Abstract
Glut1 deficiency syndrome (Glut1 DS) was originally described in 1991 as a developmental encephalopathy characterized by infantile onset refractory epilepsy, cognitive impairment, and mixed motor abnormalities including spasticity, ataxia, and dystonia. The clinical condition is caused by impaired glucose transport across the blood brain barrier. The past 5 years have seen a dramatic expansion in the range of clinical syndromes that are recognized to occur with Glut1 DS. In particular, there has been greater recognition of milder phenotypes. Absence epilepsy and other idiopathic generalized epilepsy syndromes may occur with seizure onset in childhood or adulthood. A number of patients present predominantly with movement disorders, sometimes without any accompanying seizures. In particular, paroxysmal exertional dyskinesia is now a well-documented clinical feature that occurs in individuals with Glut1 DS. A clue to the diagnosis in patients with paroxysmal symptoms may be the triggering of episodes during fasting or exercise. Intellectual impairment may range from severe to very mild. Awareness of the broad range of potential clinical phenotypes associated with Glut1 DS will facilitate earlier diagnosis of this treatable neurologic condition. The ketogenic diet is the mainstay of treatment and nourishes the starving symptomatic brain during development.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Simpson IA, Carruthers A, Vannucci SJ. Supply and demand in cerebral energy metabolism: the role of nutrient transporters. J Cereb Blood Flow Metab Off J Int Soc Cereb Blood Flow Metab. 2007;27(11):1766–91. doi:10.1038/sj.jcbfm.9600521.
Chugani HT. A critical period of brain development: studies of cerebral glucose utilization with PET. Prev Med. 1998;27(2):184–8. doi:10.1006/pmed.1998.0274.
De Vivo DC, Trifiletti RR, Jacobson RI, Ronen GM, Behmand RA, Harik SI. Defective glucose transport across the blood–brain barrier as a cause of persistent hypoglycorrhachia, seizures, and developmental delay. N Engl J Med. 1991;325(10):703–9. doi:10.1056/NEJM199109053251006.
Seidner G, Alvarez MG, Yeh JI, O'Driscoll KR, Klepper J, Stump TS, et al. GLUT-1 deficiency syndrome caused by haploinsufficiency of the blood–brain barrier hexose carrier. Nat Genet. 1998;18(2):188–91. doi:10.1038/ng0298-188.
Klepper J, Scheffer H, Elsaid MF, Kamsteeg EJ, Leferink M, Ben-Omran T. Autosomal recessive inheritance of GLUT1 deficiency syndrome. Neuropediatrics. 2009;40(5):207–10. doi:10.1055/s-0030-1248264.
•• Rotstein M, Engelstad K, Yang H, Wang D, Levy B, Chung WK, et al. Glut1 deficiency: inheritance pattern determined by haploinsufficiency. Ann Neurol. 2010;68(6):955–8. doi:10.1002/ana.22088. This article describes 2 patients with Glut1 DS as an autosomal recessive trait, demonstrating that the severity of the clinical syndrome was determined by the relative pathogenicity of the mutations and the resulting degree of haploinsufficiency. This illustrates an important principle that applies to all patients with Glut1DS.
•• Leen WG, Klepper J, Verbeek MM, Leferink M, Hofste T, van Engelen BG, et al. Glucose transporter-1 deficiency syndrome: the expanding clinical and genetic spectrum of a treatable disorder. Brain. 2010;133(Pt 3):655–70. doi:10.1093/brain/awp336. This articles describes the genetic and clinical features of a series of 57 patients with Glut1 DS, outlining the broad range of possible clinical syndromes, including patients with seizure onset at an older age and patients without epilepsy.
•• Yang H, Wang D, Engelstad K, Bagay L, Wei Y, Rotstein M, et al. Glut1 deficiency syndrome and erythrocyte glucose uptake assay. Ann Neurol. 2011;70(6):996–1005. doi:10.1002/ana.22640. This study validated the erythrocyte glucose uptake assay as a confirmatory functional diagnostic test, and as a surrogate marker of residual Glut1 activity which correlates with clinical severity.
De Vivo DC, Leary L, Wang D. Glucose transporter 1 deficiency syndrome and other glycolytic defects. J Child Neurol. 2002;17 Suppl 3:3S15–23. discussion 3S4-5.
