Abstract
Purpose of Review
The spread of the novel coronavirus SARS-CoV-2 and its associated disease, coronavirus disease of 2019 (COVID-19), has significantly derailed cancer care. Patients with leukemia are more likely to have severe infection and increased rates of mortality. There is paucity of information on how to modify care of leukemia patients in view of the COVID-19 risks and imposed restrictions. We review the available literature on the impact of COVID-19 on different types of leukemia patients and suggest general as well as disease-specific recommendations on care based on available evidence.
Recent Findings
The COVID-19 infection impacts leukemia subtypes in variable ways and the standard treatments for leukemia have similarly, varying effects on the course of COVID-19 infection. Useful treatment strategies include deferring treatment when possible, use of less intensive regimens, outpatient targeted oral agents requiring minimal monitoring, and prioritization of curative or life-prolonging strategies. Reducing health care encounters, rational transfusion standards, just resource allocation, and pre-emptive advance care planning will serve the interests of leukemia patients.
Summary
Ad hoc modifications based on expert opinions and extrapolations of previous well-designed studies are the way forward to navigate the crisis. This should be supplanted with more rigorous prospective evidence.
Similar content being viewed by others
Introduction
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) was first detected in Wuhan, China, in December 2019. It is spread by droplet, contact, and airborne routes. About 20% of patients are asymptomatic [1]. Coronavirus disease of 2019 (COVID-19) is caused by SARS-CoV-2 and is characterized by a syndrome of fever, coryza, dysgeusia, cough, dyspnea, diarrhea, lymphopenia, ground-glass opacities, hypoxemia, and cytokine storm [2]. The spectrum of disease is heterogeneous ranging from mild symptoms akin to a common cold, to an acute respiratory distress syndrome requiring invasive ventilation. COVID-19 has evolved into a worldwide pandemic affecting more than 105 million people, with the USA contributing more than 26 million cases and over 450,000 deaths [3]. In the general population, the infection rates are reported to be <1–2% and the mortality rate approximately 1–5%. High-risk groups with higher probability of death if infected include the older patients with comorbidities such as diabetes, the overweight, African Americans, and the immunocompromised population including those with cancers. For patients with cancer, the case fatality rate is two times that of the general population (5.6% versus 2.3%) [4, 5]. People living with cancers are viewed as high-risk groups due to the immunosuppression relating to their diagnoses and their treatment. In China, 1% of COVID-19 cases had a history of cancer whereas the incidence of cancer in the overall Chinese population is 0.29%. More importantly, patients with cancer are more likely to have adverse outcomes defined by being admitted to intensive care unit for invasive ventilation or death [5]. The case rate of COVID-19 among hospitalized patients with hematological malignancies was 10% compared to <1% for other cancers [6, 7]. These patients also have more severe diseases and a higher fatality rate of up to 37% [8, 9, 10••]. Consensus-based guidance and expert recommendations are being expeditiously developed and updated to help navigate this landscape for patients with all cancers, including those with leukemia [11••, 12•, 13•, 14, 15, 16••, 17]. However, prospective evidence is still very limited. Here, we present a review of the available evidence relevant to the care of leukemia patients in the context of COVID-19.
The markers of severe disease are non-specific and include elevated d-dimer, CRP, LDH, troponin, ferritin, and CPK and lymphopenia. Abnormalities in these parameters can be seen in leukemic patients in different contexts, making interpretation of these values a challenge. Temporal trends should be reviewed and may provide more information regarding the possible etiology. Respiratory support and monitoring for cytokine storm is paramount. Patients with COVID-19 also have an increased risk of thromboses, with one study showing 31% of patients with thrombotic complications in the intensive care unit [18, 19, 20•].
Several drugs have been approved for the treatment of COVID-19 and SARS-CoV-2 infections (Table 1). Vaccines have also been approved in the USA and other countries and are currently being administered to selected populations. Asymptomatic patients can be monitored for recovery in their homes. The commonly employed drugs in the management of severe COVID-19 are summarized as follows.
General Recommendations
From the early stages of the pandemic, missed or delayed diagnosis, delays or deferral in chemotherapy, decreased frequency of follow-up visits and patient assessments, postponement of allogenic hematopoietic stem cell transplantation (allo-SCT), and shortage of blood products became apparent [30]. Shortage of acute care beds in intensive care units and respiratory support devices like ventilators has occurred throughout the country during the recurrent peaks of the crisis. This is compounded by the stress exerted in the healthcare workers who themselves are frequently exposed, requiring quarantine or falling victims of COVID-19. Many new leukemia patients are acutely ill needing supportive care (e.g., transfusions), management of infections, and hospitalization, and some, particularly those with acute leukemias, requiring early initiation of chemotherapy, frequently intensive, to control their disease. Induction chemotherapy and high-dose consolidation chemotherapy cause severe and prolonged neutropenia with an increased risk of bacterial, fungal, and viral infections. Testing for SARS-CoV-2 and CT imaging of the chest in all leukemia patients regardless of symptoms is recommended for all-new diagnosis and before any high-dose chemotherapy [31]. If patients with acute leukemia test positive for SARS-CoV-2, a delay in the start of treatment by 10–14 days should be considered whenever possible, with the possible use of transient cytoreductive agents to control rapid proliferation of the disease and in an attempt to minimize rapid progression (e.g., hydroxyurea, dexamethasone for acute lymphoblastic and other lymphoid leukemias, cytarabine single agent for acute myeloid leukemia). Such delays would not be expected to negatively affect the outcome in most instances. Several analyses have shown that a delay in the start of chemotherapy in acute myeloid leukemia (in these reports for obtaining cytogenetic and molecular analysis) does not adversely affect the outcome in most instances [32, 33]. In some instances, treatment interruption or discontinuation may be considered if the patient develops COVID-19 infection during active treatment. This decision should be weighed against the possible adverse impact this may have on the overall outcome of the patient, particularly for patients receiving potentially curative therapy. Early initiation of cytokine modulators could be considered for patients symptomatic from COVID-19 infection [34]. Specific and clear criteria should be established to guide the timing for the start of chemotherapy; these algorithms should be regularly reviewed and updated according to the regional COVID-19 situation, the institutional resources and outcomes, and the results from recent patients in similar circumstances. Although no universal criteria exist and different institutions use variations of the general recommendations, some suggested criteria include confirmation of two consecutive negative SARS-CoV-2 tests and absence of symptoms (e.g., fever, respiratory symptoms). If the test is negative once, it is recommended to repeat testing after 24 h if high clinical suspicion as RT-PCR has <90% sensitivity [35, 36].
Use of negative pressure room during hospital admission, limited visitation, rigorous use of personal protective equipment (PPE), hand washing before entering the room and upon exit (and during the visit as needed), and adequate postings in the room door to advise of the SARS-CoV-2 status are important general measures to minimize contagion. All disposable equipment and PPE should be discarded inside the room before exiting. Prophylactic anticoagulation (e.g., low molecular weight heparin if platelets >50,000/μL) for all inpatients might be appropriate [37]. Any new fever while on treatment requires re-testing for SARS-CoV-2 if previously negative. Slots for outpatient appointments, transportation options, clinician availability, availability of blood products and new and even standard drugs, and enrollment into trials may all be limited during the pandemic as resources are being diverted to areas of greatest need. Multidisciplinary coordination between hematologist/oncologist, infectious disease expert, pulmonologist/intensivist, and nursing managers is crucial at multiple levels. Importantly, infectious disease specialists should be involved early in the management of patients with active COVID-19 to co-manage whenever possible. General recommendations pertaining to care of patients with leukemia are presented in Table 2.
