Abstract
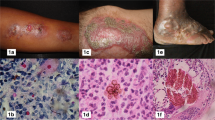
Subcutaneous mycoses are common in tropical and subtropical regions of the world. These infections have multiple features in common, including similar epidemiology, mode of transmission, indolent chronic presentation with low potential for dissemination in immunocompetent hosts, and pyogranulomatous lesions on histopathology. Herein, we provide up-to-date epidemiologic, clinical, diagnostic, and therapeutic data for three important subcutaneous mycoses: chromoblastomycosis, mycetoma, and sporotrichosis.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Baddley JW, Dismukes WE. Chromoblastomycosis. In: Kauffman CA, Pappas PG, Sobel JD, Dismukes WE, editors. Essentials of clinical mycology. New York: Springer Press; 2011. p. 427–33. Exhaustive review of chromoblastomycosis.
Ameen M. Chromoblastomycosis: clinical presentation and management. Clin Exp Dermatol. 2009;34(8):849–54.
Howles JK, Kennedy CB, Carvin WH, et al. Chromoblastomycosis: report of nine cases from a single area in Louisiana. Arch Dermatol Syphilol. 1954;69:83–90.
Gardner JT, et al. Chromoblastomycosis in Texas: Report of four cases. Tex State J Med. 1964;60:913–7.
Silva JP, de Souza W, Rozental S. Chromoblastomycosis: a retrospective study of 325 cases on Amazonic Region (Brazil). Mycopathologia. 1998-1999;143(3):171–5.
Minotto R, Verajao Bernardi CD, Mallmann, et al. Chromoblastomycosis: a review of 100 cases in the state of Rio Grande do Sul, Brazil. J Am Acad Dermatol. 2001;44:585–92.
Correia RT, Valente NY, Criado PR, et al. Chromoblastomycosis: study of 27 cases and review of medical literature. An Bras Dermatol. 2010;85(4):448–54.
Pretelt Mendoza J.: Cromomicosis. Aspectos epidemiolgicos. Analisis de 82 casos estudiados en el Centro Dermatologico “Ladislao de la Pascua” de 1956-1988. Dermatology Specialty Thesis, Universidad Nacional Autonoma de Mexico, 1989.
Bonifaz A, Carrasco-Gerard E, Saúl A. Chromoblastomycosis: clinical and mycologic experience of 51 cases. Mycoses. 2001;44:1–7.
Esterre P, Andriantsimahavandy A, et al. Forty years of chromoblastomycosis in Madagascar: a review. Am J Trop Med Hyg. 1996;55:45–7.
López Martínez R, Méndez Tovar LJ. Chromoblastomycosis. Clin Dermatol. 2007;25(2):188–94.
Guedes Salgado C, Pereirada Silva J, Picanco Diniz JA, et al. Isolation of Fonsecaea pedrosoi from thorns of Mimosa pudica, a probable natural source of chromoblastomycosis. Rev Inst Med Trop Sao Paulo. 2004;46:33–6.
Cardona-Castro N, Agudelo-Flórez P. Development of a chronic chromoblastomycosis model in immunocompetent mice. Med Mycol. 1999;37(2):81–3.
Santos AL, Palmeira VF, Rozental S, et al. Biology and pathogenesis of Fonsecaea pedrosoi, the major etiologic agent of chromoblastomycosis. FEMS Microbiol Rev. 2007;31(5):570–91.
•• Salgado CG. Fungal x host interactions in Chromoblastomycosis: what we have learned from animal models and what is yet to be solved. Virulence. 2010;1(1):3–5. This review article summarizes our current understanding of the immune response against chromoblastomycosis derived from animal models.
•• Sousa MdaG, Reid DM, Schweighoffer E, et al. Restoration of pattern recognition receptor costimulation to treat chromoblastomycosis, a chronic fungal infection of the skin. Cell Host Microbe. 2011;9(5):436–43. Original article that underscores the importance of the innate immune response, pattern recognizition receptors and their potential therapeutic applications.
Rozental S, Alviano CS, de Souza W. The in vitro susceptibility of Fonsecaea pedrosoi to activated macrophages. Mycopathologia. 1994;126:85–91.
