Abstract
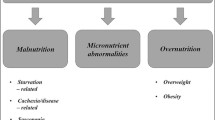
Heart failure (HF) is a syndrome characterized by high morbidity and mortality, despite advances in medical and device therapy that have significantly improved survival. The outcome of HF in elderly patients results from a combination of biological, functional, psychological, and environmental factors, one of which is nutritional status. Malnutrition, as well as HF, is frequently present with aging. Early detection might lead to earlier intervention. It is our goal to review the importance of nutritional status in elderly patients with HF, as well as tools for assessing it. We also propose a simple decision algorithm for the nutritional assessment of elderly patients with HF.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lindenfeld J, Albert NM, Boehmer JP, et al. Executive Summary: HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010;16:475–539.
Krim SR, Campbell P, Lavie CJ, Ventura H. Micronutrients in chronic heart failure. Curr Heart Fail Rep. 2013;10(1):46–53.
Heart disease and stroke statistics—2011 update. A report from the American Heart Association. Circulation. 2011;123:e18–209.
Roger VL, Weston SA, Redfield MM, et al. Trends in heart failure incidence and survival in a community-based population. JAMA. 2004;292(3):344–50.
Levy D, Kenchaiah S, Larson MG, et al. Long-term trends in the incidence of and survival with heart failure. N Engl J Med. 2002;347:1397–402.
Kulminski AM, Ukraintseva SV, Kulminskaya IV, et al. Cumulative deficits better characterize susceptibility to death in elderly people than phenotypic frailty: lessons from the Cardiovascular Health Study. J Am Geriatr Soc. 2008;56:898–903.
Ahmed T, Haboubi N. Assessment and management of nutrition in older people and its importance to health. Clin Interv Aging. 2010;5:207–16.
Vischer UM, Frangos E, Graf C, et al. The prognostic significance of malnutrition as assessed by the Mini Nutritional Assessment (MNA) in older hospitalized patients with a heavy disease burden. Clin Nutr. 2012;31(1):113–7.
Foley NC, Salter KL, Robertson J, Teasell RW, Woodbury MG. Which reported estimate of the prevalence of malnutrition after stroke is valid? Stroke. 2009;40:e66–74.
Pilotto A, Addante F, Franceschi M, et al. Multidimensional Prognostic Index based on a comprehensive geriatric assessment predicts short-term mortality in older patients with heart failure. Circ Heart Fail. 2010;3:14–20. Although the Multidimensional Prognostic Index is not a nutritional scoring system, it is a comprehensive multidimensional assessment for geriatric patients with HF.
Gastelurrutia P, Lupon J, Domingo M, et al. Usefulness of body mass index to characterize nutritional status in patients with heart failure. Am J Cardiol. 2011;108:1166–70.
Kalantar-Zadeh K, Block G, Horwich T, Fonarow GC. Reverse epidemiology of conventional cardiovascular risk factors in patients with chronic heart failure. J Am Coll Cardiol. 2004;43:1439–44.
Kalantar-Zadeh K, Anker SD, Horwich T, Fonarow GC. Nutritional and anti-inflammatory interventions in chronic heart failure. Am J Cardiol. 2008;101(suppl):89E–103E.
Anker SD, Ponikowski P, Varney S, et al. Wasting as independent risk factor for mortality in chronic heart failure. Lancet. 1997;349:1050–3.
Berkowitz D, Croll MN, Likoff W. Malabsorption as a complication of congestive heart failure. Am J Cardiol. 1963;11:43–7.
Bauer JM, Kaiser MJ, Sieber CC. Evaluation of nutritional status in older persons: nutritional screening and assessment. Curr Opin Clin Nutr Metab Care. 2010;13:8–13.
Gastelurrutia P, Lupón J, Domingo M, et al. Usefulness of body mass index to characterize nutritional status in patients with heart failure. Am J Cardiol. 2011;108(8):1166–70. This article confirms that BMI does not indicate true nutritional status in patients with HF.
Castillo-Martínez L, Colín-Ramírez E, Orea-Tejeda A, et al. Cachexia assessed by bioimpedance vector analysis as a prognostic indicator in chronic stable heart failure patients. Nutrition. 2012;28:886–91.
Casas-Vara A, Santolaria F, Fernández-Bereciartúa A, et al. The obesity paradox in elderly patients with heart failure: analysis of nutritional status. Nutrition. 2012;28(6):616–22. This report confirms the obesity paradox in elderly patients with HF.