Whenever possible, ambulatory patients should be managed through telemedicine. Many patients with myeloproliferative neoplasm, chronic myeloid leukemia, low-risk myelodysplastic syndrome, chronic lymphocytic leukemia, and some patients with acute leukemia in remission might be good candidates for these approaches. An adequate supply of their ongoing treatment should be secured when possible to minimize interruptions unless treatment pauses are indicated.
The role of granulocyte colony-stimulating factor (G-CSF) injections and subsequent neutrophil recovery to minimize COVID-19 complications is not clear. The rare but potential risk of worsening pulmonary injury in COVID-19 infection requires careful assessment when considering the use of growth factors for patients with moderate to severe COVID-19 infection [39].
Geriatric assessment prior to starting new regimens is recommended for older patients [40]. Home premedication prior to administrating outpatient infusions, when appropriate, and the use of prophylactic growth factors should be considered. Prophylactic antimicrobials for patients with prolonged neutropenia should include antibacterial, antifungal, and antiviral agents. Reduction in donor availability due to voluntary withdrawal, travel restriction, increased donor deferrals, interruptions in stem cell product supply chain, blood product shortage, and limited inpatient beds may make intensive chemotherapy and allo-SCT difficult or of higher risk for many patients.
Strategies to delay or defer allo-SCT may be pursued in select patients. Back-up donors, matched related donors or haplo-identical allo-SCT, and cryopreservation of the stem cell product before conditioning can help navigate some barriers [41•]. Controversial allo-SCT indications like patients with active refractory acute leukemia or those with a high risk of non-relapse mortality should avoid transplantation.
Acute Myeloid Leukemia (AML)
Patients with acute myeloid leukemia are at very high risk for mortality from COVID-19, particularly during induction [42•]. Considerations for the management of AML patients with COVID-19 are presented in Table 3.
Induction
Patients with AML should be screened for SARS-CoV-2 with a nasopharyngeal swab and undergo imaging, ideally CT of the chest prior to the start of induction chemotherapy. Patients who test positive for SARS-CoV-2, particularly if symptomatic, should have initiation of therapy delayed whenever possible. This time can be also used to obtain the results of the cytogenetic and molecular assessments. Management of COVID-19 can be done according to recommended guidelines. In some patients with proliferative disease, hydroxyurea or a single dose of cytarabine may help control symptoms and proliferation. Patients who test negative for COVID-19 may start induction therapy once workup is completed. Those who tested positive may initiate therapy after 10–14 days from positive testing. For patients who are symptomatic, treatment should ideally be delayed until symptoms resolve (no respiratory symptoms, no fever for at least 24 h unless fever is confirmed to be from other reasons). AML treatment can be done per standard approaches. Induction chemotherapy with cytarabine and anthracycline (e.g., 3+7 or other similar regimens per institutional guidelines) may be used for fit and younger (e.g., 18–65 years) patients [13•]. Fit adults ≥50 years old, receiving induction chemotherapy, should preferably remain hospitalized until counts recovery (absolute neutrophil count>1000/μL). Unfit or older patients (e.g., >65 years) should receive lower intensity regimens based on hypomethylating agents (HMA) or low-dose cytarabine. Venetoclax improves overall survival rates when combined with HMA or low-dose cytarabine but adds risk of prolonged myelosuppression. A bone marrow aspiration on days 14–21 is recommended to assess response and if blasts <5%, venetoclax should be interrupted. After the first cycle with venetoclax-based combination, if bone marrow contains <5% blasts, then growth factors may be used to shorten the duration of neutropenia. Glasdegib and low-dose cytarabine are also approved for such patients and cause less myelosuppression so it can be considered if myelosuppression is a concern.
Consolidation/Maintenance
The timing of consolidation should be individualized for every patient. For patients without high-risk features, the start of consolidation may be delayed, the dose reduced, and/or the number of cycles reduced. These decisions could be informed by assessment of measurable residual disease (MRD) whenever possible. Consolidation with cytarabine on days 1–3 (instead of on days 1, 3, and 5) has been found to be equally effective and to reduce myelosuppression and should be used when consolidation is to be administered [43, 44]. Outpatient administration should be favored whenever possible. Subsequent cycles of consolidation may be delayed (e.g., to 42–56-day cycles, instead of 28-day cycles) to allow a more robust recovery of counts between cycles and space out the periods of myelosuppression, particularly if access to regular monitoring, transfusions, and hospitalization is restricted. The number of consolidation cycles can be reduced to 2 or 3 particularly for patients with negative MRD after 2 cycles of consolidation chemotherapy. For patients where a stem cell transplant is indicated but not possible immediately, additional cycles of consolidation may be administered until SCT is considered feasible and safe. Allo-SCT should be deferred for patients without adverse risk disease especially when they are MRD negative. Maintenance with azacitidine ± venetoclax can also be considered as a bridging therapy until allo-SCT or as an alternative to intensive post-remission therapy after careful consideration [45]. A lower dose of venetoclax may be used to reduce risk of prolonged cytopenias, and for patients at higher risk of myelosuppression or when access to clinics, laboratory, and transfusions is limited, HMA can be used alone after complete remission.
Relapsed/Refractory Disease
These patients pose a particular challenge. For patients with a reasonable curative potential and with an option for a stem cell transplant, similar considerations as for initial therapy can be followed. Clinical trials should be considered when feasible. Re-assessment of cytogenetic and molecular characteristics of the disease are important as they may identify features that allow consideration of target-specific agents that may offer reasonable response probabilities with less myelosuppression such as FLT3 inhibitors, and IDH inhibitors. The timing of initiation of therapy should be tailored to the status of COVID-19 infection and the availability of adequate support in a similar way as has been described for frontline therapy.
Acute Promyelocytic Leukemia (APL)
APL is a highly curable disease, and delays in treatment can have serious adverse consequences. Thus, patients with APL should receive all-trans retinoic acid (ATRA) upon confirmation of diagnosis. The addition of arsenic trioxide and for patients with high-risk disease, gemtuzumab ozogomicin, or idarubicin should also be considered, following standard guidelines [46]. These treatments are not highly myelosuppressive, but patients require hospitalization for at least the first 14–21 days. All necessary precautions discussed earlier in this manuscript should be adopted to minimize the risk. Delaying the addition of arsenic trioxide may be considered in some low-risk patients if the patient has active COVID-19 and/or if the hospital resources are seriously limited.
