberg B. Does a pre-treatment diagnostic interview affect the outcome of internet-based self-help for social anxiety disorder? a randomized controlled trial. Behav Cogn Psychother. 2012;40:513–28. This study highlights the issue of pre-enrollment diagnostic assessment for Internet-based interventions.
Ellis A. Reason and emotion in psychotherapy. Lyle Stuart: Oxford, England; 1962.
Janssen E, Everaerd W, Spiering M, et al. Automatic processes and the appraisal of sexual stimuli: toward an information processing model of sexual arousal. J Sex Res. 2000;37:8–23.
Nobre PJ. Psychological determinants of erectile dysfunction: testing a cognitive-emotional model. J Sex Med. 2010;7:1429–37.
Barlow DH. Causes of sexual dysfunction: the role of anxiety and cognitive interference. J Consult Clin Psychol. 1986;54:140–8.
Barbach LG. For yourself: the fulfillment of female sexuality. New York: Doubleday; 1974.
van Lankveld J. Bibliotherapy in the treatment of sexual dysfunctions: a meta-analysis. J Consult Clin Psychol. 1998;66:702–8.
van Lankveld J. Self-help therapies for sexual dysfunction. Ann Rev Sex Res. 2009;46:143–55.
Hektner JM, Schmidt JA, Csikszentmihalyi M. Experience sampling method: measuring the quality of everyday life. Thousand Oaks: Sage; 2007.
Mehl MR, Conner TS. Handbook of research methods for studying daily life. Guilford: New York/London; 2012.
Hucker A, McCabe MP. An online, mindfulness-based, cognitive-behavioral therapy for female sexual difficulties: impact on relationship functioning. J Sex Mar Ther. 2014;40:561–76.
Hucker A, McCabe MP. A qualitative evaluation of online chat groups for women completing a psychological intervention for female sexual dysfunction. J Sex Mar Ther. 2014;40:58–68.
Hucker A, McCabe MP. Incorporating mindfulness and chat groups into an online cognitive behavioral therapy for mixed female sexual problems. J Sex Res. 2015;52:627–39.
Hummel SB, van Lankveld JJ, Oldenburg HS, et al. Internet-based cognitive behavioral therapy for sexual dysfunctions in women treated for breast cancer: design of a multicenter, randomized controlled trial. BMC Cancer. 2015;15:321.
Jones LM, McCabe MP. The effectiveness of an internet-based psychological treatment program for female sexual dysfunction. J Sex Med. 2011;8:2781–92.
McCabe MP, Jones LM. Attrition from an internet-based treatment program for female sexual dysfunction: who is best treated with this approach? Psychol Health Med. 2013;18:612–8.
Schover LR, Yuan Y, Fellman BM, et al. Efficacy trial of an internet-based intervention for cancer-related female sexual dysfunction. J Nat Compreh Cancer Netw. 2013;11:1389–97. This study directly compares self-help and therapist-assisted versions of the same Internet-based intervention for women’s sexual dysfunctions.
Wiljer D, Urowitz S, Barbera L, et al. A qualitative study of an internet-based support group for women with sexual distress due to gynecologic cancer. J Cancer Educ. 2011;26:451–8.
Wiegel M, Meston C, Rosen R. The Female Sexual Function Index (FSFI): cross-validation and development of clinical cutoff scores. J Sex Mar Ther. 2005;31:1–20.
Mineka S, Zinbarg R. A contemporary learning theory perspective on the etiology of anxiety disorders: it’s not what you thought it was. Am Psychol. 2006;61:10–26.
Clark DA, Beck AT. Cognitive theory and therapy of anxiety and depression: convergence with neurobiological findings. Tr Cogn Sci. 2010;14:418–24.
Masters WH, Johnson VE. Human sexual response. Little, Brown: Oxford, England; 1966.
Brotto LA, Goldmeier D. Mindfulness interventions for treating sexual dysfunctions: the gentle science of finding focus in a multitask world. J Sex Med. 2015;12:1687–9.
Piet J, Hougaard E. The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: a systematic review and meta-analysis. Clin Psychol Rev. 2011;31:1032–40.
Spiegel D, Classen C. Group therapy for cancer patients: a research-based handbook of psychosocial care. New York, NY, US: Basic Books; 2000.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
JVL declares that he has no conflicts of interest.
Human and Animal Rights and Informed Consent
All reported studies in this review have been previously published and were in compliance with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
This article is part of the Topical Collection on Female Sexual Dysfunction and Disorders
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
van Lankveld, J. Internet-Based Interventions for Women’s Sexual Dysfunction. Curr Sex Health Rep 8, 136–143 (2016). https://doi.org/10.1007/s11930-016-0087-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11930-016-0087-9