Ahrens J, Graybill JR, Abishawl A, et al. Experimental murine chromomycosis mimicking chronic progressive human disease. Am J Trop Med Hyg. 1989;40(6):651–8.
de Sousa Teixeira MG, Ghosn EE, Almeida SR. Absence of CD4+ T cells impairs host defence of mice infected with Fonsecaea pedrosoi. Scand J Immunol. 2006;64:595–600.
Gimenes VMF, Sousa MG, et al. Cytokine and lymphocyte proliferation in patients with different clinical forms of chromoblasto-mycosis. Microbes Infect. 2005;7:708–13.
Queiroz-Telles F, Esterre P, Perez-Blanco M, et al. Chromoblastomycosis: an overview of clinical manifestations, diagnosis and treatment. Med Mycol. 2009;47:3–15.
McGinnis MR. Chromoblastomycosis and phaeohyphomycosis: new concepts, diagnosis and mycology. J Am Acad Dermatol. 1983;8:1–16.
Ogawa MM, Alchorne MM, Barbieri A, et al. Lymphoscintigraphic analysis in chromoblastomycosis. Int J Dermatol. 2003;42:622–5.
Fukushiro R. Chromomycosis in Japan. Int J Dermatol. 1983;22:221–9.
Takase T, Baba T, Ueno K. Chromomycosis. A case with a widespread rash, lymph node metastasis and multiple subcutaneous nodules. Mycoses. 1988;31:343–52.
Wackym PA. Cutaneous chromomycosis in renal transplant recipients. Arch Intern Med. 1985;145:1036–7.
Carrion A. Chromoblastomycosis. Ann NY Acad Sci. 1950;50:1255–81.
Abliz P, Fukushima K, Takizawa K, et al. Specific oligonucleotide primers for identification of Cladophialophora carrionii, a causative agent of chromoblastomycosis. J Clin Microbiol. 2004;42(1):404–7.
de Andrade TS, Cury AE, de Castro LG, et al. Rapid identification of Fonsecaea by duplex polymerase chain reaction in isolates from patients with chromoblastomycosis. Diagn Microbiol Infect Dis. 2007;57(3):267–72.
Abliz P, Fukushima K, Takizawa K, et al. Rapid identification of the genus fonsecaea by PCR with specific oligonucleotide primers. J Clin Microbiol. 2003;41(2):873–6.
Bonifaz A, Paredes-Solis V, Saul A. Treating chromoblastomycosis with systemic antifungals. Expert Opin Pharmacother. 2004;5:247–54.
Ameen M. Managing Chromoblastomycosis. Trop Doct. 2010;40(2):65–7.
Esterre P, Queiroz-Telles F. Management of chromoblastomycosis: novel perspectives. Curr Opin Infect Dis. 2006;19(2):148–52.
Vitale RG, Perez-Blanco M, De Hoog GS. In vitro activity of antifungal drugs against Cladophialophora species associated with human chromoblastomycosis. Med Mycol. 2009;47(1):35–40.
Caligiorne RB, Resende MA, Melillo PH, et al. In vitro susceptibility of chromoblastomycosis and phaeohyphomycosis agents to antifungal drugs. Med Mycol. 1999;37(6):405–9.
Gupta AK, Taborda PR, Sanzovo AD. Alternate week and combination itraconazole and terbinafine therapy for chromoblastomycosis caused by Fonsecaea pedrosoi in Brazil. Med Mycol. 2002;40:529–34.
• Bustamante B, Campos PE. Eumycetoma. In: Kauffman CA, Pappas PG, Sobel JD, Dismukes WE, editors. Essentials of clinical mycology. 2nd ed. New York: Springer Press; 2011. p. 415–25. Extensive review of Eumycetoma.
Hospenthal DR. Agents of mycetoma. In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 7th ed. Philadelphia: Churchill Livingstone; 2009. p. 3281–5.
Green Jr WO, Adams TE. Mycetoma in the United States: a review and report of seven additional cases. Am J Clin Pathol. 1964;42:75–91.