Acute Lymphoblastic Leukemia (ALL)
General Considerations
ALL patients have been reported to have prolonged PCR positivity for weeks after COVID infection (possibly due to detection of viral fragments that have not cleared) but limited patient experience seems to support that it is safe to resume treatment once symptoms have resolved completely [47]. Table 3 highlights common issues relevant to care of ALL during COVID-19 times. All patients with newly diagnosed ALL should be screened for COVID-19 with the nasopharyngeal swab and CT chest. If positive, systemic intensive chemotherapy should be delayed whenever possible (e.g., in the absence of major hyperleukocytosis) although intrathecal treatment may be given for central nervous system symptoms [47]. Corticosteroids are an important component of treatment and may be used to manage ALL when temporizing measures are needed. In addition, dexamethasone can reduce mortality of patients hospitalized for COVID-19 [24]. Use of asparaginase is probably best avoided in most instances due to additive risk of thromboses with COVID-19. Growth factors are routinely used to hasten neutrophil recovery in ALL regimens and should be used if chemotherapy is being administered to minimize prolonged myelosuppression.
Induction
For Philadelphia (Ph) chromosome–negative disease, multi-drug chemotherapy regimens such as hyerCVAD (hyperfractionated cyclophosphamide, vincristine, doxorubicin, methotrexate, cytarabine, dexamethasone, and intrathecal chemotherapy) comprises the backbone of ALL treatment in young adults (e.g., <65 years) [48]. Older patients may receive reduced-intensity regimens (e.g., mini-hyper-CVAD; 50% dose–reduced cyclophosphamide, vincristine, dexamethasone, 75% dose–reduced methotrexate, 83% dose–reduced cytarabine, and omission of doxorubicin), possibly in combination with inotuzumab and alternating with blinatumomab [49]. A recent report suggests reduced myelosuppression with this approach [50]. For young adults (up to 40 years) treated with pediatric-inspired regimens, some recommendations include dose-reducing daunorubicin (50%) or using a reduced-dose Peg-asparaginase (e.g., 1000 IU/m2) in patients with high risk for complications [47]. However, the additive thrombotic potential when using asparaginase in the context of the risk of COVID-19-associated coagulopathy makes this regimen a less desirable option [51]. Rituximab is frequently used for CD20-positive ALL, but the associated B-cell depletion and the limited efficacy as a single agent make its use also less desirable in the setting of active COVID-19. Some recommend immunoglobulin G (IgG) level monitoring when it is used [47]. When available, outpatient administration of chemotherapy is preferred, but this requires existing outpatient protocols, robust support infrastructure, and close monitoring.
For Ph-positive ALL, a second or third-generation tyrosine kinase inhibitor (TKI) alone or in combination with dexamethasone and blinatumomab can result in a high response rate and minimal myelosuppression [52, 53]. These combinations should be considered in patients with active COVID-19 in lieu of TKI + intensive chemotherapy. Patients may require hospitalization for the first few days of the first cycle of blinatumomab infusion to monitor for cytokine release syndrome, and the logistics of the continuous infusion may make administration of blinatumomab difficult when hospital and clinic resources are stretched. This regimen however starts with dasatinib and dexamethasone only which is less daunting and may be administered in the outpatient setting once the patient is stable. Other options are TKI plus mini-hyper-CVAD or TKI plus vincristine and steroids [54].
For patients with T-cell ALL, regimens such as hyper-CVAD with the addition of asparaginase and nelarabine are frequently recommended [55, 56]. However, in the context of active COVID-19, such approaches might not be optimal because of the myelosuppression induced by the combination chemotherapy and the coagulopathy associated with asparaginase. Reduced-intensity approaches can be considered, such as dexamethasone alone or in combination with nelarabine if therapy has to be initiated in a patient with active COVID-19 in an attempt to minimize prolonged and profound myelosuppression. A full combination regimen can be started once the patient recovers from the viral infection.
Consolidation/Maintenance
Consolidation is an integral part of ALL regimens. MRD status is checked during treatment and patients achieving negative MRD may be switched to early maintenance. Persistent MRD-positive patients after 2–3 cycles of intensive chemotherapy would benefit from switching to blinatumomab if not included in the initial regimen [57]. In patients where consolidation with intensive chemotherapy is not desirable because of an active COVID-19, temporizing measures such as dexamethasone with or without rituximab (if CD20 positive) may be considered, resuming consolidation once the patient is fully recovered from COVID-19. A dose-reduced consolidation (such as mini-hyper-CVAD) can also be considered.
Dose reductions for 6-mercaptopurine and/or methotrexate to minimize myelosuppression can be considered while on maintenance when using POMP (6-mercaptopurine, vincristine, methotrexate, and prednisone). Blinatumomab or inotuzumab can be used as later intensification strategy. High-risk ALL and relapsed ALL in second complete remission will require an allo-SCT, but the timing of the SCT should be delayed if the patient has active COVID-19, and adjusted to local conditions and hospital resources.
Relapsed/Refractory Disease
In a salvage setting, blinatumomab and inotuzumab offer survival benefit compared to intensive chemotherapy. Both are also less myelosuppressive than intensive chemotherapy, and, in randomized trials, infections were less common among patients treated with these agents compared to those treated with standard chemotherapy. Thus, these agents should be preferred for patients with COVID-19. Depending on the severity of the SARS-CoV-2 infection, the initiation may need to be delayed in some instances and patients temporized with dexamethasone.
Myelodysplastic Syndromes (MDS)
Epidemiology
MDS, particularly in patients with high-risk disease, may pose an increased risk to severe COVID-19 and a risk or mortality similar to AML [8]. One report suggested a lethality rate of 73% among male MDS patients with COVID-19 [58]. Mortality was particularly high among patients in the higher risk categories. Patients also had multiple comorbidities, in accordance with their reported median age of 78 years. This was higher than the median age (73 years) of the overall MDS population. Table 4 lists common issues with care of MDS patients during these times.
Treatment
Older age at diagnosis, qualitative and quantitative defects in neutrophils, and higher comorbidity index put these patients at higher risk regardless of MDS. Patients with higher risk MDS (IPSS-R score of ≥3.5) may be in need of treatment more immediately, although in most instances, this can be delayed by a few weeks, a time that is also valuable in obtaining full cytogenetic and molecular characterization. A delay in the start of therapy is not associated with worsened survival or increased risk of transformation [59]. Thus, patients with active COVID-19 should in most instances delay the start of therapy and be managed with supportive measures (transfusion support, prophylactic, or therapeutic antibiotics). Once the patient has recovered, therapy with HMA can be initiated. The standard is single-agent HMA and this approach should be used unless the patient is eligible for an available high-priority clinical trial, provided trials are feasible based on local conditions. HMA may alter type 1 interferon response, but its effect in the clinical course of COVID 19 infection is not clear [60]. Available therapies for patients with low-risk MDS such as erythroid stimulating agents, lenalidomide, and luspatercept reduce transfusion requirements and may be considered for such patients. Lenalidomide may cause myelosuppression in some patients with del (5q) MDS, so blood counts should be monitored closely upon starting therapy with lenalidomide. MDS/MPN (myelodysplastic syndrome and myeloproliferative neoplasm) overlap entities such as chronic myelomonocytic leukemias have baseline inflammatory cytokine profile and higher expression of ACE2 (angiotensin-converting enzyme 2) expression in monocytes and macrophages [61, 62]. Few cases of severe COVID-19 have been reported in patients with CMML and prophylactic cytoreduction is suggested as a strategy to reduce the risk of cytokine storm in the event of COVID-19 infection later [63,64,65] The same principles discussed earlier for MDS can be used for managing patients with these entities.
