Abstract
Purpose of Review
The aim of this review is to summarize the most recent and most robust pharmacogenetic predictors of treatment-related toxicity (TRT) in childhood acute lymphoblastic leukemia (ALL).
Recent Findings
Multiple studies have examined the toxicities of the primary chemotherapeutic agents used to treat childhood ALL in relation to host genetic factors. However, few results have been replicated independently, largely due to cohort differences in ancestry, chemotherapy treatment protocols, and definitions of toxicities. To date, there is only one widely accepted clinical guideline for dose modification based on gene status: thiopurine dosing based on TPMT genotype. Based on recent data, it is likely that this guideline will be modified to incorporate other gene variants, such as NUDT15.
Summary
We highlight genetic variants that have been consistently associated with TRT across treatment groups, as well as those that best illustrate the underlying pathophysiology of TRT. In the coming decade, we expect that survivorship care will routinely specify screening recommendations based on genetics. Furthermore, clinical trials testing protective interventions may modify inclusion criteria based on genetically determined risk of specific TRTs.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •Of importance, ••Of major importance
Abrahao R, Lichtensztajn DY, Ribeiro RC, Marina NM, Keogh RH, Marcos-Gragera R, et al. Racial/ethnic and socioeconomic disparities in survival among children with acute lymphoblastic leukemia in California, 1988–2011: a population-based observational study. Pediatr Blood Cancer. 2015;62(10):1819–25. doi:10.1002/pbc.25544.
Conklin KA. Dietary antioxidants during cancer chemotherapy: impact on chemotherapeutic effectiveness and development of side effects. Nutr Cancer. 2000;37(1):1–18. doi:10.1207/S15327914NC3701_1.
Gupta S, Wilejto M, Pole JD, Guttmann A, Sung L. Low socioeconomic status is associated with worse survival in children with cancer: a systematic review. PLoS One. 2014;9(2):e89482. doi:10.1371/journal.pone.0089482.
Xue H. Nutrition modulation of gastrointestinal toxicity related to cancer chemotherapy from preclinical findings to clinical strategy. JPEN J Parenter Enteral Nutr. 2011;35(1):74–90. doi:10.1177/0148607110377338.
Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA, editors. SEER cancer statistics review, 1975–2013. Bethesda: National Cancer Institute. http://seer.cancer.gov/csr/1975_2013/, based on November 2015 SEER data submission, posted to the SEER web site.
Chang CQ, Yesupriya A, Rowell JL, Pimentel CB, Clyne M, Gwinn M, et al. A systematic review of cancer GWAS and candidate gene meta-analyses reveals limited overlap but similar effect sizes. Eur J Hum Genet. 2014;22(3):402–8. doi:10.1038/ejhg.2013.161.
Yates CR. Molecular diagnosis of thiopurine S-methyltransferase deficiency: genetic basis for azathioprine and mercaptopurine intolerance. Ann Intern Med. 1997;126(8):608. doi:10.7326/0003-4819-126-8-199704150-00003.
Relling MV, Gardner EE, Sandborn WJ, Schmiegelow K, Pui CH, Yee SW, et al. Clinical pharmacogenetics implementation consortium guidelines for thiopurine methyltransferase genotype and thiopurine dosing: 2013 update. Clin Pharmacol Ther. 2013;93(4):324–5. doi:10.1038/clpt.2013.4.
Weinshilboum RM. Mercaptopurine pharmacogenetics: monogenic inheritance of erythrocyte thiopurine methyltransferase activity. Am J Hum Genet. 1980;32(5):651.
Yang SK, Hong M, Baek J, Choi H, Zhao W, Jung Y, et al. A common missense variant in NUDT15 confers susceptibility to thiopurine-induced leukopenia. Nat Genet. 2014;46(9):1017–20. doi:10.1038/ng.3060.
Tanaka Y, Kato M, Hasegawa D, Urayama KY, Nakadate H, Kondoh K, et al. Susceptibility to 6-MP toxicity conferred by a NUDT15 variant in Japanese children with acute lymphoblastic leukaemia. Br J Haematol. 2015;171(1):109–15. doi:10.1111/bjh.13518.
