Abstract
Background
Posterior spinal instrumentation and fusion for correction of adolescent idiopathic scoliosis (AIS) typically requires lengthy operating time and may be associated with significant blood loss and subsequent transfusion. This study aimed to identify factors predictive of duration of surgery, intraoperative blood loss and transfusion requirements in an Irish AIS cohort.
Methods
A retrospective review of 77 consecutive patients with AIS who underwent single-stage posterior spinal instrumentation and fusion over a two-year period at two Dublin tertiary hospitals was performed. Data were collected prospectively and parameters under analysis included pre- and postoperative radiographic measurements, intraoperative blood loss, surgical duration, blood products required, laboratory blood values and perioperative complications.
Results
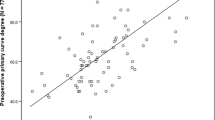
Mean preoperative primary curve Cobb angle was 62.3°; mean surgical duration was 5.6 h. The perioperative allogeneic red blood cell transfusion rate was 42.8 % with a median requirement of 1 unit. Larger curve magnitudes were positively correlated with longer fusion segments, increased operative time and greater estimated intraoperative blood loss. Preoperative Cobb angles greater than 70° [Relative Risk (RR) 4.42, p = 0.003] and estimated intraoperative blood loss greater than 1400 ml (RR 3.01, p = 0.037) were independent predictors of red blood cell transfusion risk.
Conclusion
Larger preoperative curve magnitudes in AIS increase operative time and intraoperative blood loss; preoperative Cobb angles greater than 70o and intraoperative blood loss greater than 1400 ml are predictive of red blood cell transfusion requirement in this patient group.
Similar content being viewed by others
References
Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA (2008) Adolescent idiopathic scoliosis. Lancet 371(9623):1527–1537
Bjerkreim I, Steen H, Brox JI (2007) Idiopathic scoliosis treated with Cotrel-Dubousset instrumentation: evaluation 10 years after surgery. Spine (Phila Pa 1976) 32(19):2103–2110
Helenius I, Remes V, Yrjonen T, Ylikoski M, Schlenzka D, Helenius M et al (2003) Harrington and Cotrel-Dubousset instrumentation in adolescent idiopathic scoliosis. Long-term functional and radiographic outcomes. J Bone Joint Surg Am 85-A(12):2303–2309
Lenke LG, Bridwell KH, Blanke K, Baldus C, Weston J (1998) Radiographic results of arthrodesis with Cotrel-Dubousset instrumentation for the treatment of adolescent idiopathic scoliosis. A five to ten-year follow-up study. J Bone Joint Surg Am 80(6):807–814
Luque ER (1982) Segmental spinal instrumentation for correction of scoliosis. Clin Orthop Relat Res 163:192–198
Storer SK, Vitale MG, Hyman JE, Lee FY, Choe JC, Roye DP Jr (2005) Correction of adolescent idiopathic scoliosis using thoracic pedicle screw fixation versus hook constructs. J Pediatr Orthop 25(4):415–419
Wang Y, Fei Q, Qiu G, Lee CI, Shen J, Zhang J et al (2008) Anterior spinal fusion versus posterior spinal fusion for moderate lumbar/thoracolumbar adolescent idiopathic scoliosis: a prospective study. Spine (Phila Pa 1976) 33(20):2166–2172
Zheng F, Cammisa FP Jr, Sandhu HS, Girardi FP, Khan SN (2002) Factors predicting hospital stay, operative time, blood loss, and transfusion in patients undergoing revision posterior lumbar spine decompression, fusion, and segmental instrumentation. Spine (Phila Pa 1976) 27(8):818–824
Edler A, Murray DJ, Forbes RB (2003) Blood loss during posterior spinal fusion surgery in patients with neuromuscular disease: is there an increased risk? Paediatr Anaesth 13(9):818–822
Nuttall GA, Horlocker TT, Santrach PJ, Oliver WC Jr, Dekutoski MB, Bryant S (2000) Predictors of blood transfusions in spinal instrumentation and fusion surgery. Spine (Phila Pa 1976) 25(5):596–601
Modi HN, Suh SW, Hong JY, Song SH, Yang JH (2010) Intraoperative blood loss during different stages of scoliosis surgery: a prospective study. Scoliosis 5:16
Shapiro F, Sethna N (2004) Blood loss in pediatric spine surgery. Eur Spine J 13(Suppl 1):S6–S17
Triulzi DJ, Vanek K, Ryan DH, Blumberg N (1992) A clinical and immunologic study of blood transfusion and postoperative bacterial infection in spinal surgery. Transfusion 32(6):517–524
Triulzi DJ (2009) Transfusion-related acute lung injury: current concepts for the clinician. Anesth Analg 108(3):770–776
Guay J, de Moerloose P, Lasne D (2006) Minimizing perioperative blood loss and transfusions in children. Can J Anaesth 53(6 Suppl):S59–S67
Hassan N, Halanski M, Wincek J, Reischman D, Sanfilippo D, Rajasekaran S et al (2011) Blood management in pediatric spinal deformity surgery: review of a 2-year experience. Transfusion 51(10):2133–2141
van Popta D, Stephenson J, Patel D, Verma R (2014) The pattern of blood loss in adolescent idiopathic scoliosis. Spine J 14(12):2938–2945
