Abstract
Aldosterone antagonists have been highly successful in treating congestive heart failure and resistant hypertension. Until recently, therapies targeting the mineralocorticoid receptor in chronic kidney disease (CKD) have received little attention, largely because of the risk of hyperkalemia and the incorrect assumption that traditional therapy with angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, or both consistently reduces activity of the renin-angiotensin system in all patients. Control of extracellular volume and low-dose mineralocorticoid receptor blocker therapy may offer additional antihypertensive and anti-inflammatory benefits in select CKD populations.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Bomback AS, Klemmer PJ. The incidence and implications of aldosterone breakthrough. Nat Clin Pract Nephrol. 2007;3:486–92.
Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. 1999;341:709–17.
Pitt B, Remme W, Zannad F, Neaton J, Martinez F, Roniker B, et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med. 2003;348:1309–21.
Oliver WJ, Cohen EL, Neel JV. Blood pressure, sodium intake, and sodium related hormones in the Yanomamo Indians, a “no-salt” culture. Circulation. 1975;52:146–51.
Brunner HR, Laragh JH, Baer L, Newton MA, Goodwin FT, Krakoff LR, et al. Essential hypertension: renin and aldosterone, heart attack and stroke. N Engl J Med. 1972;286:441–9.
• Bomback AS, Kshirsagar AV, Ferris ME, Klemmer PJ: Disordered aldosterone-volume relationship in end-stage kidney disease. J Renin Angiotensin Aldosterone Syst 2009, 10:230–236. The results of this pilot study suggest that hemodialysis patients are unable to suppress their aldosterone appropriately in response to volume expansion (i.e., a state of relative hyperaldosteronism).
Krug AW, Ehrhart-Bornstein M. Aldosterone and metabolic syndrome: is increased aldosterone in metabolic syndrome patients an additional risk factor? Hypertension. 2008;51:1252–8.
Whaley-Connell A, Johnson MS, Sowers JR. Aldosterone: role in the cardiometabolic syndrome and resistant hypertension. Prog Cardiovasc Dis. 2010;52:401–9.
Sowers JR, Whaley-Connell A, Epstein M. Narrative review: the emerging clinical implications of the role of aldosterone in the metabolic syndrome and resistant hypertension. Ann Intern Med. 2009;150:776–83.
Schrier RW, Masoumi A, Elhassan E. Aldosterone: role in edematous disorders, hypertension, chronic renal failure, and metabolic syndrome. Clin J Am Soc Nephrol. 2010;5:1132–40.
Wehling M, Christ M, Theisen K. Membrane receptors for aldosterone: a novel pathway for mineralocorticoid action. Am J Physiol. 1992;263:E974–9.
Sato A, Saruta T. Aldosterone-induced organ damage: plasma aldosterone level and inappropriate salt status. Hypertens Res. 2004;27:303–10.
Selye H, Hall C. Pathologic changes induced in various species by overdosage with desoxycorticosterone. Arch Pathol. 1943;36:19–31.
Quinkler M, Zehnder D, Eardley KS, Lepenies J, Howie AJ, Hughes SV, et al. Increased expression of mineralocorticoid effector mechanisms in kidney biopsies of patients with heavy proteinuria. Circulation. 2005;112:1435–43.
Greene EL, Kren S, Hostetter TH. Role of aldosterone in the remnant kidney model in the rat. J Clin Invest. 1996;98:1063–8.
Krikken JA, Laverman GD, Navis G. Benefits of dietary sodium restriction in the management of chronic kidney disease. Curr Opin Nephrol Hypertens. 2009;18:531–8.
• Vogt L, Waanders F, Boomsma F, De ZD, Navis G: Effects of dietary sodium and hydrochlorothiazide on the antiproteinuric efficacy of losartan. J Am Soc Nephrol 2008, 19:999–1007. In this crossover study, reduction of ECV (via diuretics and/or salt restriction) enhances the antiproteinuric effect of RAAS blockade.
Pimenta E, Gaddam KK, Pratt-Ubunama MN, Nishizaka MK, Aban I, Oparil S, et al. Relation of dietary salt and aldosterone to urinary protein excretion in subjects with resistant hypertension. Hypertension. 2008;51:339–44.
Vasavada N, Agarwal R. Role of excess volume in the pathophysiology of hypertension in chronic kidney disease. Kidney Int. 2003;64:1772–9.
Mathie A, Cull-Candy SG, Colquhoun D. Single-channel and whole-cell currents evoked by acetylcholine in dissociated sympathetic neurons of the rat. Proc R Soc Lond B Biol Sci. 1987;232:239–48.
Tattersall J. Bioimpedance analysis in dialysis: state of the art and what we can expect. Blood Purif. 2009;27:70–4.
Wabel P, Chamney P, Moissl U, Jirka T. Importance of whole-body bioimpedance spectroscopy for the management of fluid balance. Blood Purif. 2009;27:75–80.
Lifton RP, Gharavi AG, Geller DS. Molecular mechanisms of human hypertension. Cell. 2001;104:545–56.
Milliez P, Girerd X, Plouin PF, Blacher J, Safar ME, Mourad JJ. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol. 2005;45:1243–8.
