Abstract
Background
Congestive heart failure patients with reduced left ventricular ejection fraction (HFrEF) and sleep-disordered breathing (SDB) are at an increased risk of nocturnal cardiac arrhythmias. SDB can be effectively treated with adaptive servo-ventilation (ASV). Therefore, we tested the hypothesis that ASV therapy reduces nocturnal arrhythmias and heart rate in patients with HFrEF and SDB.
Methods
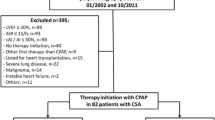
In a non-prespecified subanalysis of a multicenter randomized controlled trial (ISRCTN04353156), 20 consecutive patients with stable HFrEF (age 67 ± 9 years; left ventricular ejection fraction, LVEF 32 ± 7 %) and SDB (apnea–hypopnea index, AHI 48 ± 20/h) were randomized to either an ASV therapy (n = 10) or an optimal medical treatment alone group (controls, n = 10). Polysomnography (PSG) with blinded centralized analysis and scoring was performed at baseline and at 12 weeks. The electrocardiograms (ECG) of the PSGs were analyzed with long-term (24-h) Holter ECG software (QRS-Card™ Cardiology Suite; Pulse Biomedical Inc., King of Prussia, PA, USA).
Results
There was a decrease in ventricular extrasystoles (VES) per hour of recording time in the ASV group compared to the control group (−8.1 ± 42.4 versus +9.8 ± 63.7/h, p = 0.356). ASV reduced the number of ventricular couplets and nonsustained ventricular tachycardias (nsVT) compared to the control group (−2.3 ± 6.9 versus +2.1 ± 12.7/h, p = 0.272 and −0.1 ± 0.5 versus +0.1 ± 1.1/h, p = 0.407, respectively). Mean nocturnal heart rate decreased in the ASV group compared to the controls (−2.0 ± 2.7 versus +3.9 ± 11.5/min, p = 0.169). The described changes were not significantly different between the groups.
Conclusion
In HFrEF patients with SDB, ASV treatment may reduce nocturnal VES, couplets, nsVT, and mean nocturnal heart rate. The findings of the present pilot study underscore the need for further analyses in larger studies.
Zusammenfassung
Hintergrund
Patienten mit chronischer Herzinsuffizienz und reduzierter linksventrikulärer Ejektionsfraktion (HFrEF) und schlafbezogenen Atmungsstörungen (SBAS) leiden häufig unter nächtlich auftretenden kardialen Arrhythmien. SBAS können effektiv mit einer adaptiven Servoventilation (ASV) behandelt werden. Wir überprüften daher die Hypothese, dass eine ASV-Therapie bei Patientenmit HFrEF und SBAS die Häufigkeit nächtlicher kardialer Arrhythmien und die Herzfrequenz reduziert.
Methoden
In einer nicht-präspezifizierten Subanalyse einer multizentrischen randomisierten Studie (ISRCTN04353156) wurden 20 Patienten mit stabiler HFrEF (Alter 67 ± 9 J; linksventrikulärer Ejektionsfraktion 32 ± 7 %) und SBAS (Apnoe-Hypopnoe-Index, AHI 48 ± 20/h) entweder einer ASV- (n = 10; Philips Respironics, Murrysville, PA, USA) oder einer Kontrollgruppe mit alleiniger optimaler Herzinsuffizienztherapie (n = 10) zugeteilt. Zu Beginn der Studie und nach 12 Wochen wurde jeweils eine Polysomnographie (PSG) mit zentraler verblindeter Auswertung durchgeführt. Die Elektrokardiogramme (EKG) der PSG wurden mit Unterstützung einer Langzeit-EKG-Software (Pulse Biomedical Inc., QRS-CardTM Cardiology Suite, USA) ausgewertet.
Ergebnisse
In der ASV-Gruppe nahmen ventrikuläre Extrasystolen (VES) pro Stunde Aufnahmezeit im Vergleich zur Kontrollgruppe ab (−8,1 ± 42,4 versus +9,8 ± 63,7/h, p = 0,356). Eine ASV-Therapie reduziert im Vergleich mit der Kontrollgruppe die Anzahl ventrikulärer Couplets (−2,3 ± 6,9 versus +2,1 ± 12,7/h, p = 0,272) sowie nichtanhaltender ventrikulärer Tachykardien (nsVT, −1,2 ± 3,9 versus +1,3 ± 8,7, p = 0,340). Die mittlere nächtliche Herzfrequenz sank in der ASV-Gruppe im Vergleich zur Kontrollgruppe (−2,0 ± 2,7 versus +3,9 ± 11,5/Minute, p = 0,169). Die Veränderungen waren jeweils nicht statistisch signifikant.