• Yang JJ, Landier W, Yang W, Liu C, Hageman L, Cheng C, et al. Inherited NUDT15 variant is a genetic determinant of mercaptopurine intolerance in children with acute lymphoblastic leukemia. J Clin Oncol. 2015;33(11):1235–42. doi:10.1200/JCO.2014.59.4671. GWAS of >1000 children with ALL describing association between a germline NUDT15 variant and 6-MP intolerance.
Chiengthong K, Ittiwut C, Muensri S, Sophonphan J, Sosothikul D, Seksan P, et al. NUDT15 c.415C>T increases risk of 6-mercaptopurine induced myelosuppression during maintenance therapy in children with acute lymphoblastic leukemia. Haematologica. 2016;101(1):e24–6. doi:10.3324/haematol.2015.134775.
Liang DC, Yang CP, Liu HC, Jaing TH, Chen SH, Hung IJ, et al. NUDT15 gene polymorphism related to mercaptopurine intolerance in Taiwan Chinese children with acute lymphoblastic leukemia. Pharmacogenomics J. 2016;16(6):536–9. doi:10.1038/tpj.2015.75.
Karas-Kuzelicki N, Jazbec J, Milek M, Mlinaric-Rascan I. Heterozygosity at the TPMT gene locus, augmented by mutated MTHFR gene, predisposes to 6-MP related toxicities in childhood ALL patients. Leukemia. 2009;23(5):971–4. doi:10.1038/leu.2008.317.
Liu Y, Yin Y, Sheng Q, Lu X, Wang F, Lin Z, et al. Association of ABCC2 -24C>T polymorphism with high-dose methotrexate plasma concentrations and toxicities in childhood acute lymphoblastic leukemia. PLoS One. 2014;9(1):e82681. doi:10.1371/journal.pone.0082681.
Salazar J, Altes A, del Rio E, Estella J, Rives S, Tasso M, et al. Methotrexate consolidation treatment according to pharmacogenetics of MTHFR ameliorates event-free survival in childhood acute lymphoblastic leukaemia. Pharmacogenomics J. 2012;12(5):379–85. doi:10.1038/tpj.2011.25.
Zgheib NK, Akra-Ismail M, Aridi C, Mahfouz R, Abboud MR, Solh H, et al. Genetic polymorphisms in candidate genes predict increased toxicity with methotrexate therapy in Lebanese children with acute lymphoblastic leukemia. Pharmacogenet Genomics. 2014;24(8):387–96.
Cole PD, Drachtman RA, Masterson M, Smith AK, Glod J, Zebala JA, et al. Phase 2B trial of aminopterin in multiagent therapy for children with newly diagnosed acute lymphoblastic leukemia. Cancer Chemother Pharmacol. 2008;62(1):65–75. doi:10.1007/s00280-007-0576-7.
D'Angelo V, Ramaglia M, Iannotta A, Crisci S, Indolfi P, Francese M, et al. Methotrexate toxicity and efficacy during the consolidation phase in paediatric acute lymphoblastic leukaemia and MTHFR polymorphisms as pharmacogenetic determinants. Cancer Chemother Pharmacol. 2011;68(5):1339–46. doi:10.1007/s00280-011-1665-1.
El-Khodary NM, El-Haggar SM, Eid MA, Ebeid EN. Study of the pharmacokinetic and pharmacogenetic contribution to the toxicity of high-dose methotrexate in children with acute lymphoblastic leukemia. Med Oncol. 2012;29(3):2053–62. doi:10.1007/s12032-011-9997-6.
Erculj N, Kotnik BF, Debeljak M, Jazbec J, Dolzan V. Influence of folate pathway polymorphisms on high-dose methotrexate-related toxicity and survival in childhood acute lymphoblastic leukemia. Leuk Lymphoma. 2012;53(6):1096–104. doi:10.3109/10428194.2011.639880.
Liu SG, Li ZG, Cui L, Gao C, Li WJ, Zhao XX. Effects of methylenetetrahydrofolate reductase gene polymorphisms on toxicities during consolidation therapy in pediatric acute lymphoblastic leukemia in a Chinese population. Leuk Lymphoma. 2011;52(6):1030–40. doi:10.3109/10428194.2011.563883.