Bendl BJ, Mackey D, Al-Saati F, et al. Mycetoma in Saudi Arabia. J Trop Med Hyg. 1987;90(2):51–9.
Develoux M, Audoin J, Treguer J, et al. Mycetoma in the Republic of Niger: clinical features and epidemiology. Am J Trop Med Hyg. 1988;38(2):386–90.
Castro LG, Belda Júnior W, Salebian A, et al. Mycetoma: a retrospective study of 41 cases seen in São Paulo, Brazil, from 1978 to 1989. Mycoses. 1993;36(3–4):89–95.
Khatri ML, Al-Halali HM, Fouad Khalid M, et al. Mycetoma in Yemen: clinicoepidemiologic and histopathologic study. Int J Dermatol. 2002;41(9):586–93.
Dieng MT, Sy MH, Diop BM, et al. Mycetoma: 130 cases. Ann Dermatol Venereol. 2003;130(1 Pt 1):16–9.
Bakshi R, Mathur DR. Incidence and changing pattern of mycetoma in western Rajasthan. Indian J Pathol Microbiol. 2008;51(1):154–5.
Castro LG, Piquero-Casals J. Clinical and mycologic findings and therapeutic outcome of 27 mycetoma patients from São Paulo, Brazil. Int J Dermatol. 2008;47(2):160–3.
Padhi S, Uppin SG, Uppin MS, et al. Mycetoma in South India: retrospective analysis of 13 cases and description of two cases caused by unusual pathogens: Neoscytalidium dimidiatum and Aspergillus flavus. Int J Dermatol. 2010;49(11):1289–96.
Ahmed AO, van Leeuwen W, Fahal A, et al. Mycetoma caused by Madurella mycetomatis: a neglected infectious burden. Lancet Infect Dis. 2004;4(9):566–74.
van de Sande WW, Gorkink R, Simons G, et al. Genotyping of Madurella mycetomatis by selective amplification of restriction fragments (amplified fragment length polymorphism) and subtype correlation with geographical origin and lesion size. J Clin Microbiol. 2005;43(9):4349–56.
van de Sande WW, Janse DJ, Hira V, Goedhart H, et al. Translationally controlled tumor protein from Madurella mycetomatis, a marker for tumorous mycetoma progression. J Immunol. 2006;177(3):1997–2005.
Mahgoub ES, Gumaa SA, El Hassan AM. Immunological status of mycetoma patients. Bull Soc Pathol Exot Filiales. 1977;70(1):48–54.
Fahal AH, Sadig ME, Suliman SH, et al. Lack of association between ABO blood groups and Rh factor and the tendency to develop mycetoma. East Afr Med J. 1996;73(11):771.
Fahal AH, el Toum EA, el Hassan AM, et al. The host tissue reaction to Madurella mycetomatis: new classification. J Med Vet Mycol. 1995;33:15.
van de Sande WW, Fahal A, Verbrugh H, van Belkum A. Polymorphisms in genes involved in innate immunity predispose toward mycetoma susceptibility. J Immunol. 2007;179:3065.
Ameen M, Arenas R. Emerging therapeutic regimes for the management of mycetomas. Expert Opin Pharmacother. 2008;9(12):2077–85.
El Hag IA, Fahal AH, Gasim ET. Fine needle aspiration cytology of mycetoma. Acta Cytol. 1996;40(3):461–4.
Gabhane SK, Gangane N, Anshu A. Cytodiagnosis of eumycotic mycetoma: a case report. Acta Cytol. 2008;52(3):354–6.
Afroz N, Khan N, Siddiqui FA, et al. Eumycetoma versus actinomycetoma: Diagnosis on cytology. J Cytol. 2010;27(4):133–5.
Hemalata M, Prasad S, Venkatesh K, et al. Cytological diagnosis of actinomycosis and eumycetoma: a report of two cases. Diagn Cytopathol. 2010;38(12):918–20.
• Yousif BM, Fahal AH, Shakir MY. A new technique for the diagnosis of mycetoma using fixed blocks of aspirated material. Trans R Soc Trop Med Hyg. 2010;104(1):6–9. This article in together with the two previous references highlight new diagnostic methods for eumycetoma.
