Abstract
The concept inflammatory bowel diseases (IBD, CED) includes ulcerative colitis (UC) and Crohn's disease (CD). Both diseases are chronic with remissions and relapses over years. Symptoms include abdominal cramps and pain, diarrhea, weight loss and bleeding from the intestines. CD usually causes ulcers in the ileocoecal area, but any part of the gut may be affected. Some have fistula to the skin or surrounding organs. In ulcerative colitis diffuse ulcerations in the rectum are typical, but also to a variable degree more proximal sites may be affected. The aetiology is unknown. Type of drug treatment depends on disease activity. Commonly used drugs include 5-ASA drugs, corticosteroids and immune inhibiting drugs (e. g. azathioprin, methotrexat, ciclosporin, infliximab). Both steroids and infliximab may provoke psychiatric symptoms, most often anxiety or depression. Methotrexat may increase lithium concentration, but pharmacodynamic interactions with other psychotropics are not frequently seen.
Perceived life stress may influence the course of IBD negatively, and the prevalence of mental disorders is slightly above the frequency reported in population studies. However, there is no empirical evidence supporting the view that IBD is a psychosomatic disorder in the traditional meaning of the word. Patients with IBD should be evaluated with regard to the presence of perceived major life stress and mental disorders. Psychiatric treatment should follow regular guidelines. There is no evidence to support a view that patients with IBD should routinely receive psychotherapy.
Zusammenfassung
Zu den chronisch entzündlichen Darmerkrankungen (CED) gehören die Colitis ulcerosa (UC) und der Morbus Crohn (CD). Kennzeichen dieser entzündlichen Erkrankungen des Intestinaltraktes bisher unbekannter Ursache ist ein chronischer, meist rezidivierender Verlauf. Zu den Symptomen gehören Bauchschmerzen und -krämpfe, Durchfälle, Gewichtsabnahme und Blutverlust aus dem Darm. Beim Morbus Crohn, der alle Abschnitte des Gastrointestinaltraktes befallen kann, finden sich häufig Ulzera am Übergang zwischen Dünn- und Dickdarm. Bei einigen Patienten entstehen Fisteln zwischen Darmabschnitten, zu nahe liegenden Organen oder zur Haut. Bei der Colitis ulcerosa, die meist im Rektum beginnt und sich variierend nach proximal ausbreitet, entstehen diffuse und kontinuierliche Schleimhautulzerationen. Die somatische Behandlung ist abhängig von der Krankheitsaktivität und beinhaltet 5-Aminosalicylate (5-ASA), Kortikosteroide und Immunsuppressiva (Azathioprin, Methotrexat, Ciclosporin, Infliximab). Sowohl die Glukokortikoide als auch Tumornekrosefaktor-Alpha-Antikörper (Infliximab) können zu psychischen und psychiatrischen Nebenwirkungen führen, am häufigsten Angst und Depressionen bzw. Manie. Außer der Erhöhung der Lithiumkonzentration durch Methotrexat sind ernsthafte Interaktionen mit Psychopharmaka selten.
Es gibt Anhaltspunkte für eine negative Auswirkung auf den Krankheitsverlauf durch subjektiv erlebten Stress und für ein etwas häufigeres Vorkommen psychischer Störungen als in der Normalbevölkerung. Gesicherte Nachweise für die Zuordnung der chronisch entzündlichen Darmerkrankungen zu psychosomatischen Erkrankungen im traditionellen Verständnis sind nicht gegeben. Unter Experten besteht Konsens, Patienten mit diesen Erkrankungen bei Vorhandensein chronischer Stressbelastungen oder eventuellen psychischen Störungen eine Behandlung anzubieten. Die Therapie erfolgt nach den üblichen Behandlungsleitlinien. Alle Psychopharmaka können eingesetzt werden. Eine Lithiumbehandlung ist schwer zu kontrollieren. Demgegenüber gibt es keine ausreichenden Hinweise, routinemäßig den betroffenen Patienten eine psychodynamische oder andere Form von Psychotherapie anzubieten.