Leary LD, Wang D, Nordli Jr DR, Engelstad K, De Vivo DC. Seizure characterization and electroencephalographic features in Glut-1 deficiency syndrome. Epilepsia. 2003;44(5):701–7.
• Pong AW, Geary BR, Engelstad KM, Natarajan A, Yang H, De Vivo DC. Glucose transporter type I deficiency syndrome: epilepsy phenotypes and outcomes. Epilepsia. 2012;53(9):1503–10. doi:10.1111/j.1528-1167.2012.03592.x. This retrospective study details the epilepsy phenotypes and treatment response to the ketogenic diet and anticonvulsant mediations in 87 patients with Glut1 DS. Also found was a significant lag in diagnosis, with mean age at seizure onset of 8 months to mean age at diagnosis of 5 years.
Suls A, Mullen SA, Weber YG, Verhaert K, Ceulemans B, Guerrini R, et al. Early-onset absence epilepsy caused by mutations in the glucose transporter GLUT1. Ann Neurol. 2009;66(3):415–9. doi:10.1002/ana.21724.
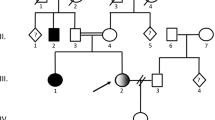
•• Mullen SA, Suls A, De Jonghe P, Berkovic SF, Scheffer IE. Absence epilepsies with widely variable onset are a key feature of familial GLUT1 deficiency. Neurology. 2010;75(5):432–40. doi:10.1212/WNL.0b013e3181eb58b4. The authors describe the variety of epilepsy syndromes observed in 2 kindreds (12 individuals) with SLC2A1 mutations, including idiopathic generalized epilepsy with absence, myoclonic-astatic, and focal seizures. These represent milder forms of epilepsy than were previously associated with Glut1 DS.
Afawi Z, Suls A, Ekstein D, Kivity S, Neufeld MY, Oliver K, et al. Mild adolescent/adult onset epilepsy and paroxysmal exercise-induced dyskinesia due to GLUT1 deficiency. Epilepsia. 2010;51(12):2466–9. doi:10.1111/j.1528-1167.2010.02726.x.
Striano P, Weber YG, Toliat MR, Schubert J, Leu C, Chaimana R, et al. GLUT1 mutations are a rare cause of familial idiopathic generalized epilepsy. Neurology. 2012;78(8):557–62. doi:10.1212/WNL.0b013e318247ff54.
Mullen SA, Marini C, Suls A, Mei D, Della Giustina E, Buti D, et al. Glucose transporter 1 deficiency as a treatable cause of myoclonic astatic epilepsy. Arch Neurol. 2011;68(9):1152–5. doi:10.1001/archneurol.2011.102.
Akman CI, Engelstad K, Hinton VJ, Ullner P, Koenigsberger D, Leary L, et al. Acute hyperglycemia produces transient improvement in glucose transporter type 1 deficiency. Ann Neurol. 2010;67(1):31–40. doi:10.1002/ana.21797.
Lindgren KA, Larson CL, Schaefer SM, Abercrombie HC, Ward RT, Oakes TR, et al. Thalamic metabolic rate predicts EEG alpha power in healthy control subjects but not in depressed patients. Biol Psychiatry. 1999;45(8):943–52.
Feige B, Scheffler K, Esposito F, Di Salle F, Hennig J, Seifritz E. Cortical and subcortical correlates of electroencephalographic alpha rhythm modulation. J Neurophysiol. 2005;93(5):2864–72. doi:10.1152/jn.00721.2004.
Goldman RI, Stern JM, Engel Jr J, Cohen MS. Simultaneous EEG and fMRI of the alpha rhythm. Neuroreport. 2002;13(18):2487–92. doi:10.1097/01.wnr.0000047685.08940.d0.
Schreckenberger M, Lange-Asschenfeldt C, Lochmann M, Mann K, Siessmeier T, Buchholz HG, et al. The thalamus as the generator and modulator of EEG alpha rhythm: a combined PET/EEG study with lorazepam challenge in humans. Neuroimage. 2004;22(2):637–44. doi:10.1016/j.neuroimage.2004.01.047.
Pascual JM, Van Heertum RL, Wang D, Engelstad K, De Vivo DC. Imaging the metabolic footprint of Glut1 deficiency on the brain. Ann Neurol. 2002;52(4):458–64. doi:10.1002/ana.10311.