Myeloproliferative Neoplasms
Epidemiology
In a survey from the GIMEMA group, 33.6% of tested patients with MPN were positive for SARS-CoV-2 (0.002% of all MPN patients included in the survey) [66]. Although 36% were asymptomatic, 27.8% had pneumonia. Mortality among patients who tested positive was 22%. A separate report, also from Italy, reported a mortality rate of 48% among patients with myelofibrosis, while no increased risk of mortality was identified for patients with essential thrombocythemia, polycythemia vera, and prefibrotic myelofibrosis [67]. Although these results were collected from a survey not reflecting the whole universe of patients and do not have full information about comorbidities and other risk factors, it highlights the seriousness of COVID-19 among patients with MPN.
Treatment
Patients in need of low-risk interventions such as phlebotomies or aspirin for prophylaxis of thrombosis should be managed as needed. Increased risk of thrombosis with MPN is a concern and this might be increased in the setting of COVID-19. Patients should be carefully assessed and managed according to standard guidelines. MPN patients with COVID-19 infection when hospitalized should be administered low molecular weight or unfractionated heparin in prophylactic or intermediate doses during inpatient or intensive care unit settings. For patients with myelofibrosis who are very symptomatic and/or with a very enlarged spleen, ruxolitinib can be initiated. Because of the effect ruxolitinib has on reducing pro-inflammatory cytokines, several studies are exploring the role of ruxolitinib in reducing the inflammatory consequences of COVID-19 [68]. However, it is not yet known whether it has a role in this indication. A recent phase 2 randomized study of patients with severe COVID-19 randomized to standard of care alone or with ruxolitinib failed to show statistically significant clinical improvement with ruxolitinib, but there was a trend in radiologic improvement and survival in favor of patients receiving ruxolitinib [69]. Still, patients with MPN in need of therapy with ruxolitinib can be treated and monitored closely. Patients already on therapy with ruxolitinib should not discontinue therapy if they develop COVID-19 [70]. Discontinuation of ruxolitinib has been associated with a “cytokine storm” that can have serious consequences [71]. In a recent report, among patients with MPN, treatment with ruxolitinib was not associated with an increased risk of death in a multivariate analysis, but treatment discontinuation led to death in 11 of 45 patients [67]. It is therefore important to ensure patients have adequate supplies of ruxolitinib. The theoretical immunosuppressive effects of ruxolitinib do not appear to have significant clinical consequences in general or among patients with COVID-19 [72]. Common considerations for MPN management are outlined in Table 4.
Chronic Myeloid Leukemia (CML)
Epidemiology
Prevalence of COVID-19 in CML patients was 0.9% (0.1% in the general population) in a Chinese study, but preliminary results from a Dutch study did not show significantly increased prevalence compared to the general population [73••, 74•]. No signal for increased mortality was observed for patients receiving tyrosine kinase inhibitors (TKIs) in one report [75]. The International CML Foundation recently reported on 110 CML patients with COVID-19 from 20 countries around the world [76]. Seventy percent of them were on treatment with TKIs while others were not receiving treatment either because of elective treatment discontinuation (n=8) or other reasons, or treatment information was not available (n=14). COVID-19 was asymptomatic in 8 (7%) patients, mild in 49 (45%), moderate in 19 (17%), and severe in 19 (17%) (unknown in 15). At the time of the report, 12 patients (14%) had died due to COVID-19.
Treatment
Evaluation and choice of therapy for newly diagnosed CML is generally unaffected by COVID-19 [77]. TKIs can cause myelosuppression during the initial weeks of therapy and laboratory workup every 1–2 weeks is recommended [52]. This is less of a concern for stable patients on TKIs and hence therapy can be continued in the absence of neutropenia. TKIs do not seem to increase the risk of acquiring SARA-CoV-2 or of causing severe disease in COVID-19 patients. However, the side effect profile of some TKI may overlap with COVID-19-induced organ damage or predispose to complications. Dasatinib for example can cause pleural effusions and pulmonary arterial hypertension; nilotinib, dasatinib, and ponatinib can cause arterio-occlusive adverse events; bosutinib can frequently cause diarrhea. COVID-19 can cause similar symptoms in some patients and testing for active and recent infection with nasopharyngeal swab and antibody serology is recommended when there is increased symptom burden. For CML patients with mild infections, TKIs can be continued. However, in case of severe COVID-19 infection or patients with cardiopulmonary symptoms, consideration can be given to a treatment hiatus, particularly for patients with stable disease. For accelerated phase and, particularly, for blast phase CML, TKIs are frequently combined with intensive or lower intensity chemotherapy. Considerations for initiation of chemotherapy parallel what was discussed earlier for AML and ALL. In patients with active disease, single-agent TKI can be used until the patient recovers from COVID-19 and then add the chemotherapy if this is being considered as part of the treatment plan (e.g., blast phase CML).
For patients in remission, routine BCR-ABL1 PCR monitoring (typically every 3 months) may be spaced out further and remote testing can be utilized along with telemedicine. Follow-up bone marrow biopsies and attempts at treatment-free remission should be delayed unless absolutely necessary and adequate resources and monitoring are available.
Chronic Lymphocytic Leukemia (CLL)
Epidemiology
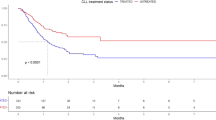
CLL is a disease mostly affecting older patients which is frequently accompanied clinically by both humoral and cell-mediated immune dysfunctions. In Italy and Spain, 79% of CLL patients hospitalized with COVID-19 had severe disease (need of supplemental oxygen and/or intensive care admission) compared to 13.4% among the general population in the same countries; 36.4% of the CLL patients included in this analysis died, underscoring the high risk for these patients [78]. Interestingly, 60% of patients with severe COVID-19 were off therapy within the last 12 months or had never received therapy for CLL, compared to less severe cases (38.5%). The effect of various treatments however may be different. Hospitalization rates for severe COVID-19 were lower for patients on ibrutinib compared to those on other regimens or off treatment. Interestingly, BTK (Bruton tyrosine kinase) inhibitors appear to exert some protective effect against severe disease, consistent with studies showing an anti-inflammatory effect in CLL [79]. Contemporary issues in CLL management are enlisted in Table 5.
Treatment
For patients with CLL who are on surveillance, telemedicine visits with home labs or no labs are suggested for follow-up. Initiation of treatment according to the International Workshop on CLL indications (anemia and/or thrombocytopenia, splenomegaly, lymphadenopathy, lymphocyte doubling time <6 months, extranodal involvement, B symptoms) are usually not urgent and in most instances can be delayed with close follow-up, until symptoms of COVID-19 resolve and resources are available and circumstances are appropriate for proper monitoring.
