Abstract
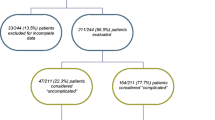
Urodynamic studies (UDS) have been used to objectively characterize a patient’s complaint of urinary incontinence. Presumably, the clinician can utilize the UDS data to guide treatment options. It is even hoped that UDS can help predict which treatments should be utilized to produce the most effective outcomes. However, is this currently the case? The Urinary Incontinence Treatment Network (UITN) has completed four large randomized clinical trials related to treatments for urinary incontinence. Two trials compared outcomes of different surgeries for stress urinary incontinence (SUI) in which standardized UDS protocols were used. Secondary analyses of these UDS data showed that UDS were neither prognostic of treatment outcomes nor correlative with severity of UI symptoms, suggesting limited utility of UDS in the evaluation and management of the uncomplicated SUI patient. A third trial was designed to answer whether a basic office examination is not noninferior to UDS in affecting SUI surgical outcomes. The results of this study are currently in press. A fourth trial examined treatment of urgency urinary incontinence (UUI). Because UDS was not part of this trial, the utility of UDS in management and treatment of UUI could not be assessed. In summary, UDS will need to undergo further refinements to increase its clinical effectiveness in the area of urinary incontinence.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Albo ME, Richter HE, Brubaker L, et al. Burch colposuspension versus fascial sling to reduce urinary stress incontinence. N Engl J Med. 2007;356:2143–55.
Burgio KL, Kraus SR, Menefee S, et al. Behavioral therapy to enable women with urge incontinence to discontinue drug treatment: a randomized trial. Ann Intern Med. 2008;149:161–9.
Richter HE, Albo ME, Zyczynski HM, et al. Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med. 2010;362:2066–76.
• Nager CW, Brubaker L, Daneshgari F, et al. Design of the Value of Urodynamic Evaluation (ValUE) trial: A non-inferiority randomized trial of preoperative urodynamic investigations. Contemp Clin Trials. 2009;30:531–9. This paper is on the design of the ValUE trial, which compares basic office examination to UDS in uncomplicated SUI patients undergoing surgical treatment for their SUI.
• Steers W, Richter H, Nyberg L, et al. Challenges of conducting multi-center, multi-disciplinary urinary incontinence clinical trials: experience of the urinary incontinence treatment network. Neurourol Urodyn. 2009;28:170–6. This paper is a good overview of the UITN, although this publication was written at about the halfway point of the UITN existence.
Nager CW, Albo ME, Fitzgerald MP, et al. Process for development of multicenter urodynamic studies. Urology. 2007;69:63–7.
Nager CW, Albo ME, Fitzgerald MP, et al. Reference urodynamic values for stress incontinent women. Neurourol Urodyn. 2007;26:333–40.
Chai TC, Huang L, Kenton K, et al. Association of Baseline urodynamic measures of urethral function with clinical, demographic, and other urodynamic variables in women prior to undergoing midurethral sling surgery. Neurourol Urodyn. 2012;31:496–501.
Nager CW, FitzGerald M, Kraus SR, et al. Urodynamic measures do not predict stress continence outcomes after surgery for stress urinary incontinence in selected women. J Urol. 2008;179:1470–4.
Nager CW, Kraus SR, Kenton K, et al. Urodynamics, the supine empty bladder stress test, and incontinence severity. Neurourol Urodyn. 2010;29:1306–11.
Lemack GE, Krauss S, Litman H, et al. Normal preoperative urodynamic testing does not predict voiding dysfunction after Burch colposuspension versus pubovaginal sling. J Urol. 2008;180:2076–80.
Albo M, Wruck L, Baker J, et al. The relationships among measures of incontinence severity in women undergoing surgery for stress urinary incontinence. J Urol. 2007;177:1810–4.
Lemack GE, Xu Y, Brubaker L, et al. Clinical and demographic factors associated with Valsalva leak point pressure among women undergoing Burch bladder neck suspension or autologous rectus fascial sling procedures. Neurourol Urodyn. 2007;26:392–6.
Kirby AC, Nager CW, Litman HJ, et al. Perineal surface electromyography does not typically demonstrate expected relaxation during normal voiding. Neurourol Urodyn. 2011;30:1591–6.
Kirby AC, Nager CW, Litman HJ, et al. Preoperative voiding detrusor pressures do not predict stress incontinence surgery outcomes. Int Urogynecol J. 2011;22:657–63.
Kraus SR, Lemack GE, Richter HE, et al. Changes in urodynamic measures two years after Burch colposuspension or autologous sling surgery. Urology. 2011;78:1263–8.
Kraus S, Lemack G, Chai T, et al. Urodynamic changes 12 months after retropubic and transobturator midurethral slings. Presented at the American Urological Association Annual Meeting 2011 Apr. p. e864–e864. (Journal of Urology; vol. 185, no. 4).
Kraus SR, Lemack GE, Sirls LT, et al. Urodynamic changes associated with successful stress urinary incontinence surgery: is a little tension a good thing? Urology. 2011;78:1257–62.
•• Dmochowski R, Blaivas JM, Gormley EA, et al. Update of AUA guideline on the surgical management of female stress urinary incontinence. J Urol. 2010;183:1906–14. These are the AUA guidelines on surgical management of female SUI. These guidelines state that preoperative UDS is optional for female patients with uncomplicated SUI (documented by stress test) who plan to undergo surgical intervention.
Disclosure
Dr. Chai has received grant support from the National Institutes of Health, Endo Pharmaceutical, and Allergan; has had travel expenses covered/reimbursed by the National Institutes of Health; and has served as a consultant for Taris Biomedical.
Dr. Kraus has served as a consultant for Pfizer, Allergan, and Merck & Co., has received grant support from the NIDDK; and has received payment for development of educational presentations from Allergan and Laborie Medical.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chai, T.C., Kraus, S.R. Evaluation of Stress Predominant Urinary Incontinence. Curr Bladder Dysfunct Rep 7, 157–162 (2012). https://doi.org/10.1007/s11884-012-0140-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11884-012-0140-0