Hughes SW, Crunelli V. Thalamic mechanisms of EEG alpha rhythms and their pathological implications. Neuroscientist Rev J Bringing Neurobiol Neurol Psychiatry. 2005;11(4):357–72. doi:10.1177/1073858405277450.
Klepper J, Fischbarg J, Vera JC, Wang D, De Vivo DC. GLUT1-deficiency: barbiturates potentiate haploinsufficiency in vitro. Pediatr Res. 1999;46(6):677–83.
von Moers A, Brockmann K, Wang D, Korenke CG, Huppke P, De Vivo DC, et al. EEG features of glut-1 deficiency syndrome. Epilepsia. 2002;43(8):941–5.
Pons R, Collins A, Rotstein M, Engelstad K, De Vivo DC. The spectrum of movement disorders in Glut-1 deficiency. Mov Disord. 2010;25(3):275–81. doi:10.1002/mds.22808.
Overweg-Plandsoen WC, Groener JE, Wang D, Onkenhout W, Brouwer OF, Bakker HD, et al. GLUT-1 deficiency without epilepsy–an exceptional case. J Inherit Metab Dis. 2003;26(6):559–63.
Friedman JR, Thiele EA, Wang D, Levine KB, Cloherty EK, Pfeifer HH, et al. Atypical GLUT1 deficiency with prominent movement disorder responsive to ketogenic diet. Mov Disord. 2006;21(2):241–5. doi:10.1002/mds.20660.
Perez-Duenas B, Prior C, Ma Q, Fernandez-Alvarez E, Setoain X, Artuch R, et al. Childhood chorea with cerebral hypotrophy: a treatable GLUT1 energy failure syndrome. Arch Neurol. 2009;66(11):1410–4. doi:10.1001/archneurol.2009.236.
Klepper J, Engelbrecht V, Scheffer H, van der Knaap MS, Fiedler A. GLUT1 deficiency with delayed myelination responding to ketogenic diet. Pediatr Neurol. 2007;37(2):130–3. doi:10.1016/j.pediatrneurol.2007.03.009.
Joshi C, Greenberg CR, De Vivo D, Dong W, Chan-Lui W, Booth FA. GLUT1 deficiency without epilepsy: yet another case. J Child Neurol. 2008;23(7):832–4. doi:10.1177/0883073808314896.
Koy A, Assmann B, Klepper J, Mayatepek E. Glucose transporter type 1 deficiency syndrome with carbohydrate-responsive symptoms but without epilepsy. Dev Med Child Neurol. 2011;53(12):1154–6. doi:10.1111/j.1469-8749.2011.04082.x.
Lance JW. Familial paroxysmal dystonic choreoathetosis and its differentiation from related syndromes. Ann Neurol. 1977;2(4):285–93. doi:10.1002/ana.410020405.
Plant GT, Williams AC, Earl CJ, Marsden CD. Familial paroxysmal dystonia induced by exercise. J Neurol Neurosurg Psychiatry. 1984;47(3):275–9.
Nardocci N, Lamperti E, Rumi V, Angelini L. Typical and atypical forms of paroxysmal choreoathetosis. Dev Med Child Neurol. 1989;31(5):670–4.
Bhatia KP, Soland VL, Bhatt MH, Quinn NP, Marsden CD. Paroxysmal exercise-induced dystonia: eight new sporadic cases and a review of the literature. Mov Disord. 1997;12(6):1007–12. doi:10.1002/mds.870120626.
Suls A, Dedeken P, Goffin K, Van Esch H, Dupont P, Cassiman D, et al. Paroxysmal exercise-induced dyskinesia and epilepsy is due to mutations in SLC2A1, encoding the glucose transporter GLUT1. Brain. 2008;131(Pt 7):1831–44. doi:10.1093/brain/awn113.
•• Weber YG, Storch A, Wuttke TV, Brockmann K, Kempfle J, Maljevic S, et al. GLUT1 mutations are a cause of paroxysmal exertion-induced dyskinesias and induce hemolytic anemia by a cation leak. J Clin Invest. 2008;118(6):2157–68. doi:10.1172/JCI34438. The authors identified a SLC2A1 mutation in members of a family with paroxysmal exertional dyskinesia (PED), epilepsy, mild developmental delay, and hemolytic anemia, and demonstrated that a cation leak in the red cell membrane caused by the mutant Glut1 protein was the mechanism underlying the hemolytic anemia. They also identified SLC2A1 mutations in 2 other families with PED and epilepsy.