•• Lopez-Lopez E, Martin-Guerrero I, Ballesteros J, Garcia-Orad A. A systematic review and meta-analysis of MTHFR polymorphisms in methotrexate toxicity prediction in pediatric acute lymphoblastic leukemia. Pharmacogenomics J. 2013;13(6):498–506. doi:10.1038/tpj.2012.44. Meta-analysis showing no association between MTHFR polymorphisms and MTX-related toxicity in pediatric ALL.
Spyridopoulou KP, Dimou NL, Hamodrakas SJ, Bagos PG. Methylene tetrahydrofolate reductase gene polymorphisms and their association with methotrexate toxicity: a meta-analysis. Pharmacogenet Genomics. 2012;22(2):117–33. doi:10.1097/FPC.0b013e32834ded2a.
Yang L, Hu X, Xu L. Impact of methylenetetrahydrofolate reductase (MTHFR) polymorphisms on methotrexate-induced toxicities in acute lymphoblastic leukemia: a meta-analysis. Tumour Biol. 2012;33(5):1445–54. doi:10.1007/s13277-012-0395-2.
•• Krull KR, Bhojwani D, Conklin HM, Pei D, Cheng C, Reddick WE, et al. Genetic mediators of neurocognitive outcomes in survivors of childhood acute lymphoblastic leukemia. J Clin Oncol. 2013;31(17):2182–8. doi:10.1200/JCO.2012.46.7944. Association of inferior neurocognitive outcomes in ALL survivors with polymorphisms in genes related to metabolism of chemotherapeutic agents and oxidative stress.
Kamdar KY, Krull KR, El-Zein RA, Brouwers P, Potter BS, Harris LL, et al. Folate pathway polymorphisms predict deficits in attention and processing speed after childhood leukemia therapy. Pediatr Blood Cancer. 2011;57(3):454–60. doi:10.1002/pbc.23162.
Krajinovic M, Robaey P, Chiasson S, Lemieux-Blanchard E, Rouillard M, Primeau M, et al. Polymorphisms of genes controlling homocysteine levels and IQ score following the treatment for childhood ALL. Pharmacogenomics. 2005;6(3):293–302. doi:10.1517/14622416.6.3.293.
Kishi S, Cheng C, French D, Pei D, Das S, Cook EH, et al. Ancestry and pharmacogenetics of antileukemic drug toxicity. Blood. 2007;109(10):4151–7.
Eipel O, Hegyi M, Csordás K, Németh K, Luczay A, Török D, et al. Some GCR polymorphisms (N363S, ER22/23EK, and Bcl-1) may influence steroid-induced toxicities and survival rates in children with ALL. J Pediatr Hematol Oncol. 2016;38(5):334–40.
• Cole PD, Finkelstein Y, Stevenson KE, Blonquist TM, Vijayanathan V, Silverman LB, et al. Polymorphisms in genes related to oxidative stress are associated with inferior cognitive function after therapy for childhood acute lymphoblastic leukemia. J Clin Oncol. 2015;33(19):2205–11. doi:10.1200/JCO.2014.59.0273. Recent study confirming the association between inferior neurocognitive outcomes in ALL survivors and gene polymorphisms related to oxidative stress.
Krajinovic M, Elbared J, Drouin S, Bertout L, Rezgui A, Ansari M, et al. Polymorphisms of ABCC5 and NOS3 genes influence doxorubicin cardiotoxicity in survivors of childhood acute lymphoblastic leukemia. Pharmacogenomics J. 2016;16(6):530–5. doi:10.1038/tpj.2015.63.
Ceppi F, Langlois-Pelletier C, Gagné V, Rousseau J, Ciolino C, De Lorenzo S, et al. Polymorphisms of the vincristine pathway and response to treatment in children with childhood acute lymphoblastic leukemia. Pharmacogenomics. 2014;15(8):1105–16.
Egbelakin A, Ferguson MJ, MacGill EA, Lehmann AS, Topletz AR, Quinney SK, et al. Increased risk of vincristine neurotoxicity associated with low CYP3A5 expression genotype in children with acute lymphoblastic leukemia. Pediatr Blood Cancer. 2011;56(3):361–7. doi:10.1002/pbc.22845.
• Diouf B, Crews KR, Lew G, Pei D, Cheng C, Bao J, et al. Association of an inherited genetic variant with vincristine-related peripheral neuropathy in children with acute lymphoblastic leukemia. JAMA. 2015;313(8):815–23. doi:10.1001/jama.2015.0894. GWAS associating a SNP in the promoter region of the CEP72 gene with vincristine induced peripheral neuropathy.