Similar content being viewed by others
Literatur
Addolorato G, Capristo E, Stefanini GF, Gasbarrini G (1997) Inflammatory bowel disease: a study of the association between anxiety and depression, physical morbidity, and nutritional status. Scand J Gastroenterol 32:1013–1021
Alexander F (1952) Emotional factors in gastrointestinal disturbances. In: Alexander F (ed) Psychosomatic medicine. Its principles and applications. Norton, New York
Andrews H, Barczak P, Allan RN (1987) Psychiatric illness in patients with inflammatory bowel disease. Gut 28:1600–1604
Bellini M, Tansella M (1976) Obsessional scores and subjective general psychiatric complaints of patients with duodenal ulcer or ulcerative colitis. Psychol Med 6:461–467
Bernklev T, Jahnsen J, Schulz T et al. (2005) Course of disease, drug treatment and health-related quality of life in patients with inflammatory bowel disease 5 years after initial diagnosis. Eur J Gastroenterol Hepatol 17:1037–1045
Bernklev T, Jahnsen J, Aadland E et al. (2004) Health-related quality of life in patients with inflammatory bowel disease five years after the initial diagnosis. Scand J Gastroenterol 39:365–373
Bitton A, Sewitch MJ, Peppercorn MA, deB Edwardes MD, Shah S, Ransil B, Locke SE (2003) Psychosocial determinants of relapse in ulcerative colitis: a longitudinal study. Am J Gastroenterol 98:2203–2208
Brustolim D, Ribeiro-dos-Santos R, Kast RE, Altschuler EL, Soares MB (2006) A new chapter opens in anti-inflammatory treatments: the antidepressant bupropion lowers production of tumor necrosis factor-alpha and interferon-gamma in mice. Int Immunopharmacol 6:903–907
Candy S, Wright J, Gerber M, Adams G, Gerig M, Goodman R (1995) A controlled double blind study of azathioprine in the management of Crohn's disease. Gut 37:674–678
Caprilli R, Gassull MA, Escher JC et al. (2006) European evidence based consensus on the diagnosis and management of Crohn's disease: special situations. Gut 55, Suppl 1:i36-i58
Casati J, Toner BB, de Rooy EC, Drossman DA, Maunder RG (2000) Concerns of patients with inflammatory bowel disease: a review of emerging themes. Dig Dis Sci 45:26–31
Drossman DA, Leserman J, Li ZM, Mitchell CM, Zagami EA, Patrick DL (1991) The rating form of IBD patient concerns: a new measure of health status. Psychosom Med 53:701–712
Engel GL (1955) Studies of ulcerative colitis. III. The nature of the psychologic processes. Am J Med 19:231–256
Farrokhyar F, Marshall JK, Easterbrook B, Irvine EJ (2006) Functional gastrointestinal disorders and mood disorders in patients with inactive inflammatory bowel disease: prevalence and impact on health. Inflamm Bowel Dis 12:38–46
Fuller-Thomson E, Sulman J (2006) Depression and inflammatory bowel disease: findings from two nationally representative Canadian surveys. Inflamm Bowel Dis 12:697–707
Garcia-Vega E, Fernandez-Rodriguez C (2004) A stress management programme for Crohn's disease. Behav Res Ther 42:367–383
Goldstein ET, Preskorn SH (1989) Mania triggered by a steroid nasal spray in a patient with stable bipolar disorder. Am J Psychiatry 146:1076–1077
Gomez-Gil E, Vidal A, Panes J, Jaen J, Peri JM, Fernandez-Egea E, Pique JM (2003) Relationship between patient's subjective stress perception and the course of inflammatory bowel disease. Gastroenterol Hepatol 26:411–416
Guthrie E, Jackson J, Shaffer J, Thompson D, Tomenson B, Creed F (2002) Psychological disorder and severity of inflammatory bowel disease predict health-related quality of life in ulcerative colitis and Crohn's disease. Am J Gastroenterol 97:1994–1999
Hampe J, Grebe J, Nikolaus S et al. (2002) Association of NOD2 (CARD 15) genotype with clinical course of Crohn's disease: a cohort study. Lancet 359 (9318):1661–1665
Han SW, McColl E, Barton JR, James P, Steen IN, Welfare MR (2005) Predictors of quality of life in ulcerative colitis: the importance of symptoms and illness representations. Inflamm Bowel Dis 11:24–34
Hyphantis TN, Triantafillidis JK, Pappa S et al. (2005) Defense mechanisms in inflammatory bowel disease. J Gastroenterol 40:24–30
Jantschek G, Zeitz M, Pritsch M et al. (1998) Effect of psychotherapy on the course of Crohn's disease.Results of the German prospective multicenter psychotherapy treatment study on Crohn's disease. German Study Group on Psychosocial Intervention in Crohn's Disease. Scand J Gastroenterol 33:1289–1296