Schlussfolgerungen
Eine Beatmungstherapie mit ASV reduziert bei Patienten mit HFrEF und SBAS möglicherweise die Häufigkeit nächtlicher VES, ventrikulärer Couplets, nsVTs und die nächtlichemittlere Herzfrequenz. Die Ergebnisse der vorliegenden Pilotstudie unterstreichen die Notwendigkeit, diese Fragestellung in größeren Studien zu evaluieren.




Similar content being viewed by others
References
Arzt M, Schroll S, Series F et al (2013) Auto-servoventilation in heart failure with sleep apnoea: a randomised controlled trial. Eur Respir J 42(5):1244–1254. doi:10.1183/09031936.00083312
Arzt M, Wensel R, Montalvan S et al (2008) Effects of dynamic bilevel positive airway pressure support on central sleep apnea in men with heart failure. Chest 134(1):61–66. doi:10.1378/chest.07-1620
Arzt M, Woehrle H, Oldenburg O et al (2016) Prevalence and predictors of sleep-disordered breathing in patients with stable chronic heart failure: the SchlaHF registry. JACC Heart Fail 4(2):116–125. doi:10.1016/j.jchf.2015.09.014
Bitter T, Faber L, Hering D et al (2009) Sleep-disordered breathing in heart failure with normal left ventricular ejection fraction. Eur J Heart Fail 11(6):602–608. doi:10.1093/eurjhf/hfp057
Bitter T, Gutleben K, Nölker G et al (2013) Treatment of Cheyne-stokes respiration reduces Arrhythmic events in chronic heart failure. J Cardiovasc Electrophysiol. doi:10.1111/jce.12197
Bitter T, Westerheide N, Prinz C et al (2011) Cheyne-Stokes respiration and obstructive sleep apnoea are independent risk factors for malignant ventricular arrhythmias requiring appropriate cardioverter-defibrillator therapies in patients with congestive heart failure. Eur Heart J 32(1):61–74. doi:10.1093/eurheartj/ehq327
Cowie MR, Woehrle H, Wegscheider K et al (2015) Adaptive servo-ventilation for central sleep apnea in systolic heart failure. N Engl J Med 373(12):1095–1105. doi:10.1056/NEJMoa1506459
Damy T, Margarit L, Noroc A et al (2012) Prognostic impact of sleep-disordered breathing and its treatment with nocturnal ventilation for chronic heart failure. Eur J Heart Fail 14(9):1009–1019. doi:10.1093/eurjhf/hfs085
Dickstein K, Cohen-Solal A, Filippatos G et al (2008) ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008. Eur J Heart Fail 10(10):933–989. doi:10.1016/j.ejheart.2008.08.005
Fox H, Bitter T, Gutleben K et al (2014) Cardiac or other Implantable electronic devices and sleep-disordered breathing – implications for diagnosis and therapy. Arrhythm Electrophysiol Rev 3(2):116–119. doi:10.15420/aer.2014.3.2.116
Gertsch M (2008) Das EKG. Auf einen Blick und im Detail, 2nd edn. Springer, Heidelberg
Gottlieb DJ, Yenokyan G, Newman AB et al (2010) Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation 122(4):352–360. doi:10.1161/CIRCULATIONAHA.109.901801
Iber C, American Academy of Sleep Medicine (2007) Das AASM-Manual zum Scoring von Schlaf und assoziierten Ereignissen. Steinkopff, Heidelberg
Javaheri S, Parker TJ, Liming JD et al (1998) Sleep apnea in 81 ambulatory male patients with stable heart failure. Types and their prevalences, consequences, and presentations. Circulation 97(21):2154–2159
Javaheri S (2000) Effects of continuous positive airway pressure on sleep apnea and ventricular irritability in patients with heart failure. Circulation 101(4):392–397. doi:10.1161/01.CIR.101.4.392
Jessup M, Brozena S (2003) Heart failure. N Engl J Med 348(20):2007–2018. doi:10.1056/NEJMra021498
Jilek C, Krenn M, Sebah D et al (2011) Prognostic impact of sleep disordered breathing and its treatment in heart failure: an observational study. Eur J Heart Fail 13(1):68–75. doi:10.1093/eurjhf/hfq183
Kasai T, Usui Y, Yoshioka T et al (2010) Effect of flow-triggered adaptive servo-ventilation compared with continuous positive airway pressure in patients with chronic heart failure with coexisting obstructive sleep apnea and Cheyne-Stokes respiration. Circ Heart Fail 3(1):140–148. doi:10.1161/CIRCHEARTFAILURE.109.868786
Lanfranchi PA, Somers VK, Braghiroli A et al (2003) Central sleep apnea in left ventricular dysfunction: prevalence and implications for arrhythmic risk. Circulation 107(5):727–732
