Abstract
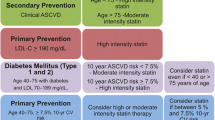
Despite major advances, many patients with diabetes are currently achieving suboptimal control of lipids and blood pressure. The new cholesterol guidelines by the ACC/AHA have reignited the emphasis on more intensive treatment with statins in the population at high risk of CVD, including those with diabetes. While these guidelines do not include specific lipid goals, several other guidelines have retained previously defined risk-based LDL-C and non-HDL-C goals. More recent data indicate potential benefits in CVD outcomes with non-statin therapy added to statin therapy. On-going long-term trials with PCSK-9 inhibitors may help answer the question of the benefits and safety of very low LDL-C. Regarding the blood pressure guidelines, there remains an inconsistency of evidence for targets to reduce CVD outcomes. The ACCORD trial weighted heavily in the recent meta-analyses, leading to currently recommended goal of <140/90 mmHg. Studies targeting blood pressure goals of <130 mmHg in younger patients with diabetes, including sub-populations of interest, may help solve the controversy. Until we have these data, perhaps it is time to shift our focus from a rigid blood pressure target to risk-based goals.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
The Emerging Risk Factors Collaboration. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375:2215–22.
Shah AD, Langenberg C, Rapsomaniki E, et al. Type 2 diabetes and incidence of cardiovascular diseases: a cohort study in 1.9 million people. Lancet Diabetes Endocrinol. 2015;3:105–13.
Baigent C, Blackwell L, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670–81.
Cholesterol Treatment Trialists’ (CTT) Collaborators, Mihaylova B, Emberson J, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380:581–90.
Kearney PM, Blackwell L, Collins R, Keech A, Simes J, Peto R, et al. Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet. 2008;371:117–25.
•• Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2889–934. This is the latest cholesterol guideline paper from AHA and ACC, an evidence based document stratifying patients with or without diabetes, but a major departure from ATP III and other guidelines, leading to some controversy.
Hayward RA. Moneyball, gambling, and the new cholesterol guidelines. Circ Cardiovasc Qual Outcomes. 2014;7:311–4.
Ginsberg HN. The 2013 ACC/AHA guidelines on the Treatment of Blood Cholesterol: questions, questions, questions. Circ Res. 2014;114:761–4.
Nissen SE. Prevention guidelines. Bold process, bad outcome. JAMA Intern Med. 2014;174:1972–3.
Ganda OP. Deciphering cholesterol treatment guidelines: a clinician’s perspective. JAMA. 2015;313:1009–10.
NICE clinical guideline, CG 181. Lipid modification. Cardiovascular risk assessment and modification of blood lipids for the primary and secondary prevention of cardiovascular disease. National Clinical Guideline Centre, July 2014, pp 1-292
Jacobsen TA, Ito MK, Maki KC, et al. National Lipid Association recommendations for patient-centered management of dyslipidemia: part 1—executive summary. J Clin Lipidol. 2014;8:473–88.
Piepoli, MF et al 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Eur Herat J 2016; doi:10.1093/eurheartj/ehw106
ADA. Standards of medical care in diabetes in 2016. Diabetes Care. 2016;39(Suppl1):S60–71.
•• Cannon CP, Blazing MA, Giugliano RP, et al. Ezetimibe added to simvastatin therapy in acute coronary syndromes. N Engl J Med. 2015;372:2787–97. The first major CVD trial describing a modest but significant benefit by the addition of a non- statin drug to moderate dose statin in high risk patients.
• Robinson JG, Farnier M, Krempf M, et al. Efficacy and safety of alirocumab in reducing lipids and cardiovascular events. N Engl J Med. 2015;372:1489–99. doi:10.1056/NEJMoa1501031. This RCT describes the initial, albeit short – term, data on the CVD benefits of PCSK -9 inhibitor.
• Sabatine MS, Giugliano RP, Wiviott SD, et al. Efficacy and safety of evolocumab in reducing lipids and cardiovascular events. N Engl J Med. 2015;372:1500–9. doi:10.1056/NEJMoa1500858. This RCT describes the initial, albeit short – term, data on the CVD benefits of PCSK -9 inhibitor.
•• Lloyd-Jones, DM, Morris, PB, Ballantyne, CM et al 2016 ACC Expert Consensus Decision Pathway on the Role of Non-Statin Therapies for LDL-Cholesterol Lowering in the Management of Atherosclerotic Cardiovascular Disease Risk. J Amer Col Cardiol. doi: 10.1016/j.jacc.2016.03.519. This is the latest consensus statement from ACC, incorporating non- statin therapies in patients with CVD or high risk patients including those with diabetes.