Chemoimmunotherapy regimens like FCR (fludarabine, cyclophosphamide, rituximab) and BR (bendamustine, rituximab) should be avoided in most instances in favor of highly effective oral targeted agents. BTK inhibitors like ibrutinib and acalabrutinib require fewer clinic visits. Interestingly, in vitro studies have suggested that these agents might be protective in COVID-19 infection [80, 81]. Patients still should be monitored for efficacy and safety, with telehealth whenever possible. Anti-CD20-targeted agents like rituximab and obinutuzumab carry the risk of B-cell lymphodepletion and may worsen the severity of COVID-19 infection. These should therefore be avoided or deferred [82,83,84]. Venetoclax and obinutuzumab are the only fixed duration frontline therapy but carry risk of tumor lysis syndrome and neutropenia in addition to the lymphopenia associated with obinutuzumab. It is ideal to delay the start of therapy for patients with COVID-19 or at high risk of infection. Patients treated with venetoclax or with neutropenia from other therapies can be supported with filgrastim. Patients with indications for intravenous immunoglobulins (IVIG) may continue these infusions, but the frequency should be evaluated according to patient and healthcare facility’s needs. IVIG increases the risk of thrombosis, which should be considered. There are reports of successful treatment of severely ill COVID-19 patients with high-dose IVIG [85, 86]. A syndrome of CLL flare and cytokine release akin to COVID-19 is seen on discontinuation of BCR signaling inhibitors (ibrutinib, acalabrutinib, idelalisib, duvelisib) which resolves on resumption of the drug [87, 88]. Patients with CLL who contract COVID-19 should consider stopping or dose adjusting immunosuppressive therapy until they are free of symptoms and at least 14 days from onset of symptoms with preferably negative nasopharyngeal swab [14].
Conclusion
COVID-19 is an unprecedented healthcare crisis, and this has percolated to affect patients’ care and prognosis. Patients with leukemia and hematological malignancies and the health care infrastructure are forced to cope up with this situation. Patients with leukemia are in many instances at increased risk of severe disease and mortality. Sound ethical rationing of the existing resources and using evidence-based adjustments to the treatment paradigms will be our path forward as the COVID-19 outbreak is likely to last months and might recur in the future in a cyclical pattern [89].
Availability of Data and Materials
Not applicable.
Code Availability
Not applicable.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Mizumoto K, Kagaya K, Zarebski A, Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill Bull Eur sur les Mal Transm Eur Commun Dis Bull. 2020;25(10).
Guan W-J, Ni Z-Y, Hu Y, Liang W-H, Ou C-Q, He J-X, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–20.
Nuzzo J, Moss B, Kahn J, Rutkow L, Laboratory AP. COVID-19 Dashboard by the Center for systems science and engineering (CSSE) at Johns Hopkins University [Internet]. 2021 [cited 2021 Feb 6]. Available from: https://coronavirus.jhu.edu/map.html
Wu Z, JM MG. Characteristics of and Important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–42. https://doi.org/10.1001/jama.2020.2648.
Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–7.
He W, Chen L, Chen L, Yuan G, Fang Y, Chen W, et al. COVID-19 in persons with haematological cancers. Leukemia. 2020;34(6):1637–45.
Yu J, Ouyang W, Chua MLK, Xie C. SARS-CoV-2 Transmission in patients with cancer at a tertiary care hospital in Wuhan. China. JAMA Oncol. 2020;6(7):1108–10.
Piñana JL, Martino R, García-García I, Parody R, Morales MD, Benzo G, et al. Risk factors and outcome of COVID-19 in patients with hematological malignancies. Exp Hematol Oncol. 2020;9:21.
Mehta V, Goel S, Kabarriti R, Cole D, Goldfinger M, Acuna-Villaorduna A, et al. Case fatality rate of cancer patients with COVID-19 in a New York hospital system. Cancer Discov. 2020;10(7):935 LP–941 Available from: http://cancerdiscovery.aacrjournals.org/content/10/7/935.abstract.
Passamonti F, Cattaneo C, Arcaini L, Bruna R, Cavo M, Merli F, et al. Clinical characteristics and risk factors associated with COVID-19 severity in patients with haematological malignancies in Italy: a retrospective, multicentre, cohort study. Lancet Haematol. 2020.;7(10):e737–45. Available from: https://pubmed.ncbi.nlm.nih.gov/32798473This is one of the first studies with a sizable patient population (536 COVID-19-positive patients with hematological malignancies who were hospitalized across multiple care centers in Itality). It showed that these patients had significantly worse outcomes than both healthy patients and COVID-19-negative patients with hematological malignancies. Therefore, it is vital to formulate appropriate management for these at-risk patients.
Segelov E, Underhill C, Prenen H, Karapetis C, Jackson C, Nott L, et al. Practical considerations for treating patients with cancer in the COVID-19 pandemic. JCO Oncol Pract. 2020;16(8):467–82 This article not only highlights that comprehensive care for cancer patients during the pandemic should not be interrupted or compromised but also provides reasonable changes to standard practice to be adopted by oncology clinicians.
Paul S, Rausch CR, Jain N, Kadia T, Ravandi F, DiNardo CD, et al. Treating leukemia in the time of COVID-19. Acta Haematol. 2020:1–13 This paper outlines the expert opinion from MD Anderson (large leukemia center in USA) regarding the management of leukemia patients with and without evidence of COVID-19 published in the midst of the pandemic.
Brissot E, Labopin M, Baron F, Bazarbachi A, Bug G, Ciceri F, et al. Management of patients with acute leukemia during the COVID-19 outbreak: practical guidelines from the acute leukemia working party of the European Society for Blood and Marrow Transplantation. Bone Marrow Transplant. 2020:1–4 This article was one of the early articles providing general approaches to acute leukemia and stem cell transplantation in the time of COVID 19 pandemic.
Rossi D, Shadman M, Condoluci A, Brown JR, Byrd JC, Gaidano G, et al. How we manage patients with chronic lymphocytic leukemia during the SARS-CoV-2 pandemic. HemaSphere. 2020;4(4):e432.
ASH. COVID-19 Resources [Internet]. 2021 [cited 2021 Feb 6]. Available from: https://www.hematology.org/covid-19#faq
Zeidan AM, Boddu PC, Patnaik MM, Bewersdorf JP, Stahl M, Rampal RK, et al. Special considerations in the management of adult patients with acute leukaemias and myeloid neoplasms in the COVID-19 era: recommendations from a panel of international experts. Lancet Haematol. 2020;7(8):e601–12 This article outlines the general framework for the care of patients with acute leukemia and myeloid neoplasms during COVID-19 pandemic from international experts. It addresses some key challenges related to resource allocation, scarce resouces, and access to clinical trials.
EHA. Recommendations for specific hematologic malignancies [Internet]. COVID-19 & Hematology Information Center. 2021 [cited 2021 Feb 6]. Available from: https://ehaweb.org/covid-19/covid-19-recommendations/recommendations-for-specific-hematologic-malignancies/
Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–7 Available from: http://www.sciencedirect.com/science/article/pii/S0049384820301201.
Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, et al. Remdesivir for the treatment of Covid-19 - preliminary report. N Engl J Med. 2020;383:1813–26.
