Abstract
Background
The clinical spectrum of adult coeliac disease (ACD) is varied with limited Irish data.
Aims and Objectives
The aim of this study was to analyse the presenting symptoms, associated conditions and complications in a consecutive series of patients with ACD.
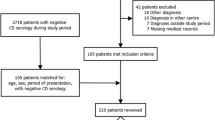
Methods
Data were obtained from database on patients with ACD between 1988 and 2004.
Results
One hundred and six patients (69F:37M, mean age: 46, range: 23–95 years) were included. The modes of presentation were diarrhoea in 44 patients (45%), weight loss in 41 (42%), anaemia in 37 (38%), abdominal pain in 15 (15%), fatigue in 8 (8%), hypocalcaemia in 4 (4%) and steatorrhoea in 4 (4%). Associated conditions included thyroid disorders in 7 patients (7%), bipolar affective disorder in 4 (4%), major depression in 3 (3%), rheumatoid disease in 3 (3%), inflammatory bowel disease in 4 (4%) and type I diabetes mellitus in 2 (2%). Malignancy emerged as a major complication in 15 patients (15%)
Conclusion
The presenting features of ACD are diverse and associated with high risk of malignancy.


Similar content being viewed by others
References
Kennedy NP, Feighery C (2009) Clinical features of coeliac disease today. Biomed Pharmacother 54(7):373–380
Aziz I, Evans K, Papageorgiou V et al (2011) Are patients with coeliac disease seeking alternative therapies to gluten free diet? J Gastrointestin Liver Dis 20(1):27–31
Green PHR, Stavropoulos SN, Panagi SG et al (2001) Characteristics of adult celiac disease in the USA: results of a national survey. Am J Gastroenterol 96(1):126–131
Feighery C (1999) Fortnightly review: coeliac disease. BMJ 319(7204):236–239
Gasbarrini G, Malandrino N, Giorgio V et al (2008) Celiac disease: what’s new about it? Dig Dis 26(2):121–127
Green PH, Fleischauer AT, Bhagat G et al (2003) Risk of malignancy in patients with celiac disease. Am J Med 115(3):191–195
Lombardo T, Ximenes B, Ferro G (2006) Hypochromic microcytic anemia as a clinical presentation of celiac disease. Clin Lab 52(5–6):231–236
Ransford RA, Hayes M, Palmer M et al (2002) A controlled, prospective screening study of celiac disease presenting as iron deficiency anemia. J Clin Gastroenterol 35(3):228–233
De Freitas IN, Sipahi AM, Damiao AO et al (2002) Celiac disease in Brazilian adults. J Clin Gastroenterol 34(4):430–434
Ciacci C, Cirillo M, Sollazzo R et al (1995) Gender and clinical presentation in adult celiac disease. Scand J Gastroenterol 30(11):1077–1081
Sachdev A, Srinivasan V, Maheswary S et al (2002) Adult onset celiac disease in North India. Trop Gastroenterol 23(3):117–119
McElvaney NG, Duignan R, Fielding JF (1992) Coeliac disease: clinical presentations, correlations of dietary compliance, symptomatic response and repeat biopsy findings. Ulster Med J 61(2):134–138
Hankey GL, Holmes GK (1994) Coeliac disease in the elderly. Gut 35(1):65–67
Rampertab SD, Pooran N, Brar P et al (2006) Trends in the presentation of celiac disease. Am J Med 119(4):355.e9–14
Freeman HJ (1998) Survey of gastroenterologists on the diagnosis and treatment of adult patients with celiac disease in British Columbia. Can J Gastroenterol 12(2):149–152
Brar P, Kwon GY, Egbuna II et al (2007) Lack of correlation of degree of villous atrophy with severity of clinical presentation of coeliac disease. Dig Liv Dis 39(1):26–29
Murray JA, Rubio-Tapia A, Van Dyke CT et al (2008) Mucosal atrophy in celiac disease: extent of involvement, correlation with clinical presentation, and response to treatment. Clin Gastroenterol Hepatol 6(2):186–193
Rubio-Tapia A, Murray JA (2007) The liver in celiac disease. Hepatology 46(5):1650–1658
Dewar DH, Ciclitria PJ (2005) Clinical features and diagnosis of celiac disease. Gastroenterology 128(4 Suppl 1):S19–S24
Abdo A, Meddings J, Swain M (2004) Liver abnormalities in celiac disease. Clin Gastroenterol Hepatol 2(2):107–112
Bardella MT, Vecchi M, Conte D et al (1992) Chronic unexplained hypertransaminasemia may be caused by occult celiac disease. Hepatology 29(3):654–657
Volta U, De Franceschi L, Lari F et al (1998) Coelic disease hidden by cryptogenic hypertransaminasaemia. Lancet 325(9121):26–29
Mahmud FH, Murray JA, Kudva YC et al (2005) Celiac disease in type 1 diabetes mellitus in a North American community: prevalence, serologic screening, and clinical features. Mayo Clin Proc 80(11):1429–1434
Gasbarrini G, Ciccocioppo R, De Vitis I et al (2001) Coeliac disease in the elderly. A multicentre Italian study. Gerontology 47(6):306–310
Tursi A, Giorgetti G, Brandimarte G et al (2001) Prevalence and clinical presentation of subclinical/silent celiac disease in adults: an analysis on a 12 year observation. Hepatogastroenterology 48(38):462–464
Cuoco L, Certo M, Jorizzo RA et al (1999) Prevalence and early diagnosis of coeliac disease in autoimmune disorders. Ital J Gastroenterol Hepatol 31(4):283–287
Holmes GK (1996) Non malignant complications of coeliac disease. Acta Paediatr Suppl 412:68–75
Addolorato G, Leggio L, D’Angelo C et al (2008) Affective and psychiatric disorders in celiac disease. Dig Dis 26(2):140–148
Askling J, Linet M, Gridley G et al (2002) Cancer incidence in a population- based cohort of individuals hospitalized with celiac disease or dermatitis herpetiformis. Gastroenterology 123(5):1428–1435
Farrell RJ, Kelly CP (2002) Coeliac Sprue. N Engl J Med 346(3):180–187
Ryan BM, Kelleher D (2000) Refractory celiac disease. Gastroenterology 119(1):243–251
Holmes GK (2002) Coeliac disease and malignancy. Dig Liver Dis 34(3):229–237
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saleem, A., Connor, H.J.O. & Regan, P.O. Adult coeliac disease in Ireland: a case series. Ir J Med Sci 181, 225–229 (2012). https://doi.org/10.1007/s11845-011-0788-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-011-0788-z