Keller W, Pritsch M, Von Wietersheim J et al.(2004) Effect of psychotherapy and relaxation on the psychosocial and somatic course of Crohn's disease: main results of the German Prospective Multicenter Psychotherapy Treatment study on Crohn's Disease. J Psychosom Res 56:687–696
Kennedy AP, Nelson E, Reeves D et al. (2004) A randomised controlled trial to assess the effectiveness and cost of a patient orientated self management approach to chronic inflammatory bowel disease. Gut 53:1639–1645
Krauthammer C, Klerman GL (1978) Secondary mania: manic syndromes associated with antecedent physical illness or drugs. Arch Gen Psychiatry 35:1333–1339
Kurina LM, Goldacre MJ, Yeates D, Gill LE (2001) Depression and anxiety in people with inflammatory bowel disease. J Epidemiol Community Health 55:716–720
Levenstein S, Prantera C, Varvo V, Scribano ML, Berto E, Andreoli A, Luzi C (1994) Psychological stress and disease activity in ulcerative colitis: a multidimensional cross-sectional study. Am J Gastroenterol 89:1219–1225
Levenstein S, Prantera C, Varvo V et al. (2000) Stress and exacerbation in ulcerative colitis: a prospective study of patients enrolled in remission. Psychological stress and disease activity in ulcerative colitis: a multidimensional cross-sectional study. Am J Gastroenterol 95:1213–1220
Li J, Norgard B, Precht DH, Olsen J (2004) Psychological stress and inflammatory bowel disease: a follow-up study in parents who lost a child in Denmark. Am J Gastroenterol 99:1129–1133
Mardini HE, Kip KE, Wilson JW (2004) Crohn's disease: a two-year prospective study of the association between psychological distress and disease activity. Dig Dis Sci 49:492–497
Maunder RG, Lancee WJ, Greenberg GR, Hunter JJ, Fernandes BJ (2000) Insecure attachment in a subgroup with ulcerative colitis defined by ANCA status. Dig Dis Sci 45:2127–2132
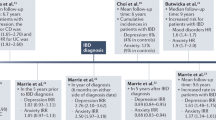
Maunder RG, Lancee WJ, Hunter JJ, Greenberg GR, Steinhart AH (2005) Attachment insecurity moderates the relationship between disease activity and depressive symptoms in ulcerative colitis. Inflamm Bowel Dis 11:919–926
Maunder RG, Greenberg GR, Hunter JJ, Lancee WJ, Steinhart AH, Silverberg MS (2006) Psychobiological Subtypes of Ulcerative Colitis: pANCA Status moderates the relationship between Disease Activity and Psychological Distress. Am J Gastroenterol 101:2546–2551
Milne B, Joachim G, Niedhardt J (1986) A stress management programme for inflammatory bowel disease patients. J Adv Nurs 11:561–567
Mittermaier C, Dejaco C, Waldhoer T et al. (2004) Impact of depressive mood on relapse in patients with inflammatory bowel disease: a prospective 18-month follow-up study. Psychosom Med 66:79–84
Moum B, Vatn MH, Ekbom A et al. (1996) Incidence of Crohn's disease in four counties in southeastern Norway, 1990–1993. A prospective population-based study. The Inflammatory Bowel South-Eastern Norway (IBSEN) Study Group of Gastroenterologists. Scand J Gastroenterol 31:355–361
Moum B, Vatn MH, Ekbom A et al. (1996) Incidence of ulcerative colitis and indeterminate colitis in four counties of southeastern Norway, 1990–93.A prospective population-based study. The Inflammatory Bowel South-Eastern Norway (IBSEN) Study Group of Gastroenterologists. Scand J Gastroenterol 31:362–366
Mussell M, Bocker U, Nagel N, Olbrich R, Singer MV (2003) Reducing psychological distress in patients with inflammatory bowel disease by cognitive-behavioural treatment: exploratory study of effectiveness. Scand J Gastroenterol 38:755–762
North CS, Clouse RE, Spitznagel EL, Alpers DH (1990) The relation of ulcerative colitis to psychiatric factors: a review of findings and methods. Am J Psychiatry 147:974–981
North CS, Alpers DH, Helzer JE, Spitznagel EL, Clouse RE (1991) Do life events or depression exacerbate inflammatory bowel disease? A prospective study. Ann Intern Med 114:381–386
North CS, Alpers DH, North CS, Clouse RE, Spitznagel EL, Alpers DH (1994) A review of studies of psychiatric factors in Crohn's disease: etiologic implications. The relation of ulcerative colitis to psychiatric factors: a review of findings and methods. Ann Clin Psychiatry 6:117–124