Oreopoulos A, Padwal R, Kalantar-Zadeh K, et al. Body mass index and mortality in heart failure: a meta-analysis. Am Heart J. 2008;156:13–22.
Nagarajan V, Cauthen CA, Starling RC, Tang WH. Prognosis of morbid obesity patients with advanced heart failure. Congest Heart Fail. 2013;19(4):160–4.
Nescolarde L, Gastelurrutia P, Calpe J, et al. Comment on “Is bioelectrical impedance vector analysis of value in the elderly with malnutrition and impaired functionality?”. Nutrition. 2009;25:370–1.
Anker SD, Ponikowski PP, Clark AL, et al. Cytokine and neurohormones relating to body composition alterations in the wasting syndrome of chronic heart failure. Eur Heart J. 1999;20:683–93.
Fulster S, Tacke M, Sandek A, et al. Muscle wasting in patients with chronic heart failure: results from the studies investigating comorbidities aggravating heart failure (SICA-HF). Eur Heart J. 2013;34:512–9. This paper evaluates the relationship between wasting and the functional status of patients with chronic HF. Patients with muscle wasting have reduced exercise capacity (6-minute walk time and peak VO2), muscle strength, and left ventricle ejection fraction.
Kondrup J, Allison SP, Elia M, Vellas B, Plauth M. ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003;22:415–21.
Yamauti AK, Ochiai ME, Bifulco PS, et al. Subjective global assessment of nutritional status in cardiac patients. Arq Bras Cardiol. 2006;87:772–7.
Malnutrition Advisory Group (MAG). MAG guidelines for detection and management of malnutrition. Redditch: British Association for Parenteral and Enteral Nutrition; 2000.
Kondrup J, Rasmussen HH, Hamberg O, Ad SZ, Hoc ESPEN. Working Group. Nutritional Risk Screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22:321–36.
Vellas B, Guigoz Y, Garry PJ, et al. The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition. 1999;15:116–22.
Neelemaat F, Kruizenga HM, de Vet HC, et al. Screening malnutrition in hospital outpatients. Can the SNAQ malnutrition screening tool also be applied to this population? Clin Nutr. 2008;27:439–46.
Al-Najjar Y, Clark AL. Predicting outcome in patients with left ventricular systolic chronic heart failure using a nutritional risk index. Am J Cardiol. 2012;109(9):1315–20. This easy-to-use nutritional scoring system includes serum albumin and weight. Based on NRI scores, 23 % of patients are at risk for malnutrition. The score is a univariable predictor of mortality.
Naber TH, Schermer T, de Bree A, et al. Prevalence of malnutrition in nonsurgical hospitalized patients and its association with disease complications. Am J Clin Nutr. 1997;66:1232–9.
Baker JP, Detsky AS, Wesson DE, et al. A comparison of clinical judgment and objective measurements. N Engl J Med. 1982;306:969–72.
Stratton RJ, Hackston A, Longmore D, et al. Malnutrition in hospital outpatients and inpatients: prevalence, concurrent validity and ease of use of the ‘malnutrition universal screening tool’ (‘MUST’) for adults. Br J Nutr. 2004;92:799–808.
Nochioka K, Sakata Y, Takahashi J, et al. CHART-2 Investigators. Prognostic impact of nutritional status in asymptomatic patients with cardiac diseases: a report from the CHART-2 Study. Circ J. 2013;77(9):2318–26. The CONUT score includes serum albumin, total cholesterol, and lymphocyte count. In this study, it was applied in patients with stage B HF. Poor nutritional status was associated with an increased incidence of death in the entire CHART-2 population and with the risk of hospitalization in the elderly population.
Pilotto A, Ferrucci L, Franceschi M, et al. Development and validation of a multidimensional prognostic index for 1-year mortality from the comprehensive geriatric assessment in hospitalized older patients. Rejuvenation Res. 2008;11:151–61.
Sargento L, Satendra M, Almeida I, et al. Nutritional status of geriatric outpatients with systolic heart failure and its prognostic value regarding death or hospitalization, biomarkers and quality of life. J Nutr Health Aging. 2013;17:300–4. There is good agreement between the MNA full and short forms. The MNA score correlated significantly with the patient’s quality of life and levels of N-terminal pro-brain natriuretic peptide and albumin. The short-form MNA was a predictor of outcome.