Lopez-Lopez E. Vincristine pharmacokinetics pathway and neurotoxicity during early phases of treatment in pediatric acute lymphoblastic leukemia. Pharmacogenomics. 2016;17(7):731–41. doi:10.2217/pgs-2016-0001.
•• Karol SE, Yang W, Van Driest SL, Chang TY, Kaste S, Bowton E, et al. Genetics of glucocorticoid-associated osteonecrosis in children with acute lymphoblastic leukemia. Blood. 2015;126(15):1770–6. doi:10.1182/blood-2015-05-643601. GWAS of >2000 children with ALL identifying variant in glutamate receptor genes as risk factors for steroid-induced osteonecrosis.
Relling MV, Yang W, Das S, Cook EH, Rosner GL, Neel M, et al. Pharmacogenetic risk factors for osteonecrosis of the hip among children with leukemia. J Clin Oncol. 2004;22(19):3930–6. doi:10.1200/JCO.2004.11.020.
Karol SE, Mattano LA, Yang W, Maloney KW, Smith C, Liu C, et al. Genetic risk factors for the development of osteonecrosis in children under age 10 treated for acute lymphoblastic leukemia. Blood. 2016;127(5):558–64.
French D, Hamilton LH, Mattano Jr LA, Sather HN, Devidas M, Nachman JB, et al. A PAI-1 (SERPINE1) polymorphism predicts osteonecrosis in children with acute lymphoblastic leukemia: a report from the Children’s Oncology Group. Blood. 2008;111(9):4496–9. doi:10.1182/blood-2007-11-123885.
• Finkelstein Y, Blonquist TM, Vijayanathan V, Stevenson KE, Neuberg DS, Silverman LB, et al. A thymidylate synthase polymorphism is associated with increased risk for bone toxicity among children treated for acute lymphoblastic leukemia. Pediatr Blood Cancer. 2016; doi:10.1002/pbc.26393. Recent study reporting association of the TYMS 2R/2R genotype with increased risk of osteonecrosis in young children and bone fractures in older children.
Semsei AF, Erdelyi DJ, Ungvari I, Csagoly E, Hegyi MZ, Kiszel PS, et al. ABCC1 polymorphisms in anthracycline-induced cardiotoxicity in childhood acute lymphoblastic leukaemia. Cell Biol Int. 2012;36(1):79–86. doi:10.1042/CBI20110264.
Visscher H, Ross CJ, Rassekh SR, Barhdadi A, Dube MP, Al-Saloos H, et al. Pharmacogenomic prediction of anthracycline-induced cardiotoxicity in children. J Clin Oncol. 2012;30(13):1422–8. doi:10.1200/JCO.2010.34.3467.
Visscher H, Ross CJ, Rassekh SR, Sandor GS, Caron HN, van Dalen EC, et al. Validation of variants in SLC28A3 and UGT1A6 as genetic markers predictive of anthracycline-induced cardiotoxicity in children. Pediatr Blood Cancer. 2013;60(8):1375–81. doi:10.1002/pbc.24505.
Gregers J, Green H, Christensen IJ, Dalhoff K, Schroeder H, Carlsen N, et al. Polymorphisms in the ABCB1 gene and effect on outcome and toxicity in childhood acute lymphoblastic leukemia. Pharmacogenomics J. 2015;15(4):372–9. doi:10.1038/tpj.2014.81.
Blanco JG, Sun CL, Landier W, Chen L, Esparza-Duran D, Leisenring W, et al. Anthracycline-related cardiomyopathy after childhood cancer: role of polymorphisms in carbonyl reductase genes—a report from the Children’s Oncology Group. J Clin Oncol. 2012;30(13):1415–21. doi:10.1200/JCO.2011.34.8987.
Cascales A, Sanchez-Vega B, Navarro N, Pastor-Quirante F, Corral J, Vicente V, et al. Clinical and genetic determinants of anthracycline-induced cardiac iron accumulation. Int J Cardiol. 2012;154(3):282–6. doi:10.1016/j.ijcard.2010.09.046.