Paulley JW (1956) Psychotherapy in ulcerative colitis. Lancet 271(6936):215–218
Persoons P, Vermeire S, Demyttenaere K et al. (2005) The impact of major depressive disorder on the short- and long-term outcome of Crohn's disease treatment with infliximab. Aliment Pharmacol Ther 22:101–110
Porcelli P, Zaka S, Centonze S, Sisto G (1994) Psychological distress and levels of disease activity in inflammatory bowel disease. Ital J Gastroenterol 26:111–115
Porcelli P, Zaka S, Leoci C, Centonze S, Taylor GJ (1995) Alexithymia in inflammatory bowel disease. A case-control study. Psychother Psychosom 64:49–53
Porcelli P, Leoci C, Guerra V, Porcelli P, Zaka S, Centonze S, Sisto G (1996) A prospective study of the relationship between disease activity and psychologic distress in patients with inflammatory bowel disease. Psychological distress and levels of disease activity in inflammatory bowel disease. Scand J Gastroenterol 31:792–796
Porcelli P, Leoci C, Guerra V, Taylor GJ, Bagby RM (1996) A longitudinal study of alexithymia and psychological distress in inflammatory bowel disease. J Psychosom Res 41:569–573
Porcelli P, Taylor GJ, Bagby RM et al. (1999) Alexithymia and functional gastrointestinal disorders. A comparison with inflammatory bowel disease. Psychother Psychosom 68:263–269
Robertson DA, Ray J, Diamond I, Edwards JG (1989) Personality profile and affective state of patients with inflammatory bowel disease. Gut 30:623–626
Roblin X, Oltean P, Heluwaert F, Bonaz B (2006) Panic attack with suicide: an exceptional adverse effect of infliximab. Dig Dis Sci 51:1056
Rutgeerts P, Sandborn WJ, Feagan BG et al. (2005) Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med 353:2462–2476
Schwarz SP, Blanchard EB (1991) Evaluation of a psychological treatment for inflammatory bowel disease. Behav Res Ther 29:167–177
Shaw L, Ehrlich A (1987) Relaxation training as a treatment for chronic pain caused by ulcerative colitis. Pain 29:287–293
Smith GD, Watson R, Roger D, McRorie E, Hurst N, Luman W, Palmer KR (2002) Impact of a nurse-led counselling service on quality of life in patients with inflammatory bowel disease. J Adv Nurs 38:152–160
Tarter RE, Switala J, Carra J, Edwards KL, Van Thiel DH (1987) Inflammatory bowel disease: psychiatric status of patients before and after disease onset. Int J Psychiatry Med 17:173–181
Trzepacz PT, Levenson JL, Tringali RA (1991) Psychopharmacology and neuropsychiatric syndromes in organ transplantation. Gen Hosp Psychiatry 13:233–245
Vidal A, Gomez-Gil E, Sans M et al. (2006) Life events and inflammatory bowel disease relapse: a prospective study of patients enrolled in remission. Psychosocial determinants of relapse in ulcerative colitis: a longitudinal study. Am J Gastroenterol 101:775–781
Vollrath M (2001) Personality and stress. Scand J Psychol 42:335–347
Walker EA, Gelfand MD, Gelfand AN, Creed F, Katon WJ (1996) The relationship of current psychiatric disorder to functional disability and distress in patients with inflammatory bowel disease. Gen Hosp Psychiatry 18:220–229
Waters BM, Jensen L, Fedorak RN (2005) Effects of formal education for patients with inflammatory bowel disease: a randomized controlled trial. Can J Gastroenterol 19:235–244
Weinryb RM, Gustavsson JP, Barber JP (1997) Personality predictors of dimensions of psychosocial adjustment after surgery. Psychosom Med 59:626–631
Weinryb RM, Gustavsson JP, Barber JP (2003) Personality traits predicting long-term adjustment after surgery for ulcerative colitis. J Clin Psychol 59:1015–1029
Zaag-Loonen HJ van der, Grootenhuis MA, Last BF, Derkx HH (2004) Coping strategies and quality of life of adolescents with inflammatory bowel disease. Qual Life Res 13:1011–1019
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boye, B., Jahnsen, J., Lundin, K.E.A. et al. Chronisch entzündliche Darmerkrankungen (Colitis ulcerosa und Morbus Crohn) aus der Perspektive der Konsiliar-/Liaison-Psychosomatik und -Psychiatrie. Psychosom Konsiliarpsychiatr 1, 258–265 (2007). https://doi.org/10.1007/s11800-007-0026-8
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s11800-007-0026-8