Ahmed AO, Mukhtar MM, Kools-Sijmons M, et al. Development of a species-specific PCR-restriction fragment length polymorphism analysis procedure for identification of Madurella mycetomatis. J Clin Microbiol. 1999;37(10):3175–8.
Desnos-Ollivier M, Bretagne S, Dromer F, et al. Molecular identification of black-grain mycetoma agents. J Clin Microbiol. 2006;44(10):3517–23.
Czechowski J, Nork M, Haas D, et al. MR and other imaging methods in the investigation of mycetomas. Acta Radiol. 2001;42:24.
Sharif HS, Clark DC, Aabed MY, et al. Mycetoma: comparison of MR imaging with CT. Radiology. 1991;178:865.
Welsh O, Salinas MC, Rodríguez MA. Treatment of eumycetoma and actinomycetoma. Curr Top Med Mycol. 1995;6:47.
Mahgoub ES, Gumaa SA. Ketoconazole in the treatment of eumycetoma due to Madurella mycetomii. Trans R Soc Trop Med Hyg. 1984;78:376.
Venugopal PV, Venugopal TV, Ramakrishna ES, Ilavarasi S. Antimycotic susceptibility testing of agents of black grain eumycetoma. J Med Vet Mycol. 1993;31:161.
Smith EL, Kutbi S. Improvement of eumycetoma with itraconazole. J Am Acad Dermatol. 1997;34:279–80.
•• Fahal AH, Rahman IA, El-Hassan AM, et al. The safety and efficacy of itraconazole for the treatment of patients with eumycetoma due to Madurella mycetomatis. Trans R Soc Trop Med Hyg. 2011;105(3):127–32. Small prospective study, evaluating the safety and efficacy of itraconazole for the treatment of M. mycetomatis eumycetoma.
Restrepo A. Treatment of tropical mycoses. J Am Acad Dermatol. 1994;31(3 Pt 2):S91–S102.
•• van Belkum A, Fahal AH, van de Sande WW. In vitro susceptibility of Madurella mycetomatis to posaconazole and terbinafine. Antimicrob Agents Chemother. 2011;55(4):1771–3. First to describe the in vitro susceptibility of M. mycetomatis to posaconazole and terbinafine using 24 clinical isolates.
Negroni R, Tobon A, Bustamante B, et al. Posaconazole treatment of refractory eumycetoma and chromoblastomycosis. Rev Inst Med Trop Sao Paulo. 2005;47(6):339–46.
Difonzo EM, Massi D, Vanzi L, et al. Madurella mycetomatis mycetoma treated successfully with oral posaconazole. J Chemother. 2011;23(4):243–4.
Lacroix C, De Kerviler E, Morel P, et al. Madurella mycetomatis mycetoma treated successfully with oral voriconazole. Br J Dermatol. 2005;152:1067–8.
Loulergue P, Hot A, Dannaoui E, et al. Successful treatment of black-grain mycetoma with voriconazole. Am J Trop Med Hyg. 2006;75(6):1106–7.
N'diaye B, Dieng MT, Perez A, et al. Clinical efficacy and safety of oral terbinafine in fungal mycetoma. Int J Dermatol. 2006;45(2):154–7.
•• van de Sande WW, Fahal AH, Bakker-Woudenberg IA, et al. Madurella mycetomatis is not susceptible to the echinocandin class of antifungal agents. Antimicrob Agents Chemother. 2010;54(6):2738–40. Original study showing the lack of in-vitro activity of the echinocandins against M. mycetomatis.
Porte L, Khatibi S, Hajj LE, et al. Scedosporium apiospermum mycetoma with bone involvement successfully treated with voriconazole. Trans R Soc Trop Med Hyg. 2006;100(9):891–4.
McGinnis MR, Pasarell L. In vitro testing of susceptibilities of filamentous ascomycetes to voriconazole, itraconazole, and amphotericin B, with consideration of phylogenetic implications. J Clin Microbiol. 1998;36(8):2353.
Troke P, Aguirrebengoa K, Arteaga C, et al. Treatment of scedosporiosis with voriconazole: clinical experience with 107 patients. Antimicrob Agents Chemother. 2008;52(5):1743.