Malhotra A, Patil S, Sands S et al (2015) Central sleep apnoea in congestive heart failure. Lancet Respir Med 3(7):507–508. doi:10.1016/S2213-2600(15)00235-0
Mehra R, Redline S (2014) Arrhythmia risk associated with sleep disordered breathing in chronic heart failure. Curr Heart Fail Rep 11(1):88–97. doi:10.1007/s11897-013-0171-7
Mehra R, Stone KL, Varosy PD et al (2009) Nocturnal Arrhythmias across a spectrum of obstructive and central sleep-disordered breathing in older men: outcomes of sleep disorders in older men (MrOS sleep) study. Arch Intern Med 169(12):1147–1155. doi:10.1001/archinternmed.2009.138
Mosterd A, Hoes AW (2007) Clinical epidemiology of heart failure. Heart 93(9):1137–1146. doi:10.1136/hrt.2003.025270
Neumann T, Biermann J, Erbel R et al (2009) Heart failure: the commonest reason for hospital admission in Germany: medical and economic perspectives. Dtsch Arztebl Int 106(16):269–275. doi:10.3238/arztebl.2009.0269
Oldenburg O, Lamp B, Faber L et al (2007) Sleep-disordered breathing in patients with symptomatic heart failure: a contemporary study of prevalence in and characteristics of 700 patients. Eur J Heart Fail 9(3):251–257. doi:10.1016/j.ejheart.2006.08.003
Priefert H (2016) Effekte einer Adaptiven Servo-Ventilation auf Herzrhythmusstörungen bei Patienten mit chronischer Herzinsuffizienz und schlafbezogenen Atmungsstörungen – Subanalyse einer randomisierten Studie. Inaugural. Universität Regensburg, Regensburg (Dissertation)
Priefert H‑J, Hetzenecker A, Escourrou P, Luigart R, Series F, Lewis K, Benjamin A, Birner C, Pfeifer M, Arzt M (2014) Effekte einer adaptiven Servoventilation auf Herzrhythmusstörungen bei Patienten mit chronischer Herzinsuffizienz und schlafbezogenen Atmungsstörungen – eine randomisierte Pilotstudie. 22. Jahrestagung der DGSM, Köln, 4.–6. Dezember 2014. vol. Abstract Nr. 73. (Somnologie 18(1): 27. doi:10.1007/s11818-014-0691-8)
Redfield MM, Jacobsen SJ, Burnett JC et al (2003) Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA 289(2):194–202
Ryan CM, Juvet S, Leung R et al (2008) Timing of nocturnal ventricular ectopy in heart failure patients with sleep apnea. Chest 133(4):934–940. doi:10.1378/chest.07-2595
Ryan CM, Usui K, Floras JS et al (2005) Effect of continuous positive airway pressure on ventricular ectopy in heart failure patients with obstructive sleep apnoea. Thorax 60(9):781–785. doi:10.1136/thx.2005.040972
Schäfer A, Brinker A, Schriever U (2016) Adaptive servo-ventilation for central sleep apnea in heart failure. N Engl J Med 374(7):689–690. doi:10.1056/NEJMc1515007#SA6
Schulz R, Blau A, Börgel J et al (2007) Sleep apnoea in heart failure. Eur Respir J 29(6):1201–1205. doi:10.1183/09031936.00037106
Wang H, Parker JD, Newton GE et al (2007) Influence of obstructive sleep apnea on mortality in patients with heart failure. J Am Coll Cardiol 49(15):1625–1631. doi:10.1016/j.jacc.2006.12.046
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was supported by Philips Respironics. M. Arzt receives financial support for research activities from Philips Respironics, ResMed, and the ResMed Foundation, as well as speaker honoraria from Philips Respironics and ResMed. Prior to its current publication in this journal, this work was submitted by the first author to the Faculty of Medicine, University of Regensburg, in the form of a dissertation. H.-J. Priefert, A. Hetzenecker, P. Escourrou, R. Luigart, F. Series, K. Lewis, A. Benjamin, C. Birner and M. Pfeifer declare that they have no conflicts of interest.
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Additional information
The German version of this Article can be found under doi:10.1007/s11818-016-0059-3. Please refer there for the Clinical Trial Registration.
Rights and permissions
About this article
Cite this article
Priefert, HJ., Hetzenecker, A., Escourrou, P. et al. Effects of adaptive servo-ventilation on ventricular arrhythmias in patients with stable congestive heart failure and sleep-disordered breathing. Somnologie 21 (Suppl 1), 19–27 (2017). https://doi.org/10.1007/s11818-016-0072-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11818-016-0072-6
Keywords
- Heart failure
- Sleep-disordered breathing
- Adaptive servo-ventilation
- Cardiac arrhythmias
- Sudden cardiac death