Bovi T, Fasano A, Juergenson I, Gellera C, Castellotti B, Fontana E, et al. Paroxysmal exercise-induced dyskinesia with self-limiting partial epilepsy: a novel GLUT-1 mutation with benign phenotype. Parkinsonism Relat Disord. 2011;17(6):479–81. doi:10.1016/j.parkreldis.2011.03.015.
Schneider SA, Paisan-Ruiz C, Garcia-Gorostiaga I, Quinn NP, Weber YG, Lerche H, et al. GLUT1 gene mutations cause sporadic paroxysmal exercise-induced dyskinesias. Mov Disord. 2009;24(11):1684–8. doi:10.1002/mds.22507.
Auburger G, Ratzlaff T, Lunkes A, Nelles HW, Leube B, Binkofski F, et al. A gene for autosomal dominant paroxysmal choreoathetosis/spasticity (CSE) maps to the vicinity of a potassium channel gene cluster on chromosome 1p, probably within 2 cM between D1S443 and D1S197. Genomics. 1996;31(1):90–4. doi:10.1006/geno.1996.0013.
Weber YG, Kamm C, Suls A, Kempfle J, Kotschet K, Schule R, et al. Paroxysmal choreoathetosis/spasticity (DYT9) is caused by a GLUT1 defect. Neurology. 2011;77(10):959–64. doi:10.1212/WNL.0b013e31822e0479.
Zorzi G, Castellotti B, Zibordi F, Gellera C, Nardocci N. Paroxysmal movement disorders in GLUT1 deficiency syndrome. Neurology. 2008;71(2):146–8. doi:10.1212/01.wnl.0000316804.10020.ba.
Rotstein M, Doran J, Yang H, Ullner PM, Engelstad K, De Vivo DC. Glut1 deficiency and alternating hemiplegia of childhood. Neurology. 2009;73(23):2042–4. doi:10.1212/WNL.0b013e3181c55ebf.
Urbizu A, Cuenca-Leon E, Raspall-Chaure M, Gratacos M, Conill J, Redecillas S, et al. Paroxysmal exercise-induced dyskinesia, writer's cramp, migraine with aura and absence epilepsy in twin brothers with a novel SLC2A1 missense mutation. J Neurol Sci. 2010;295(1–2):110–3. doi:10.1016/j.jns.2010.05.017.
Ito Y, Oguni H, Ito S, Oguni M, Osawa M. A modified Atkins diet is promising as a treatment for glucose transporter type 1 deficiency syndrome. Dev Med Child Neurol. 2011;53(7):658–63. doi:10.1111/j.1469-8749.2011.03961.x.
Liu Y, Bao X, Wang D, Fu N, Zhang X, Cao G, et al. Allelic variations of Glut-1 deficiency syndrome: the Chinese experience. Pediatr Neurol. 2012;47(1):30–4. doi:10.1016/j.pediatrneurol.2012.04.010.
Klepper J, Scheffer H, Leiendecker B, Gertsen E, Binder S, Leferink M, et al. Seizure control and acceptance of the ketogenic diet in GLUT1 deficiency syndrome: a 2- to 5-year follow-up of 15 children enrolled prospectively. Neuropediatrics. 2005;36(5):302–8. doi:10.1055/s-2005-872843.
Wang D, Pascual JM, Yang H, Engelstad K, Jhung S, Sun RP, et al. Glut-1 deficiency syndrome: clinical, genetic, and therapeutic aspects. Ann Neurol. 2005;57(1):111–8. doi:10.1002/ana.20331.
Pascual JM, Wang D, Hinton V, Engelstad K, Saxena CM, Van Heertum RL, et al. Brain glucose supply and the syndrome of infantile neuroglycopenia. Arch Neurol. 2007;64(4):507–13. doi:10.1001/archneur.64.4.noc60165.
Flatt JF, Guizouarn H, Burton NM, Borgese F, Tomlinson RJ, Forsyth RJ, et al. Stomatin-deficient cryohydrocytosis results from mutations in SLC2A1: a novel form of GLUT1 deficiency syndrome. Blood. 2011;118(19):5267–77. doi:10.1182/blood-2010-12-326645.