Kalil AC, Patterson TF, Mehta AK, Tomashek KM, Wolfe CR, Ghazaryan V, et al. Baricitinib plus remdesivir for hospitalized adults with Covid-19. N Engl J Med. 2020; This is a fairly well-designed randomized double-blind study with about 500 patients in each arm to evaluate the effectiveness of baricitinib in combination with remdesivir for adults with COVID-19. This study found that this combination was superior to remdesivir alone in decreasing recovery time and promoting clinical improvement in COVID-19 infected patients. Baricitinib is a drug used to treat rheumatoid arthritis and its role in COVID-19 was actually theorized using artificial intelligence so this also represented an exciting new way to discover new treatment alternatives.
Chen P, Nirula A, Heller B, Gottlieb RL, Boscia J, Morris J, et al. SARS-CoV-2 neutralizing antibody LY-CoV555 in outpatients with Covid-19. N Engl J Med. 2021;384(3):229–37.
Gottlieb RL, Nirula A, Chen P, Boscia J, Heller B, Morris J, et al. Effect of bamlanivimab as monotherapy or in combination with etesevimab on viral load in patients with mild to moderate COVID-19: a randomized clinical trial. JAMA. 2021;325(7):632–44.
Weinreich DM, Sivapalasingam S, Norton T, Ali S, Gao H, Bhore R, et al. REGN-COV2, a neutralizing antibody cocktail, in outpatients with Covid-19. N Engl J Med. 2021;384(3):238–51.
RECOVERY Collaborative Group, Horby P, Lim WS, et al. Dexamethasone in Hospitalized Patients with Covid-19. N Engl J Med. 2021;384(8):693–704 https://doi.org/10.1056/NEJMoa2021436
Clark E, Guilpain P, Filip IL, Pansu N, Le Bihan C, Cartron G, et al. Convalescent plasma for persisting COVID-19 following therapeutic lymphocyte depletion: a report of rapid recovery. Br J Haematol. 2020;190:e154–6.
Guaraldi G, Meschiari M, Cozzi-Lepri A, Milic J, Tonelli R, Menozzi M, et al. Tocilizumab in patients with severe COVID-19: a retrospective cohort study. Lancet Rheumatol. 2020;2(8):e474–84.
Guaraldi G, Meschiari M, Cozzi-Lepri A, Milic J, Tonelli R, Menozzi M, et al. Tocilizumab in patients with severe COVID-19: a retrospective cohort study. The Lancet Rheumatology. 2020;2:e474–84.
Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N Engl J Med. 2020;383(27):2603–15.
Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384(5):403–16.
Gavillet M, Carr Klappert J, Spertini O, Blum S. Acute leukemia in the time of COVID-19. Leukemia research. 2020;92:106353.
Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of Chest CT and RT-PCR Testing for coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020;296(2):E32–40.
Sekeres MA, Elson P, Kalaycio ME, Advani AS, Copelan EA, Faderl S, et al. Time from diagnosis to treatment initiation predicts survival in younger, but not older, acute myeloid leukemia patients. Blood. 2009;113(1):28–36.
Röllig C, Kramer M, Schliemann C, Mikesch J-H, Steffen B, Krämer A, et al. Does time from diagnosis to treatment affect the prognosis of patients with newly diagnosed acute myeloid leukemia? Blood. 2020;136(7):823–30.
Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet (London, England). 2020;395:1033–4.
Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. 2020;296(2):E115–7.
Holborow A, Asad H, Porter L, Tidswell P, Johnston C, Blyth I, et al. The clinical sensitivity of a single SARS-CoV-2 upper respiratory tract RT-PCR test for diagnosing COVID-19 using convalescent antibody as a comparator. Clin Med. 2020.
Spyropoulos AC, Levy JH, Ageno W, Connors JM, Hunt BJ, Iba T, et al. Scientific and standardization committee communication: clinical guidance on the diagnosis, prevention, and treatment of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020;18(8):1859–65.
Tanasijevic AM, Revette A, Klepin HD, Zeidan A, Townsley D, DiNardo CD, et al. Consensus minimum hemoglobin level above which patients with myelodysplastic syndromes can safely forgo transfusions. Leuk Lymphoma. 2020:1–5.
Karlin L, Darmon M, Thiéry G, Ciroldi M, de Miranda S, Lefebvre A, et al. Respiratory status deterioration during G-CSF-induced neutropenia recovery. Bone Marrow Transplant. 2005;36(3):245–50.
Hamaker ME, Prins MC, Stauder R. The relevance of a geriatric assessment for elderly patients with a haematological malignancy--a systematic review. Leuk Res. 2014;38(3):275–83.
Ljungman P, Mikulska M, de la Camara R, Basak GW, Chabannon C, Corbacioglu S, et al. The challenge of COVID-19 and hematopoietic cell transplantation; EBMT recommendations for management of hematopoietic cell transplant recipients, their donors, and patients undergoing CAR T-cell therapy. Bone Marrow Transplant. 2020:1, 6 This manuscript highlights the different strategies and recommendations for stem cell transplant recipients, their donors, and patients undergoing CAR T-cell therapy with active COVID-19 infection or known exposure. It is suggested that delaying or deferring allo-SCT may be pursued in select patients. Other strategies included back-up donors, matched related donors or haplo-identical allo-SCT.
Núñez-Torrón C, García-Gutiérrez V, Tenorio-Núñez MC, Moreno-Jiménez G, López-Jiménez FJ, Herrera-Puente P. Poor outcome in patients with acute leukemia on intensive chemotherapy and COVID-19. Bone Marrow Transplant. 2020. https://doi.org/10.1038/s41409-020-0961-yOne of the first studies to specifically compare COVID-19-positive against negative patients with AML undergoing intensive chemotherapy. While no one died in the COVID-19-negative group, three out of the four COVID-19-positive patients died due to worsening respiratory syndrome despite receiving high-dose corticosteroids. This provides vital insight into the impact of COVID-19 infection in these high risk patients.
Jaramillo S, Benner A, Krauter J, Martin H, Kindler T, Bentz M, et al. Condensed versus standard schedule of high-dose cytarabine consolidation therapy with pegfilgrastim growth factor support in acute myeloid leukemia. Blood Cancer J. 2017;7(5):e564 Available from: https://pubmed.ncbi.nlm.nih.gov/28548643.
Burnett AK, Russell NH, Hills RK, Hunter AE, Kjeldsen L, Yin J, et al. Optimization of chemotherapy for younger patients with acute myeloid leukemia: results of the medical research council AML15 trial. J Clin Oncol Off J Am Soc Clin Oncol. 2013;31(27):3360–8.
Wei AH, Döhner H, Pocock C, Montesinos P, Afanasyev B, Dombret H, et al. The QUAZAR AML-001 maintenance trial: results of a phase III international, randomized, double-blind, placebo-controlled study of CC-486 (oral formulation of azacitidine) in patients with acute myeloid leukemia (AML) in first remission. Blood. 2019;134(Supplement_2):LBA-3. https://doi.org/10.1182/blood-2019-132405.