Lipshultz SE, Lipsitz SR, Kutok JL, Miller TL, Colan SD, Neuberg DS, et al. Impact of hemochromatosis gene mutations on cardiac status in doxorubicin-treated survivors of childhood high-risk leukemia. Cancer. 2013;119(19):3555–62. doi:10.1002/cncr.28256.
Chen SH, Pei D, Yang W, Cheng C, Jeha S, Cox NJ, et al. Genetic variations in GRIA1 on chromosome 5q33 related to asparaginase hypersensitivity. Clin Pharmacol Ther. 2010;88(2):191–6. doi:10.1038/clpt.2010.94.
Fernandez CA, Smith C, Yang W, Daté M, Bashford D, Larsen E, et al. HLA-DRB1* 07: 01 is associated with a higher risk of asparaginase allergies. Blood. 2014;124(8):1266–76.
Fernandez CA, Smith C, Yang W, Mullighan CG, Qu C, Larsen E, et al. Genome-wide analysis links NFATC2 with asparaginase hypersensitivity. Blood. 2015;126(1):69–75. doi:10.1182/blood-2015-02-628800.
Kutszegi N, Semsei AF, Gezsi A, Sagi JC, Nagy V, Csordas K, et al. Subgroups of paediatric acute lymphoblastic leukaemia might differ significantly in genetic predisposition to asparaginase hypersensitivity. PLoS One. 2015;10(10):e0140136. doi:10.1371/journal.pone.0140136.
Rajic V, Debeljak M, Goricar K, Jazbec J. Polymorphisms in GRIA1 gene are a risk factor for asparaginase hypersensitivity during the treatment of childhood acute lymphoblastic leukemia. Leuk Lymphoma. 2015;56(11):3103–8. doi:10.3109/10428194.2015.1020802.
Ben Tanfous M, Sharif-Askari B, Ceppi F, Laaribi H, Gagne V, Rousseau J, et al. Polymorphisms of asparaginase pathway and asparaginase-related complications in children with acute lymphoblastic leukemia. Clin Cancer Res. 2015;21(2):329–34. doi:10.1158/1078-0432.CCR-14-0508.
Lopez-Lopez E, Ballesteros J, Pinan MA, Sanchez de Toledo J, Garcia de Andoin N, Garcia-Miguel P, et al. Polymorphisms in the methotrexate transport pathway: a new tool for MTX plasma level prediction in pediatric acute lymphoblastic leukemia. Pharmacogenet Genomics. 2013;23(2):53–61. doi:10.1097/FPC.0b013e32835c3b24.
Lopez-Lopez E, Martin-Guerrero I, Ballesteros J, Pinan MA, Garcia-Miguel P, Navajas A, et al. Polymorphisms of the SLCO1B1 gene predict methotrexate-related toxicity in childhood acute lymphoblastic leukemia. Pediatr Blood Cancer. 2011;57(4):612–9. doi:10.1002/pbc.23074.
Radtke S, Zolk O, Renner B, Paulides M, Zimmermann M, Moricke A, et al. Germline genetic variations in methotrexate candidate genes are associated with pharmacokinetics, toxicity, and outcome in childhood acute lymphoblastic leukemia. Blood. 2013;121(26):5145–53. doi:10.1182/blood-2013-01-480335.
Ramsey LB, Bruun GH, Yang W, Trevino LR, Vattathil S, Scheet P, et al. Rare versus common variants in pharmacogenetics: SLCO1B1 variation and methotrexate disposition. Genome Res. 2012;22(1):1–8. doi:10.1101/gr.129668.111.
Ramsey LB, Panetta JC, Smith C, Yang W, Fan Y, Winick NJ, et al. Genome-wide study of methotrexate clearance replicates SLCO1B1. Blood. 2013;121(6):898–904.
Zhang HN, He XL, Wang C, Wang Y, Chen YJ, Li JX, et al. Impact of SLCO1B1 521T> C variant on leucovorin rescue and risk of relapse in childhood acute lymphoblastic leukemia treated with high-dose methotrexate. Pediatr Blood Cancer. 2014;61(12):2203–7. doi:10.1002/pbc.25191.
Stocco G, Cheok M, Crews K, Dervieux T, French D, Pei D, et al. Genetic polymorphism of inosine triphosphate pyrophosphatase is a determinant of mercaptopurine metabolism and toxicity during treatment for acute lymphoblastic leukemia. Clin Pharmacol Ther. 2009;85(2):164–72.