Bonilla-Palomas JL, Gámez-López AL, Anguita-Sánchez MP, et al. Impact of malnutrition on long-term mortality in hospitalized patients with heart failure. Rev Esp Cardiol. 2011;64(9):752–8. Malnutrition and the risk of malnutrition, as evaluated with the MNA, are highly prevalent (13.0 % and 59.6 %) in patients hospitalized for HF. The nutritional status, as classified by the MNA, was associated with survival.
Aggarwal A, Kumar A, Gregory MP, et al. Nutrition assessment in advanced heart failure patients evaluated for ventricular assist devices or cardiac transplantation. Nutr Clin Pract. 2013;28:112–9. Malnutrition is prevalent, as assessed with the MNA, in patients with advanced HF (being evaluated for ventricular-assisted devices or cardiac transplantation) and is an independent predictor of mortality.
Vellas B, Villars H, Abellan G, et al. Overview of the MNA—its history and challenges. J Nutr Health Aging. 2006;10(6):456–63.
Guigoz Y. The Mini Nutritional Assessment (MNA) review of the literature—what does it tell us? J Nutr Health Aging. 2006;10(6):466–85.
Guigoz Y, Lauque S, Vellas BJ. Identifying the elderly at risk for malnutrition. The Mini Nutritional Assessment. Clin Geriatr Med. 2002;18:737–57.
Bauer JM, Kaiser MJ, Anthony P, Guigoz Y, Sieber CC. The Mini Nutritional Assessment—its history, today's practice, and future perspectives. Nutr Clin Pract. 2008;23(4):388–96.
Tsai AC, Chang TL, Wang YC, et al. Population-specific short-form mini nutritional assessment with BMI or calf-circumference can predict risk of malnutrition in community-living or institutionalized elderly in Taiwan. J Am Diet Assoc. 2010;110:1328–34.
Tsai AC, Chou YT, Chang TL, et al. A modified mini nutritional assessment without BMI can effectively assess the nutritional status of neuropsychiatric patients. J Clin Nurs. 2009;18:1916–22.
Kuzuya M, Kanda S, Koike T, et al. Evaluation of mini-nutritional assessment for Japanese frail elderly. Nutrition. 2005;21:498–503.
Tsai AC, Chang TL, Yang T-W, et al. A modified mini nutritional assessment without BMI predicts nutritional status of community-living elderly in Taiwan. J Nutr Health Aging. 2010;14:183–9.
Rubenstein LZ, Harker JO, Salva A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form Mini-Nutritional Assessment (MNA-SF). J Gerontol A Biol Sci Med Sci. 2001;56:M366–72.
Kaiser MJ, Bauer JM, Uter W, et al. Validation of the mini nutritional assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13(9):782–8.
Poulia KA, Yannakoulia M, Karageorgou D, et al. Evaluation of the efficacy of six nutritional screening tools to predict malnutrition in the elderly. Clin Nutr. 2012;31:378–85.
Kinugasa Y, Kato M, Sugihara S, et al. Geriatric Nutritional Risk Index predicts functional dependency and mortality in patients with heart failure with preserved ejection fraction. Circ J. 2013;77:705–11. This is the only paper evaluating the nutritional status of patients with HF with preserved left ventricular ejection fraction. The authors applied the GNRI score (serum albumin and BMI). There was an association with prognosis.
Zapatero A, Barba R, Gonzalez N, et al. Influence of obesity and malnutrition on acute heart failure. Rev Esp Cardiol. 2012;65(5):421–6. The authors used a huge national database of patients with acute HF and evaluated nutritional status (methodology not referenced, only the ICD-9-CM code) prevalence and its impact on the outcome at 30 days.
Compliance with Ethics Guidelines
Conflict of Interest
Luis Sargento has received payment for the development of educational presentations from Servier.
Susana Longo declares that she has no conflict of interest.
Nuno Lousada has received payment for lectures, including service on speakers bureaus from Servier.
Roberto Palma dos Reis has received compensation for service as a consultant for Delta Laboratories.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sargento, L., Longo, S., Lousada, N. et al. The Importance of Assessing Nutritional Status in Elderly Patients with Heart Failure. Curr Heart Fail Rep 11, 220–226 (2014). https://doi.org/10.1007/s11897-014-0189-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-014-0189-5