• Gaddam KK, Nishizaka MK, Pratt-Ubunama MN, Pimenta E, Aban I, Oparil S, Calhoun DA: Characterization of resistant hypertension: association between resistant hypertension, aldosterone, and persistent intravascular volume expansion. Arch Intern Med 2008, 168:1159–1164. This study documents the importance of a disordered aldosterone-ECV relationship in patients with resistant hypertension.
Pimenta E, Calhoun DA, Oparil S. Sleep apnea, aldosterone, and resistant hypertension. Prog Cardiovasc Dis. 2009;51:371–80.
Visser FW, Krikken JA, Muntinga JH, Dierckx RA, Navis GJ. Rise in extracellular fluid volume during high sodium depends on BMI in healthy men. Obesity (Silver Spring). 2009;17:1684–8.
Kidambi S, Kotchen JM, Grim CE, Raff H, Mao J, Singh RJ, et al. Association of adrenal steroids with hypertension and the metabolic syndrome in blacks. Hypertension. 2007;49:704–11.
Kidambi S, Kotchen JM, Krishnaswami S, Grim CE, Kotchen TA. Aldosterone contributes to blood pressure variance and to likelihood of hypertension in normal-weight and overweight African Americans. Am J Hypertens. 2009;22:1303–8.
Doi M, Takahashi Y, Komatsu R, Yamazaki F, Yamada H, Haraguchi S, et al. Salt-sensitive hypertension in circadian clock-deficient Cry-null mice involves dysregulated adrenal Hsd3b6. Nat Med. 2010;16:67–74.
Hene RJ, Boer P, Koomans HA, Mees EJ. Plasma aldosterone concentrations in chronic renal disease. Kidney Int. 1982;21:98–101.
Gross E, Rothstein M, Dombek S, Juknis HI. Effect of spironolactone on blood pressure and the renin-angiotensin-aldosterone system in oligo-anuric hemodialysis patients. Am J Kidney Dis. 2005;46:94–101.
Goodfriend TL, Calhoun DA. Resistant hypertension, obesity, sleep apnea, and aldosterone: theory and therapy. Hypertension. 2004;43:518–24.
Nagase M, Yoshida S, Shibata S, Nagase T, Gotoda T, Ando K, et al. Enhanced aldosterone signaling in the early nephropathy of rats with metabolic syndrome: possible contribution of fat-derived factors. J Am Soc Nephrol. 2006;17:3438–46.
Rocha R, Stier Jr CT, Kifor I, Ochoa-Maya MR, Rennke HG, Williams GH, et al. Aldosterone: a mediator of myocardial necrosis and renal arteriopathy. Endocrinology. 2000;141:3871–8.
Zoccali C, Bode-Boger S, Mallamaci F, Benedetto F, Tripepi G, Malatino L, et al. Plasma concentration of asymmetrical dimethylarginine and mortality in patients with end-stage renal disease: a prospective study. Lancet. 2001;358:2113–7.
Bomback AS, Kshirsagar AV, Amamoo MA, Klemmer PJ. Change in proteinuria after adding aldosterone blockers to ACE inhibitors or angiotensin receptor blockers in CKD: a systematic review. Am J Kidney Dis. 2008;51:199–211.
• Navaneethan SD, Nigwekar SU, Sehgal AR, Strippoli GF: Aldosterone antagonists for preventing the progression of chronic kidney disease: a systematic review and meta-analysis. Clin J Am Soc Nephrol 2009, 4:542–551. This is one of two systematic reviews on the use of aldosterone blockade in CKD. In nearly all studies, spironolactone or eplerenone was added to ACE inhibitor or ARB therapy with relatively low risk of hyperkalemia.
Mehdi UF, Adams-Huet B, Raskin P, Vega GL, Toto RD. Addition of angiotensin receptor blockade or mineralocorticoid antagonism to maximal angiotensin-converting enzyme inhibition in diabetic nephropathy. J Am Soc Nephrol. 2009;20:2641–50.
Epstein M, Williams GH, Weinberger M, Lewin A, Krause S, Mukherjee R, et al. Selective aldosterone blockade with eplerenone reduces albuminuria in patients with type 2 diabetes. Clin J Am Soc Nephrol. 2006;1:940–51.
Bianchi S, Bigazzi R, Campese VM. Intensive versus conventional therapy to slow the progression of idiopathic glomerular diseases. Am J Kidney Dis. 2010;55:671–81.
Furumatsu Y, Nagasawa Y, Tomida K, Mikami S, Kaneko T, Okada N, et al. Effect of renin-angiotensin-aldosterone system triple blockade on non-diabetic renal disease: addition of an aldosterone blocker, spironolactone, to combination treatment with an angiotensin-converting enzyme inhibitor and angiotensin II receptor blocker. Hypertens Res. 2008;31:59–67.
Schepkens H, Vanholder R, Billiouw JM, Lameire N. Life-threatening hyperkalemia during combined therapy with angiotensin-converting enzyme inhibitors and spironolactone: an analysis of 25 cases. Am J Med. 2001;110:438–41.