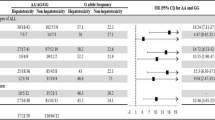
Franca R, Rebora P, Bertorello N, Fagioli F, Conter V, Biondi A, et al. Pharmacogenetics and induction/consolidation therapy toxicities in acute lymphoblastic leukemia patients treated with AIEOP-BFM ALL 2000 protocol. Pharmacogenomics J. 2015; doi:10.1038/tpj.2015.83.
Adam de Beaumais T, Fakhoury M, Medard Y, Azougagh S, Zhang D, Yakouben K, et al. Determinants of mercaptopurine toxicity in paediatric acute lymphoblastic leukemia maintenance therapy. Br J Clin Pharmacol. 2011;71(4):575–84. doi:10.1111/j.1365-2125.2010.03867.x.
Tanaka Y, Manabe A, Nakadate H, Kondoh K, Nakamura K, Koh K, et al. The activity of the inosine triphosphate pyrophosphatase affects toxicity of 6-mercaptopurine during maintenance therapy for acute lymphoblastic leukemia in Japanese children. Leuk Res. 2012;36(5):560–4. doi:10.1016/j.leukres.2011.11.015.
Wan Rosalina WR, Teh LK, Mohamad N, Nasir A, Yusoff R, Baba AA, et al. Polymorphism of ITPA 94C>A and risk of adverse effects among patients with acute lymphoblastic leukaemia treated with 6-mercaptopurine. J Clin Pharm Ther. 2012;37(2):237–41. doi:10.1111/j.1365-2710.2011.01272.x.
Campbell JM, Bateman E, Stephenson MD, Bowen JM, Keefe DM, Peters MD. Methotrexate-induced toxicity pharmacogenetics: an umbrella review of systematic reviews and meta-analyses. Cancer Chemother Pharmacol. 2016;78(1):27–39. doi:10.1007/s00280-016-3043-5.
Faganel Kotnik B, Grabnar I, Bohanec Grabar P, Dolzan V, Jazbec J. Association of genetic polymorphism in the folate metabolic pathway with methotrexate pharmacokinetics and toxicity in childhood acute lymphoblastic leukaemia and malignant lymphoma. Eur J Clin Pharmacol. 2011;67(10):993–1006. doi:10.1007/s00228-011-1046-z.
Tanaka Y, Manabe A, Nakadate H, Kondoh K, Nakamura K, Koh K, et al. Methylenetetrahydrofolate reductase gene haplotypes affect toxicity during maintenance therapy for childhood acute lymphoblastic leukemia in Japanese patients. Leuk Lymphoma. 2014;55(5):1126–31. doi:10.3109/10428194.2013.825902.
Stocco G, Yang W, Crews KR, Thierfelder WE, Decorti G, Londero M, et al. PACSIN2 polymorphism influences TPMT activity and mercaptopurine-related gastrointestinal toxicity. Hum Mol Genet. 2012;21(21):4793–804. doi:10.1093/hmg/dds302.
Relling MV. Mercaptopurine therapy intolerance and heterozygosity at the thiopurine S-methyltransferase gene locus. JNCI: Journal of the National Cancer Institute. 1999;91(23):2001.
Lennard L, Lilleyman JS, Van Loon J, Weinshilboum RM. Genetic variation in response to 6-mercaptopurine for childhood acute lymphoblastic leukaemia. Lancet. 1990;336(8709):225–9. doi:10.1016/0140-6736(90)91745-V.
Moriyama T, Nishii R, Perez-Andreu V, Yang W, Klussmann FA, Zhao X, et al. NUDT15 polymorphisms alter thiopurine metabolism and hematopoietic toxicity. Nat Genet. 2016;48(4):367–73. doi:10.1038/ng.3508.
Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline information for mercaptopurine and TPMT-May 2016 Update on PharmGKB. https://www.pharmgkb.org/guideline/PA166104945.
Tanaka Y, Manabe A, Fukushima H, Suzuki R, Nakadate H, Kondoh K, et al. Multidrug resistance protein 4 (MRP4) polymorphisms impact the 6-mercaptopurine dose tolerance during maintenance therapy in Japanese childhood acute lymphoblastic leukemia. Pharmacogenomics J. 2015;15(4):380–4. doi:10.1038/tpj.2014.74.