Tallman M, Rollig C, Zappasodi P, Schiller G, Mannis G, Olin R, et al. COVID-19 and acute myeloid leukemia: frequently asked questions 2021 . Available from: https://www.hematology.org/covid-19/covid-19-and-acute-myeloid-leukemia
Stock W, Patel A, O’Dwyer K, Bassan R, Zhou X, Huang X, et al. COVID-19 and adult ALL: frequently asked questions 2021. Available from: https://www.hematology.org/covid-19/covid-19-and-all
Kantarjian H, Thomas D, O’Brien S, Cortes J, Giles F, Jeha S, et al. Long-term follow-up results of hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone (hyper-CVAD), a dose-intensive regimen, in adult acute lymphocytic leukemia. Cancer. 2004;101(12):2788–801.
Jabbour E, Sasaki K, Ravandi F, Huang X, Short NJ, Khouri M, et al. Chemoimmunotherapy with inotuzumab ozogamicin combined with mini-hyper-CVD, with or without blinatumomab, is highly effective in patients with Philadelphia chromosome-negative acute lymphoblastic leukemia in first salvage. Cancer. 2018;124(20):4044–55.
Jabbour EJ, Sasaki K, Ravandi F, Short NJ, Garcia-Manero G, Daver N, et al. Inotuzumab ozogamicin in combination with low-intensity chemotherapy (mini-HCVD) with or without blinatumomab versus standard intensive chemotherapy (HCVAD) as frontline therapy for older patients with Philadelphia chromosome-negative acute lymphoblastic. Cancer. 2019;125(15):2579–86.
Lippi G, Sanchis-Gomar F, Favaloro EJ, Lavie CJ, Henry BM. Coronavirus disease 2019–associated coagulopathy. Mayo Clin Proc. 2021;96(1):203–17 Available from: https://www.sciencedirect.com/science/article/pii/S0025619620312635.
Liu-Dumlao T, Kantarjian HM, Quintas-Cardama A, Jabbour E, Burger JA, Alvarado Y, et al. Clinical significance of myelosuppression associated with the use of dasatinib and nilotinib as initial therapy in chronic phase (CP) of chronic myeloid leukemia (CML). Blood. 2011;118(21):2761. https://doi.org/10.1182/blood.V118.21.2761.2761.
Foà R, Bassan R, Vitale A, Elia L, Piciocchi A, Puzzolo M-C, et al. Dasatinib–blinatumomab for Ph-positive acute lymphoblastic leukemia in adults. N Engl J Med. 2020;383(17):1613–23. https://doi.org/10.1056/NEJMoa2016272.
Rousselot P, Coudé MM, Gokbuget N, Gambacorti Passerini C, Hayette S, Cayuela J-M, et al. Dasatinib and low-intensity chemotherapy in elderly patients with Philadelphia chromosome–positive ALL. Blood. 2016;128(6):774–82. https://doi.org/10.1182/blood-2016-02-700153.
Abaza Y, Kantarjian HM, Faderl S, Jabbour E, Jain N, Thomas D, et al. Hyper-CVAD plus nelarabine in newly diagnosed adult T-cell acute lymphoblastic leukemia and T-lymphoblastic lymphoma. Am J Hematol. 2018;93(1):91–9.
Marks DI, Rowntree C. Management of adults with T-cell lymphoblastic leukemia. Blood. 2017;129(9):1134–42. https://doi.org/10.1182/blood-2016-07-692608.
Gökbuget N, Dombret H, Bonifacio M, Reichle A, Graux C, Faul C, et al. Blinatumomab for minimal residual disease in adults with B-cell precursor acute lymphoblastic leukemia. Blood. 2018;131(14):1522–31.
Mossuto S, Attardi E, Alesiani F, Angelucci E, Balleari E, Bernardi M, et al. SARS-CoV-2 in Myelodysplastic syndromes: a snapshot from early Italian experience. HemaSphere. 2020;4(5) Available from: https://journals.lww.com/hemasphere/Fulltext/2020/10000/SARS_CoV_2_in_Myelodysplastic_Syndromes__A.16.aspx.
Komrokji RS, Al Ali N, Sallman DA, Padron E, Nazha A, Steensma DP, et al. What is the optimal time to initiate hypomethylating agents (HMA) in higher risk myelodysplastic syndromes (MDS)? Blood. 2018;132(Supplement 1):3098. https://doi.org/10.1182/blood-2018-99-114836.
Wolff F, Leisch M, Greil R, Risch A, Pleyer L. The double-edged sword of (re)expression of genes by hypomethylating agents: from viral mimicry to exploitation as priming agents for targeted immune checkpoint modulation. Cell Commun Signal. 2017;15(1):13.
Jafarzadeh A, Chauhan P, Saha B, Jafarzadeh S, Nemati M. Contribution of monocytes and macrophages to the local tissue inflammation and cytokine storm in COVID-19: lessons from SARS and MERS, and potential therapeutic interventions. Life Sci. 2020;257:118102.
Niyongere S, Lucas N, Zhou J-M, Sansil S, Pomicter AD, Balasis ME, et al. Heterogeneous expression of cytokines accounts for clinical diversity and refines prognostication in CMML. Leukemia. 2019;33(1):205–16.
Patnaik MM, Lasho T, Padron E, McCullough K, Al-Kali A, Tefferi A, et al. Special considerations in the management of patients with myelodysplastic myndrome / myeloproliferative neoplasm overlap syndromes during the SARS-CoV-2 pandemic. Am J Hematol. 2020;95(8):E203–8 Available from: https://pubmed.ncbi.nlm.nih.gov/32356322.
Jain A, Jain A, Prasad P, Chaudhry S, Sharma M, Khunger JM, et al. COVID-19 in a patient with chronic myelomonocytic leukemia: a twisting tale. Blood Res. 2020;55(4):278–81 Available from: https://pubmed.ncbi.nlm.nih.gov/33380560.
Sekeres MA, Steensma DP, DeZern A, Roboz G, Garcia-Manero G, Komrokji R. COVID-19 and myelodysplastic syndromes: frequently asked questions 2021. Available from: https://www.hematology.org/covid-19/covid-19-and-myelodysplastic-syndromes
Breccia M, Piciocchi A, De Stefano V, Finazzi G, Iurlo A, Fazi P, et al. COVID-19 in Philadelphia-negative myeloproliferative disorders: a GIMEMA survey. Leukemia. 2020. https://doi.org/10.1038/s41375-020-01032-0.
Barbui T, Vannucchi AM, Alvarez-Larran A, Iurlo A, Masciulli A, Carobbio A, et al. High mortality rate in COVID-19 patients with myeloproliferative neoplasms after abrupt withdrawal of ruxolitinib. Leukemia. 2021;35(2):485–93 Available from: https://pubmed.ncbi.nlm.nih.gov/33414483.
La Rosée F, Bremer HC, Gehrke I, Kehr A, Hochhaus A, Birndt S, et al. The Janus kinase 1/2 inhibitor ruxolitinib in COVID-19 with severe systemic hyperinflammation. Leukemia. 2020;34(7):1805–15. https://doi.org/10.1038/s41375-020-0891-0.