Schaenman JM, DiGiulio DB, Mirels LF, et al. Scedosporium apiospermum soft tissue infection successfully treated with voriconazole: potential pitfalls in the transition from intravenous to oral therapy. J Clin Microbiol. 2005;43(2):973–7.
Matsumoto Y, Oh-I T, Nagai A, et al. Case of cutaneous Scedosporium apiospermum infection successfully treated with voriconazole. J Dermatol. 2009;36(2):98–102.
•• Pappas PG. Sporotrichosis. In: Kauffman CA, Pappas PG, Sobel JD, Dismukes WE, editors. Essentials of clinical mycology. 2nd ed. New York: Springer Press; 2011. p. 387–97. Detailed review on S. schenckii, infection, clinical manifestations, diagnosis and treatment.
• López-Romero E, Reyes-Montes MdelR, Pérez-Torres A, et al. Sporothrix schenckii complex and sporotrichosis, an emerging health problem. Future Microbiol. 2011;6(1):85–102. Thorough review of sporotrichosis, with a particular focus of the biology of S. schenkii.
Marimon R, Gené J, Cano J, et al. Molecular phylogeny of Sporothrix schenckii. J Clin Microbiol. 2006;44(9):3251–6.
Marimon R, Cano J, Gené J, et al. Sporothrix brasiliensis, S. globosa, and S. mexicana, three new Sporothrix species of clinical interest. J Clin Microbiol. 2007;45(10):3198–206.
D’Alessio DJ, Leavens LJ, Strumpf GB, Smith CD. An outbreak of sporotrichosis in Vermont associated with sphagnum moss as the source of infection. N Engl J Med. 1965;272:1054–8.
Powell KE, Taylor A, Phillips BJ, et al. Cutaneous sporotrichosis in forestry workers: epidemic due to contaminated sphagnum moss. JAMA. 1978;240:232–5.
Centers for Disease Control. Sporotrichosis associated with Wisconsin sphagnum moss. MMWR. 1982;31:542–4.
Itoh M, Okamoto S, Kariya H. Survey of 200 cases of sporotrichosis. Dermatologica. 1986;172:209–13.
Dixon DM, Salkin IF, Duncan RA, et al. Isolation and characterization of Sporothrix schenckii from clinical and environmental sources associated with the largest US epidemic of sporotrichosis. J Clin Microbiol. 1991;29:1106–13.
Coles FB, Schuchat A, Hibbs JR, et al. A multistate outbreak of sporotrichosis associated with sphagnum moss. Am J Epidemiol. 1992;136:475–87.
Hajjeh R, McDonnell S, Reef S, et al. Outbreak of sporotrichosis among tree nursery workers. J Infect Dis. 1997;176:499–504.
Dooley DP, Bostic PS, Beckius ML. Spook house sporotrichosis. A point-source outbreak of cutaneous sporotrichosis from hay bale props in a Halloween haunted-house. Arch Intern Med. 1997;157:1885–7.
Barros MB, Schubach AO, Schubach TM, Wanke B, Lambert-Passos SR. An epidemic of sporotrichosis in Rio de Janeiro, Brazil: epidemiological aspects of a series of cases. Epidemiol Infect. 2008;136:1192–6.
Schubach A, Barros MB, Wanke B. Epidemic sporotrichosis. Curr Opin Infect Dis. 2008;21(2):129–33.
•• Madrid IM, Mattei A, Martins A, et al. Feline sporotrichosis in the southern region of rio grande do sul, Brazil: clinical, zoonotic and therapeutic aspects. Zoonoses Public Health. 2010;57(2):151–4. Original article addressing the epidemic of sporotrichosis in Brazil derived from zoonotic transmission of the disease from cats.
• Rees RK, Swartzberg JE. Feline-transmitted sporotrichosis: A case study from California. Dermatol Online J. 2011;17(6):2. Report of zoonotic transmission of sporotrichosis in the United States.
Pluss JL, Opal SM. Pulmonary sporotrichosis: review of treatment and outcome. Medicine (Baltimore). 1986;65(3):143–53.