•• de Ferranti SD, de Boer IH, Fonseca V, et al. Type 1 diabetes mellitus and cardiovascular disease: a scientific statement from the American Heart Association and American Diabetes Association. Diabetes Care. 2014;37:2843–63. A position statement from AHA and ADA describing the high burden of CVD in patients with Type 1 diabetes.
Lind M, Svensson A-M, Kosiborod M, et al. Glycemic control and excess mortality in T1 diabetes. N Engl J Med. 2014;371:1972–82.
Hero C, Rawshani A, Svensson A-M, et al. Association between use of lipid-lowering therapy and cardiovascular diseases and death in individuals with type 1 diabetes. Diabetes Care. 2016;39:996–1003. doi:10.2337/dc15-2450.
DeGorter MK, Tirina RG, Schwartz UI, et al. Clinical and pharmacogenetic predictors of circulating atorvastatin and rosuvastatin concentrations in routine clinical care. Circ Cardiovasc Genet. 2013;16:400–8.
Ali MK, Bullard KM, Gregg EW, et al. A cascade of care for diabetes in the United States: visualizing the gaps. Ann Intern Med. 2014;161(10):681–9.
Boekholdt SM, Hoving GK, Mora S, et al. Very lowl levels of atherogenic lipoproteins and the 4risk for cardiovascular events. A meta-analysis of statin trials. J Am Coll Cardiol. 2014;64(5):485–94.
•• Musunuru K. Kathiresan, K Surprises from genetic analyses of lipid risk factors for atherosclerosis. Circ Res. 2016;118:579–85. A well described summary paper describing the relationship of genetic polymorphism of lipid factors and their relationship to CVD in many large population studies.
Hegele RA, Ginsberg HN, Chapman MJ, et al. The polygenic nature of hypertriglyceridaemia: implications for definition, diagnosis, and management. Lancet Diabetes Endocrinol. 2014;2(8):655–66.
•• Khetarpal SA, Rader DJ. Triglyceride-rich lipoproteins and coronary artery disease risk: new insights from human genetics. Arterioscler Thromb Vasc Biol. 2015;35(2):e3–9. This is an excellent review of the current state of genetic detrerminants of triglyceride- rich lipoproteins and their potential impact on atherogenesis.
ACCORD Study Group, Ginsberg HN, Elam MB, et al. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1563–74.
Boden W et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011;365:2255–67.
The HPS2-THRIVE Collaborative Group. Effects of extended release niacin with laropiprant in high-risk patients. N Engl J Med. 2014;371:203–12.
Nissen SE, Wolski K, Topol EJ. Effect of muraglitazar on death and major adverse cardiovascular events in patients with type 2 diabetes mellitus. JAMA. 2005;294:2581–6.
Conlon D. Goodbye glitazars. Br J Diabetes Vasc Dis. 2006;6:135–7.
Lincoff AM, Cardiff JC, Schwartz GG, et al. Effect of Aleglitazar on cardiovascular outcomes after acute coronary syndrome in patients with type 2 diabetes mellitus The AleCardio Randomized Clinical Trial. JAMA. 2014;311:1515–25.
Barter PJ, Caulfield M, Eriksson M, et al. Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med. 2007;357(21):2109–22.
Schwartz GG, Olsson AG, Abt M, et al. Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med. 2012;367(22):2089–99.
Nicholls SJ, Lincoff A, Barter P, et al. Late-Breaking Clinical Trials II. The ACCELERATE trial: impact of the cholesteryl ester transfer protein inhibitor evacetrapib on cardiovascular outcome. Presented at the 65th Annual Scientific Session and Expo of the American College of Cardiology. April 2-4, 2016; Chicago, IL.
A Study of AMR101 to Evaluate Its Ability to Reduce Cardiovascular Events in High Risk Patients With Hypertriglyceridemia and on Statin. The Primary Objective is to Evaluate the Effect of 4 g/Day AMR101 for Preventing the Occurrence of a First Major Cardiovascular Event. (REDUCE-IT). https://clinicaltrials.gov/ct2/show/NCT01492361. Accessed July 6, 2016
Outcomes Study to Assess STatin Residual Risk Reduction With EpaNova in HiGh CV Risk PatienTs With Hypertriglyceridemia (STRENGTH). https://clinicaltrials.gov/ct2/show/NCT02104817. Accessed July 6, 2016
Turner R, Holman R, Matthews D, et al. Hypertension in diabetes study (Hds). 1. Prevalence of hypertension in newly presenting Type-2 diabetic-patients and the association with risk-factors for cardiovascular and diabetic complications. J Hypertens. 1993;11(3):309–17.