Cao Y, Wei J, Zou L, Jiang T, Wang G, Chen L, et al. Ruxolitinib in treatment of severe coronavirus disease 2019 (COVID-19): a multicenter, single-blind, randomized controlled trial. J Allergy Clin Immunol. 2020;146(1):137–146.e3.
Mesa R, Alvarez-Larran A, Harrison C, Kiladjian J-J, Rambaldi A, Tefferi A, et al. COVID-19 and myeloproliferative neoplasms: frequently asked questions 2021. Available from: https://www.hematology.org/covid-19/covid-19-and-myeloproliferative-neoplasms
Tefferi A, Pardanani A. Serious adverse events during ruxolitinib treatment discontinuation in patients with myelofibrosis. Mayo Clin Proc. 2011;86(12):1188–91.
Heine A, Held SAE, Daecke SN, Wallner S, Yajnanarayana SP, Kurts C, et al. The JAK-inhibitor ruxolitinib impairs dendritic cell function in vitro and in vivo. Blood. 2013;122(7):1192–202. https://doi.org/10.1182/blood-2013-03-484642.
GICG E, EGW H, NMA B, Westerweel PE. Prevalence of COVID-19 diagnosis in Dutch CML patients during the 2020 SARS-CoV2 pandemic. A prospective cohort study. Leukemia. 2020;34:2533–5 This study was a prospective Dutch observational study assessing the differences in susceptibility for COVID-19 and the severity of the disease course in adult CML patients and their adult housemates (included as control group). They found no significantly increased prevalance of COVID-19 in CML patients. This study also suggested that patients can safely continue their TKI.
Li W, Wang D, Guo J, Yuan G, Yang Z, Gale RP, et al. COVID-19 in persons with chronic myeloid leukaemia. Leukemia. 2020;34(7):1799–804. https://doi.org/10.1038/s41375-020-0853-6First article to report on COVID-19 in pateints with CML. They found an increased prevalance of COVID-19 infection in CML patients in Hubei, China, when compared to the prevalance of the general population in that particular region. The major drawback of this retrospective observational analysis was that follow-up data were not provided and the control group was not included.
Başcı S, Ata N, Altuntaş F, Yiğenoğlu TN, Dal MS, Korkmaz S, et al. Outcome of COVID-19 in patients with chronic myeloid leukemia receiving tyrosine kinase inhibitors. J Oncol Pharm Pract Off Publ Int Soc Oncol Pharm Pract. 2020;1078155220953198.
Rea D, Mauro MJ, Cortes JE, Jiang Q, Pagnano, Katia B, Ongondi M, Kok CH, et al. COVID-19 in patients (pts) with chronic myeloid leukemia (CML): results from the International CML foundation (iCMLf) CML and COVID-19 (CANDID) study. In: 62nd ASH Annual Meeting and Exposition. 2020. Available from: https://ash.confex.com/ash/2020/webprogram/Paper140161.html
Mauro M, Druker B, Radich J, Cortes J, Brümmendorf TH, Saglio G, et al. COVID-19 and CML: frequently asked questions 2021. Available from: https://www.hematology.org/covid-19/covid-19-and-cml
Scarfò L, Chatzikonstantinou T, Rigolin GM, Quaresmini G, Motta M, Vitale C, et al. COVID-19 severity and mortality in patients with chronic lymphocytic leukemia: a joint study by ERIC, the European Research Initiative on CLL, and CLL Campus. Leukemia. 2020;34(9):2354–63.
Roschewski M, Lionakis MS, Sharman JP, Roswarski J, Goy A, Monticelli MA, et al. Inhibition of Bruton tyrosine kinase in patients with severe COVID-19. Sci Immunol. 2020;5(48).
Thibaud S, Tremblay D, Bhalla S, Zimmerman B, Sigel K, Gabrilove J. Protective role of Bruton tyrosine kinase inhibitors in patients with chronic lymphocytic leukaemia and COVID-19. Br J Haematol. 2020;190:e73–6.
Treon SP, Castillo JJ, Skarbnik AP, Soumerai JD, Ghobrial IM, Guerrera ML, et al. The BTK inhibitor ibrutinib may protect against pulmonary injury in COVID-19-infected patients. Blood. 2020;135(21):1912–5.
Leipe J, Wilke EL, Ebert MP, Teufel A, Reindl W. Long, relapsing, and atypical symptomatic course of COVID-19 in a B-cell-depleted patient after rituximab. Vol. 50, Seminars in arthritis and rheumatism. United States. 2020:1087–8.
Schulze-Koops H, Krueger K, Vallbracht I, Hasseli R. Skapenko A. Increased risk for severe COVID-19 in patients with inflammatory rheumatic diseases treated with rituximab. Ann Rheum Dis. 2020;annrheumdis-2020:218075 Available from: http://ard.bmj.com/content/early/2020/06/25/annrheumdis-2020-218075.abstract.
Avouac J, Airó P, Carlier N, Matucci-Cerinic M, Allanore Y. Severe COVID-19-associated pneumonia in 3 patients with systemic sclerosis treated with rituximab. England: Annals of the rheumatic diseases; 2020.
Mohtadi N, Ghaysouri A, Shirazi S, Ansari S, Shafiee E, Bastani E, et al. Recovery of severely ill COVID-19 patients by intravenous immunoglobulin (IVIG) treatment: a case series. Virology. 2020;548:1–5.
Cao W, Liu X, Bai T, Fan H, Hong K, Song H, et al. High-dose intravenous immunoglobulin as a therapeutic option for deteriorating patients with coronavirus disease 2019. Open forum Infect Dis. 2020;7(3):ofaa102.
Castillo JJ, Gustine JN, Meid K, Dubeau T, Severns P, Treon SP. Ibrutinib withdrawal symptoms in patients with Waldenström macroglobulinemia. Haematologica. 2018;103:e307–10.
Woyach JA, How I. manage ibrutinib-refractory chronic lymphocytic leukemia. Blood. 2017;129(10):1270–4. https://doi.org/10.1182/blood-2016-09-693598.
Dowell SF, Ho MS. Seasonality of infectious diseases and severe acute respiratory syndrome-what we don’t know can hurt us. Lancet Infect Dis. 2004;4(11):704–8.
Author information
Authors and Affiliations
Contributions
JC and NRK conceived the review. JC searched the literature and provided relevant references. NRK reviewed and analyzed the literature. NRK drafted the report. JC edited the manuscripts and TL performed revisions. TL verified the accuracy of references.
Corresponding author
Ethics declarations
Conflict of Interest
NRK and TL have no conflict of interest to declare. JC is a consultant for Pfizer, Novartis, Takeda, Jazz, Biopath Holdings, and Sun Pharma; he has received research support (to his institution) from Pfizer, Novartis, Takeda, Jazz, Biopath Holdings, Sun Pharma, Actuate, and Telios.
Ethics Approval
Not applicable.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Leukemia
Rights and permissions
About this article
Cite this article
Karki, N.R., Le, T. & Cortes, J. The Care of the Leukemic Patients in Times of SARS-CoV-2. Curr Oncol Rep 23, 114 (2021). https://doi.org/10.1007/s11912-021-01111-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s11912-021-01111-0