Bawazir WM, Gevers EF, Flatt JF, Ang AL, Jacobs B, Oren C, et al. An infant with pseudohyperkalemia, hemolysis, and seizures: cation-leaky GLUT1-deficiency syndrome due to a SLC2A1 mutation. J Clin Endocrinol Metab. 2012;97(6):E987–93. doi:10.1210/jc.2012-1399.
Zheng PP, Romme E, van der Spek PJ, Dirven CM, Willemsen R, Kros JM. Defect of development of ocular vasculature in Glut1/SLC2A1 knockdown in vivo. Cell Cycle. 2011;10(11):1871–2.
Kaufmann P, Shungu DC, Sano MC, Jhung S, Engelstad K, Mitsis E, et al. Cerebral lactic acidosis correlates with neurological impairment in MELAS. Neurology. 2004;62(8):1297–302.
• Levy B, Wang D, Ullner PM, Engelstad K, Yang H, Nahum O, et al. Uncovering microdeletions in patients with severe Glut-1 deficiency syndrome using SNP oligonucleotide microarray analysis. Mol Genet Metab. 2010;100(2):129–35. doi:10.1016/j.ymgme.2010.03.007. The authors describe 7 children with Glut-1 DS caused by microdeletions in the SLC2A1 region, who all had a severe clinical syndrome.
Barros LF, Bittner CX, Loaiza A, Porras OH. A quantitative overview of glucose dynamics in the gliovascular unit. Glia. 2007;55(12):1222–37. doi:10.1002/glia.20375.
Wang D, Pascual JM, Yang H, Engelstad K, Mao X, Cheng J, et al. A mouse model for Glut-1 haploinsufficiency. Hum Mol Genet. 2006;15(7):1169–79. doi:10.1093/hmg/ddl032.
Jensen PJ, Gitlin JD, Carayannopoulos MO. GLUT1 deficiency links nutrient availability and apoptosis during embryonic development. J Biol Chem. 2006;281(19):13382–7. doi:10.1074/jbc.M601881200.
Gramer G, Wolf NI, Vater D, Bast T, Santer R, Kamsteeg EJ, et al. Glucose transporter-1 (GLUT1) deficiency syndrome: diagnosis and treatment in late childhood. Neuropediatrics. 2012;43(3):168–71. doi:10.1055/s-0032-1315433.
De Vivo DC, Bohan TP, Coulter DL, Dreifuss FE, Greenwood RS, Nordli Jr DR, et al. L-carnitine supplementation in childhood epilepsy: current perspectives. Epilepsia. 1998;39(11):1216–25.
Konrad D, Somwar R, Sweeney G, Yaworsky K, Hayashi M, Ramlal T, et al. The antihyperglycemic drug alpha-lipoic acid stimulates glucose uptake via both GLUT4 translocation and GLUT4 activation: potential role of p38 mitogen-activated protein kinase in GLUT4 activation. Diabetes. 2001;50(6):1464–71.
Anheim M, Maillart E, Vuillaumier-Barrot S, Flamand-Rouviere C, Pineau F, Ewenczyk C, et al. Excellent response to acetazolamide in a case of paroxysmal dyskinesias due to GLUT1-deficiency. J Neurol. 2011;258(2):316–7. doi:10.1007/s00415-010-5702-5.
Acknowledgments
The authors are grateful for the support of the Colleen Giblin Foundation, the Will Foundation, Milestones for Children, and USPHS grant 5R01NS37949 (NINDS, dcd).
Disclosure
Toni S. Pearson declares no conflict of interest. Cigdem Akman declares no conflict of interest. Veronica J. Hinton declares no conflict of interest. Kristin Engelstad declares no conflict of interest. Darryl C. De Vivo declares no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Pediatric Neurology
Rights and permissions
About this article
Cite this article
Pearson, T.S., Akman, C., Hinton, V.J. et al. Phenotypic Spectrum of Glucose Transporter Type 1 Deficiency Syndrome (Glut1 DS). Curr Neurol Neurosci Rep 13, 342 (2013). https://doi.org/10.1007/s11910-013-0342-7
Published:
DOI: https://doi.org/10.1007/s11910-013-0342-7