Cole PD, Kamen BA. Delayed neurotoxicity associated with therapy for children with acute lymphoblastic leukemia. Ment Retard Dev Disabil Res Rev. 2006;12(3):174–83. doi:10.1002/mrdd.20113.
Duffner PK. Neurocognitive and neuroradiologic central nervous system late effects in children treated on Pediatric Oncology Group (POG) P9605 (standard risk) and P9201 (lesser risk) acute lymphoblastic leukemia protocols (ACCL0131): a methotrexate consequence? A report from the Children’s Oncology Group. J Pediatr Hematol Oncol. 2014;36(1):8–15. doi:10.1097/MPH.0000000000000000.
Hearps S, Seal M, Anderson V, McCarthy M, Connellan M, Downie P, et al. The relationship between cognitive and neuroimaging outcomes in children treated for acute lymphoblastic leukemia with chemotherapy only: a systematic review. Pediatr Blood Cancer. 2017;64(2):225–33. doi:10.1002/pbc.26188.
Jacola LM, Krull KR, Pui CH, Pei D, Cheng C, Reddick WE, et al. Longitudinal assessment of neurocognitive outcomes in survivors of childhood acute lymphoblastic leukemia treated on a contemporary chemotherapy protocol. J Clin Oncol. 2016;34(11):1239–47. doi:10.1200/JCO.2015.64.3205.
Hochhauser CJ, Lewis M, Kamen BA, Cole PD. Steroid-induced alterations of mood and behavior in children during treatment for acute lymphoblastic leukemia. Support Care Cancer. 2005;13(12):967–74.
Strauss AJ, Su JT, Dalton VMK, Gelber RD, Sallan SE, Silverman LB. Bony morbidity in children treated for acute lymphoblastic leukemia. J Clin Oncol. 2001;19(12):3066–72.
Warner JT, Evans WD, Webb DKH, Bell W, Gregory JW. Relative Osteopenia after treatment for acute lymphoblastic leukemia. Pediatr Res. 1999;45(4, Part 1 of 2):544–51.
Wilson CL, Ness KK. Bone mineral density deficits and fractures in survivors of childhood cancer. Curr Osteoporos Rep. 2013;11(4):329–37. doi:10.1007/s11914-013-0165-0.
Kunstreich M, Kummer S, Laws HJ, Borkhardt A, Kuhlen M. Osteonecrosis in children with acute lymphoblastic leukemia. Haematologica. 2016;101(11):1295–305. doi:10.3324/haematol.2016.147595.
Mattano LA, Devidas M, Chen S, Esiashvili N, Asselin B, Winick NJ, et al. Effect of high-dose methotrexate (HD-MTX) vs Capizzi methotrexate/pegaspargase (C-MTX/ASNase) on osteonecrosis (ON) incidence in children and young adults with T-acute lymphoblastic leukemia (T-ALL): results of Children’s Oncology Group (COG) Study AALL0434. Blood. 2014;124(21):3649.
Badhiwala JH, Nayiager T, Athale UH. The development of thromboembolism may increase the risk of osteonecrosis in children with acute lymphoblastic leukemia. Pediatr Blood Cancer. 2015;62(10):1851–4. doi:10.1002/pbc.25553.
Bond J, Adams S, Richards S, Vora A, Mitchell C, Goulden N. Polymorphism in the PAI-1 (SERPINE1) gene and the risk of osteonecrosis in children with acute lymphoblastic leukemia. Blood. 2011;118(9):2632–3.
Kawedia JD, Kaste SC, Pei D, Panetta JC, Cai X, Cheng C, et al. Pharmacokinetic, pharmacodynamic, and pharmacogenetic determinants of osteonecrosis in children with acute lymphoblastic leukemia. Blood. 2011;117(8):2340–7.
Wang X, Liu W, Sun CL, Armenian SH, Hakonarson H, Hageman L, et al. Hyaluronan synthase 3 variant and anthracycline-related cardiomyopathy: a report from the Children’s Oncology Group. J Clin Oncol. 2014;32(7):647–53. doi:10.1200/JCO.2013.50.3557.