Khosla N, Kalaitzidis R, Bakris GL. Predictors of hyperkalemia risk following hypertension control with aldosterone blockade. Am J Nephrol. 2009;30:418–24.
• Klemmer PJ, Bomback AS: Extracellular volume and aldosterone interaction in chronic kidney disease. Blood Purif. 2009, 27:92–98.
Mitch WE, Wilcox CS. Disorders of body fluids, sodium and potassium in chronic renal failure. Am J Med. 1982;72:536–50.
Raimann JG, Liu L, Zhu F, Thijssen S, Carter M, Bomback AS, Derebail VK, Klemmer PJ, Levin NW, Kotanko P: Changes in serum aldosterone relate to reduction of extracellular volume in hemodialysis patients [abstract]. J Am Soc Nephrol 2010.
Sato A, Funder JW, Saruta T. Involvement of aldosterone in left ventricular hypertrophy of patients with end-stage renal failure treated with hemodialysis. Am J Hypertens. 1999;12:867–73.
Taheri S, Mortazavi M, Shahidi S, Pourmoghadas A, Garakyaraghi M, Seirafian S, et al. Spironolactone in chronic hemodialysis patients improves cardiac function. Saudi J Kidney Dis Transpl. 2009;20:392–7.
Park SH, Lee SW, Lee SJ, Shin WY, Jin DK, Gil HW, et al. The association between left ventricular hypertrophy and biomarkers in patients on continuous ambulatory peritoneal dialysis. Korean Circ J. 2009;39:488–93.
Okazaki A, Mori Y, Nakata M, Kimura T, Sonomura K, Sakoda C, et al. Peritoneal mesothelial cells as a target of local aldosterone action: upregulation of connective tissue growth factor expression via serum- and glucocorticoid-inducible protein kinase 1. Kidney Blood Press Res. 2009;32:151–60.
Nessim SJ, Perl J, Bargman JM. The renin-angiotensin-aldosterone system in peritoneal dialysis: is what is good for the kidney also good for the peritoneum? Kidney Int. 2010;78:23–8.
Hussain S, Dreyfus DE, Marcus RJ, Biederman RW, McGill RL. Is spironolactone safe for dialysis patients? Nephrol Dial Transplant. 2003;18:2364–8.
Saudan P, Mach F, Perneger T, Schnetzler B, Stoermann C, Fumeaux Z, et al. Safety of low-dose spironolactone administration in chronic haemodialysis patients. Nephrol Dial Transplant. 2003;18:2359–63.
• Matsumoto Y, Kageyama S, Yakushigawa T, Arihara K, Sugiyama T, Mori Y, Sugiyama H, Ohmura H, Shio N: Long-term low-dose spironolactone therapy is safe in oligoanuric hemodialysis patients. Cardiology 2009, 114:32–38. In this study, low-dose spironolactone was administered to 61 hemodialysis patients for 6 months without any episodes of severe hyperkalemia. Half of the patients were receiving concurrent therapy with an ACE inhibitor and/or ARB.
Hatch M, Freel RW, Vaziri ND. Local upregulation of colonic angiotensin II receptors enhances potassium excretion in chronic renal failure. Am J Physiol. 1998;274:F275–82.
Michea L, Vukusich A, Gonzalez M, Zehnder C, Marusic ET. Effect of spironolactone on K(+) homeostasis and ENaC expression in lymphocytes from chronic hemodialysis patients. Kidney Int. 2004;66:1647–53.
Sugarman A, Brown RS. The role of aldosterone in potassium tolerance: studies in anephric humans. Kidney Int. 1988;34:397–403.
Hausmann MJ, Liel-Cohen N. Aldactone therapy in a peritoneal dialysis patient with decreased left ventricular function. Nephrol Dial Transplant. 2002;17:2035–6.
Fenwick S, Bell GM. Aldactone therapy in a peritoneal dialysis patient. Nephrol Dial Transplant. 2003;18:1232–3.
Raimann J, Liu L, Tyagi S, Levin NW, Kotanko P. A fresh look at dry weight. Hemodial Int. 2008;12:395–405.
Schjoedt KJ, Andersen S, Rossing P, Tarnow L, Parving HH. Aldosterone escape during blockade of the renin-angiotensin-aldosterone system in diabetic nephropathy is associated with enhanced decline in glomerular filtration rate. Diabetologia. 2004;47:1936–9.
Acknowledgments
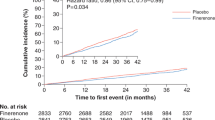
We wish to thank Jochen Raimann, MD; Peter Kotanko, MD; and Nathan Levin, MD, for sharing preliminary data [47] merged with our data [6•] in Fig. 1. We acknowledge funding from the Renal Research Institute for our pilot study.
Disclosure
Conflicts of Interest: M. Volk: none; A. Bomback: none; P. Klemmer: member of Speakers Bureau for Genzyme Corp.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Volk, M.J., Bomback, A.S. & Klemmer, P.J. Mineralocorticoid Receptor Blockade in Chronic Kidney Disease. Curr Hypertens Rep 13, 282–288 (2011). https://doi.org/10.1007/s11906-011-0202-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11906-011-0202-2