Verma RR, Williamson JB, Dashti H, Patel D, Oxborrow NJ (2006) Homologous blood transfusion is not required in surgery for adolescent idiopathic scoliosis. J Bone Joint Surg Br 88(9):1187–1191
Bowen RE, Gardner S, Scaduto AA, Eagan M, Beckstead J (2010) Efficacy of intraoperative cell salvage systems in pediatric idiopathic scoliosis patients undergoing posterior spinal fusion with segmental spinal instrumentation. Spine (Phila Pa 1976) 35(2):246–251
Bess RS, Lenke LG (2006) Blood loss minimization and blood salvage techniques for complex spinal surgery. Neurosurg Clin N Am 17(3):227–234
Xu C, Wu A, Yue Y (2012) Which is more effective in adolescent idiopathic scoliosis surgery: batroxobin, tranexamic acid or a combination? Arch Orthop Trauma Surg 132(1):25–31
Shapiro F, Zurakowski D, Sethna NF (2007) Tranexamic acid diminishes intraoperative blood loss and transfusion in spinal fusions for duchenne muscular dystrophy scoliosis. Spine (Phila Pa 1976) 32(20):2278–2283
Yang B, Li H, Wang D, He X, Zhang C, Yang P (2013) Systematic review and meta-analysis of perioperative intravenous tranexamic acid use in spinal surgery. PLoS One 8(2):e55436
Guay J, Haig M, Lortie L, Guertin MC, Poitras B (1994) Predicting blood loss in surgery for idiopathic scoliosis. Can J Anaesth 41(9):775–781
Ialenti MN, Lonner BS, Verma K, Dean L, Valdevit A, Errico T (2013) Predicting operative blood loss during spinal fusion for adolescent idiopathic scoliosis. J Pediatr Orthop 33(4):372–376
Yu X, Xiao H, Wang R, Huang Y (2013) Prediction of massive blood loss in scoliosis surgery from preoperative variables. Spine (Phila Pa 1976) 38(4):350–355
Koerner JD, Patel A, Zhao C, Schoenberg C, Mishra A, Vives MJ et al (2014) Blood loss during posterior spinal fusion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 39(18):1479–1487
Cahill PJ, Pahys JM, Asghar J, Yaszay B, Marks MC, Bastrom TP et al (2014) The effect of surgeon experience on outcomes of surgery for adolescent idiopathic scoliosis. J Bone Joint Surg Am 96(16):1333–1339
Ryan KM, O’Brien K, Regan I, O’Byrne JM, Moore D, Kelly PM et al (2013) The prevalence of abnormal preoperative coagulation tests in pediatric patients undergoing spinal surgery for scoliosis. Spine J. doi:10.1016/j.spinee.2013.07.460
Stanitski CL, Whittlesey G, Thompson I, Stanitski DF, Mohan A (1998) Clotting parameters in patients with adolescent idiopathic scoliosis undergoing posterior spinal fusion and instrumentation. J Pediatr Orthop B 7(2):132–134
Fox HJ, Thomas CH, Thompson AG (1997) Spinal instrumentation for Duchenne’s muscular dystrophy: experience of hypotensive anaesthesia to minimise blood loss. J Pediatr Orthop 17(6):750–753
Copley LA, Richards BS, Safavi FZ, Newton PO (1999) Hemodilution as a method to reduce transfusion requirements in adolescent spine fusion surgery. Spine (Phila Pa 1976) 24(3):219–222 Discussion 23–4
Neilipovitz DT (2004) Tranexamic acid for major spinal surgery. Eur Spine J 13(Suppl 1):S62–S65
Weiss JM, Skaggs D, Tanner J, Tolo V (2007) Cell Saver: is it beneficial in scoliosis surgery? J Child Orthop 1(4):221–227
Al-Mahfoudh R, Qattan E, Ellenbogen JR, Wilby M, Barrett C, Pigott T (2014) Applications of the ultrasonic bone cutter in spinal surgery—our preliminary experience. Br J Neurosurg 28(1):56–60
Bartley CE, Bastrom TP, Newton PO (2014) Blood loss reduction during surgical correction of adolescent idiopathic scoliosis utilizing an ultrasonic bone scalpel. Spine Deform 2:285–290
Hu X, Ohnmeiss DD, Lieberman IH (2013) Use of an ultrasonic osteotome device in spine surgery: experience from the first 128 patients. Eur Spine J 22(12):2845–2849
Miyanji F, Slobogean GP, Samdani AF, Betz RR, Reilly CW, Slobogean BL et al (2012) Is larger scoliosis curve magnitude associated with increased perioperative health-care resource utilization?: a multicenter analysis of 325 adolescent idiopathic scoliosis curves. J Bone Joint Surg Am 94(9):809–813
Acknowledgments
The authors are very grateful to the National Children’s Research Centre, Dublin 12, Ireland, for funding this study. They thank Ms. Gloria Crispino-O’Connell for providing statistical support, and acknowledge the assistance of the staff at Our Lady’s Children’s Hospital Crumlin and the Blackrock Clinic throughout the study. This study was exclusively funded by The National Children’s Research Centre, Crumlin, Dublin 12, Ireland.
Conflict of interest
None.
Ethical standard
This study was approved by the Ethics Committees of Our Lady’s Children’s Hospital Crumlin, Dublin 12, Ireland and the Blackrock Clinic, Co. Dublin, Ireland.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nugent, M., Tarrant, R.C., Queally, J.M. et al. Influence of curve magnitude and other variables on operative time, blood loss and transfusion requirements in adolescent idiopathic scoliosis. Ir J Med Sci 185, 513–520 (2016). https://doi.org/10.1007/s11845-015-1306-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-015-1306-5