Aminkeng F, Ross CJ, Rassekh SR, Hwang S, Rieder MJ, Bhavsar AP, et al. Recommendations for genetic testing to reduce the incidence of anthracycline-induced cardiotoxicity. Br J Clin Pharmacol. 2016;82(3):683–95. doi:10.1111/bcp.13008.
Chakrabarti R, Schuster S. L-asparaginase: perspectives on the mechanisms of action and resistance. International Journal of Pediatric Hematology/Oncology. 1997;4(6):597–611.
Pieters R, Hunger SP, Boos J, Rizzari C, Silverman L, Baruchel A, et al. L-asparaginase treatment in acute lymphoblastic leukemia: a focus on Erwinia asparaginase. Cancer. 2011;117(2):238–49. doi:10.1002/cncr.25489.
Tanaka Y, Urayama KY, Kawaguchi T, Mori M, Hasegawa D, Ishimaru S, et al. The association between L-asparaginase hypersensitivity and genetic variants in Japanese childhood ALL patients. Blood. 2016;128(22):5141.
Wolthers BO, Frandsen TL, Abrahamsson J, Albertsen BK, Helt LR, Heyman M, et al. Asparaginase-associated pancreatitis: a study on phenotype and genotype in the NOPHO ALL2008 protocol. Leukemia. 2016; doi:10.1038/leu.2016.203.
Fernandez CA, Smith C, Yang W, Liu C, Ramsey LB, Karol SE, et al. Genome-wide association study identifies PNPLA3 I148M variant associated with elevated transaminase levels after induction therapy in pediatric ALL patients. Blood. 2015;126(23):3714.
Marsh S, King CR, Ahluwalia R, McLeod HL. Distribution of ITPA P32T alleles in multiple world populations. J Hum Genet. 2004;49(10):579–81. doi:10.1007/s10038-004-0183-y.
Hagleitner MM, Coenen MJ, Aplenc R, Patino-Garcia A, Chiusolo P, Gemmati D, et al. The role of the MTHFR 677C>T polymorphism in methotrexate-induced liver toxicity: a meta-analysis in patients with cancer. Pharmacogenomics J. 2014;14(2):115–9. doi:10.1038/tpj.2013.19.
den Hoed M, Lopez-Lopez E, Te Winkel ML, Tissing W, de Rooij J, Gutierrez-Camino A, et al. Genetic and metabolic determinants of methotrexate-induced mucositis in pediatric acute lymphoblastic leukemia. The pharmacogenomics journal. 2015;15(3):248–54.
Liu S, Gao C, Zhang R, Zhao X, Cui L, Li W, et al. Germline genetic variations in methotrexate candidate genes are associated with pharmacokinetics and outcome in pediatric acute lymphoblastic leukemia in China. Blood. 2016;128(22):1595.
Asselin BL, Devidas M, Chen L, Franco VI, Pullen J, Borowitz MJ, et al. Cardioprotection and safety of dexrazoxane in patients treated for newly diagnosed T-cell acute lymphoblastic leukemia or advanced-stage lymphoblastic non-Hodgkin lymphoma: a report of the Children’s Oncology Group Randomized Trial Pediatric Oncology Group 9404. J Clin Oncol. 2016;34(8):854–62. doi:10.1200/JCO.2015.60.8851.
Pengde K, Fuxing P, Bin S, Jing Y, Jingqiu C. Lovastatin inhibits adipogenesis and prevents osteonecrosis in steroid-treated rabbits. Joint Bone Spine. 2008;75(6):696–701.
Pritchett JW. Statin therapy decreases the risk of osteonecrosis in patients receiving steroids. Clin Orthop Relat Res. 2001;386:173–8.
Cole PD, Vijayanathan V, Ali NF, Wagshul ME, Tanenbaum EJ, Price J, et al. Memantine protects rats treated with intrathecal methotrexate from developing spatial memory deficits. Clin Cancer Res. 2013;19(16):4446–54.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Rochelle R. Maxwell and Peter D. Cole each declare no potential conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Topical Collection on Acute Lymphocytic Leukemias
Rights and permissions
About this article
Cite this article
Maxwell, R.R., Cole, P.D. Pharmacogenetic Predictors of Treatment-Related Toxicity Among Children With Acute Lymphoblastic Leukemia. Curr Hematol Malig Rep 12, 176–186 (2017). https://doi.org/10.1007/s11899-017-0376-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11899-017-0376-z