Pappas PG, Tellez I, Deep AE, et al. Sporotrichosis in Peru: description of an area of hyperendemicity. Clin Inf Dis. 2000;20:65–70.
Fukushiro R. Epidemiology and ecology of sporotrichosis in Japan. Zbl Bakt Hyg A. 1984;257:228–33.
Ramos-e-Silva M, Vasconcelos C, Carneiro S, et al. Sporotrichosis. Clin Dermatol. 2007;25(2):181–7.
Smego Jr RA, Castiglia M, Asperilla MO. Lymphocutaneous syndrome. A review of non-sporothrix causes. Medicine (Baltimore). 1999;78(1):38–63.
Mahlberg MJ, Patel R, Rosenman K, et al. Fixed cutaneous sporotrichosis. Dermatol Online J. 2009;15(8):5.
Kauffman CA. Sporotrichosis. Clin Infect Dis. 1999 Aug;29(2):231–6.
Yacobucci GN, Santilli MD. Sporotrichosis of the knee. A case report. Orthopedics 9:387–90
Yao J, Penn RG, Ray S. Articular sporotrichosis. Clin Orthop. 1986;204:207–14.
Appenzeller S, Amaral TN, Amstalden EMI, et al. Sporothrix schenckii infection presented as monoarthritis: report of two cases and review of the literature. Clin Rheumatol. 2006;25:926–8.
Chowdhary G, Weinstein A, Klein R, Mascarenhas BR. Sporotrichal arthritis. Ann Rheum Dis. 1991;50:112–4.
Atdjian M, Granda JL, Ingberg HO, et al. Systemic sporotrichosis polytenosynovitis with median and ulnar nerve entrapment. JAMA. 1980;243:1841–2.
Stratton CW, Lichtenstein KA, Lowenstein SR, Phelps DB, Reller LB. Granulomatous tenosynovitis and carpal tunnel syndrome caused by Sporothrix schenckii. Am J Med. 1981;71:161–4.
Schwartz DA. Sporothrix tenosynovitis – differential diagnosis of granulomatous inflammatory disease of the joints. J Rheumatol. 1989;16:550–3.
Witherspoon CD, Kuhn F, Owens SD, et al. Endophthalmitis due to Sporothrix schenckii after penetrating ocular injury. Ann Ophthalmol. 1990 Oct;22(10):385–8.
Curi AL, Félix S, Azevedo KM, Estrela R, et al. Retinal granuloma caused by Sporothrix schenckii. Am J Ophthalmol. 2003;136(1):205–7.
Schubach A, de Lima Barros MB, Schubach TM, et al. Primary conjunctival sporotrichosis: two cases from a zoonotic epidemic in Rio de Janeiro, Brazil. Cornea. 2005;24(4):491–3. Review.
Kashima T, Honma R, Kishi S, et al. Bulbar conjunctival sporotrichosis presenting as a salmon-pink tumor. Cornea. 2010;29(5):573–6.
Iyengar SS, Khan JA, Brusco M, et al. Cutaneous Sporothrix schenckii of the human eyelid. Ophthal Plast Reconstr Surg. 2010;26(4):305–6.
Heller HM, Fuhrer J. Disseminated sporotrichosis in patients with AIDS: case report and review of the literature. AIDS. 1991 Oct;5(10):1243–6.
al-Tawfiq JA, Wools KK. Disseminated sporotrichosis and Sporothrix schenckii fungemia as the initial presentation of human immunodeficiency virus infection. Clin Infect Dis. 1998;26(6):1403–6.
Yelverton CB, Stetson CL, Bang RH, et al. Fatal sporotrichosis. Cutis. 2006 Oct;78(4):253–6.
Zhang YQ, Xu XG, Zhang M, et al. Sporotrichosis: clinical and histopathological manifestations. Am J Dermatopathol. 2011;33(3):296–302.
•• Assi M, Lakkis IE, Wheat LJ. Cross-reactivity in the Histoplasma antigen enzyme immunoassay caused by sporotrichosis. Clin Vaccine Immunol. 2011;18(10):1781–2. Report of a case of false positive Histoplasma antigen enzyme immunoassay in a patient with pulmonary sporotrichosis.