Pechère‐bertschi A, Greminger P, Hess L, Philippe J, Ferrari P. Swiss Hypertension and Risk Factor Program (SHARP): cardiovascular risk factors management in patients with type 2 diabetes in Switzerland. Blood Press. 2005;14(6):337–44.
Prospective S. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):637–46.
James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–20.
Weber, MA, Sciffrin, EL, Wright WB et al. Clinical Practice Guidelines for the Management of Hypertension in the Community. A Statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertension DOI: 10.1111/jch.12237
Harris KC, Benoit G, Dionne J, et al. Hypertension Canada’s 2016 Canadian Hypertension Education Program Guidelines for blood pressure measurement, diagnosis, and assessment of risk of pediatric hypertension. Can J Cardiol. 2016;32(5):589–97.
Garber, A J., Abrahamson,M, Brazilay, J et al. “Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm-2016 executive summary.” Endocrine Practice 22.1 (2016):84–113.
National Institute forHealth and Care Excellence.Type 2 diabetes in adults: management. NICE Guideline, 2015; https://www.nice.org.uk/guidance/ng28. Accessed July 8, 2016
•• Cushman WC, Evans GW, Byington RP et al. Effect of intensive blood pressure control in type 2 diabetes mellitus. N Engl J Med 2010, 362:1575–1585. This study is important because it reported that targeting a systolic blood pressure of less than 120 mm Hg, as compared with less than 140 mm Hg, did not reduce the rate of a composite outcome of fatal and nonfatal major cardiovascular events; leading to a change of blood pressure target in most guidelines; however, it provided stroke benefit.
The SPRINT Research Group> A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;2015(373):2103–16.
•• Lonn EM, Bosch J, López-Jaramillo P, et al. Blood-pressure lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374(21):2009–20. This study is relevant because it supported the hypothesis that treating persons without cardiovascular disease who have a systolic blood pressure above approximately 140 mm Hg appears to be beneficial, but treatment would not be of benefit and may be even harmful in persons with lower systolic blood pressure levels. The study did not include extreme ages and included only 6% of patients with diabetes.
Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet. 1998;351(9118):1755–62.
Group UPDS. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;77:703–13.
Reboldi G, Gentile G, Angeli F, Ambrosio G, Mancia G, Verdecchia P. Effects of intensive blood pressure reduction on myocardial infarction and stroke in diabetes: a meta-analysis in 73 913 patients. J Hypertens. 2011;29(7):1253–69.
Bangalore S, Kumar S, Lobach I, Messerli FH. Blood pressure targets in subjects with type 2 diabetes mellitus/impaired fasting glucose observations from traditional and bayesian random-effects meta-analyses of randomized trials. Circulation. 2011;123(24):2799–810.
Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2015;313(6):603–15.
Brunström M, Carlberg B. Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: systematic review and meta-analyses. BMJ. 2016;352:i717.
Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387(10022):957–67.
Xie X, Atkins E, Lv J, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387(10017):435–43.
• Espeland MA, Probstfield J, Hire D, et al. Systolic blood pressure control among individuals with type 2 diabetes: a comparative effectiveness analysis of three interventions. Am J Hypertens. 2015;28:995–1005. This study is relevant because it highlights the importance of intensive lifestyle intervention and shows that it could be at least as beneficial as goal targeted blood pressure treatment in obese patients with diabetes.
Acknowledgments
Supported in part by NIH Grant P30DK36836-Diabetes enrichment core.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Om Ganda has received research funding from Amarin Pharmaceuticals, consulting fees from Amgen and Sanofi- Regeneron, and speaker’s honoraria from Amgen and Merck.
Joanna Mitri has received research funding from the American Dairy Council.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Diabetes and Cardiovascular Disease
Rights and permissions
About this article
Cite this article
Ganda, O.P., Mitri, J. Current Consensus and Controversies in Guidelines for Lipid and Hypertension Management in Diabetes. Curr Cardiol Rep 18, 114 (2016). https://doi.org/10.1007/s11886-016-0790-1
Published:
DOI: https://doi.org/10.1007/s11886-016-0790-1