Kauffman CA, Bustamante B, Chapman SW, et al. Clinical practice guidelines for the management of sporotrichosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007;45(10):1255–65.
Restrepo A, Robledo J, Gomez I, Tabares AM, Gutierrez R. Itraconazole therapy in lymphangitic and cutaneous sporotrichosis. Arch Dermatol. 1986;122:413–7.
Conti Diaz IA, Civila E, Gezuele E, et al. Treatment of human cutaneous sporotrichosis with itraconazole. Mycoses. 1992;35:153–6.
Sharkey-Mathis PK, Kauffman CA, Graybill JR, et al. Treatment of sporotrichosis with itraconazole. NIAID Mycoses Study Group. Am J Med. 1993;95:279–85.
•• de Lima Barros MB, Schubach AO, de Vasconcellos Carvalhaes de Oliveira R, et al. Treatment of cutaneous sporotrichosis with itraconazole–study of 645 patients. Clin Infect Dis. 2011;52(12):e200–6. Large prospective study evaluating the safety and efficacy of itraconazole, most of the patients in the study received itraconazole 100 mg daily with excellent results.
•• Song Y, Zhong SX, Yao L, et al. Efficacy and safety of itraconazole pulses vs. continuous regimen in cutaneous sporotrichosis. J Eur Acad Dermatol Venereol. 2011;25(3):302–5. Small-randomized trial comparing itraconazole pulses vs. continuous regimen in cutaneous sporotrichosis.
Chapman SW, Pappas P, Kauffman C, et al. Comparative evaluation of the efficacy and safety of two doses of terbinafine (500 and 1000 mg day) in the treatment of cutaneous or lymphocutaneous sporotrichosis. Mycoses. 2004;47:62–8.
•• Yamada K, Zaitz C, Framil VM, et al. Cutaneous sporotrichosis treatment with potassium iodide: a 24 year experience in São Paulo State, Brazil. Rev Inst Med Trop Sao Paulo. 2011;53(2):89–93. A retrospective analysis evaluating the safety and efficacy of potassium iodine in the treatment of cutaneous sporotrichosis.
•• Xue S, Gu R, Wu T, et al. Oral potassium iodide for the treatment of sporotrichosis. Cochrane Database Syst Rev. 2009 Oct 7;(4):CD006136. A cochrane review of the evidence of potassium iodine for the treatment of sporotrichosis.
Francesconi G, Valle AC, Passos S, et al. Terbinafine (250 mg/day): an effective and safe treatment of cutaneous sporotrichosis. J Eur Acad Dermatol Venereol. 2009;23(11):1273–6.
•• Francesconi G, Francesconi do Valle AC, et al. Comparative study of 250 mg/day terbinafine and 100 mg/day itraconazole for the treatment of cutaneous sporotrichosis. Mycopathologia. 2011;171(5):349–54. This study combined with the prior reference suggest that terbinafine 250 mg is an effective option for the treatment of sporotrichosis.
McGinnis MR, Nordoff N, Li RK, et al. Sporothrix schenckii sensitivity to voriconazole, itraconazole and amphotericin B. Med Mycol. 2001;39(4):369–71.
Disclosure
J. Baddley has been a consultant for Merck, Abbott, and Pfizer. His institution has received grant support from Pfizer. R. La Hoz reported no potential conflicts of interest relevant to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
La Hoz, R.M., Baddley, J.W. Subcutaneous Fungal Infections. Curr Infect Dis Rep 14, 530–539 (2012). https://doi.org/10.1007/s11908-012-0275-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11908-012-0275-3
Keywords
- Subcutaneous mycoses
- Chromoblastomycosis
- Fonsecaea pedrosoi
- Fonsecaea
- Cladophialophora carrionii
- Cladophialophora
- Phialophora
- Eumycetoma
- Madurella mycetomatis
- Leptosphaeria senegalensis
- Madurella grisea
- Pseudallescheria boydii
- Scedosporium apiospermum
- Sporotrichosis
- Sporothrix schenckii species complex
- Nodular lymphangitis