Abstract
Purpose
Group medical consultations (GMCs) provide individual medical visits conducted within a group of four to eight peer patients. This study evaluated the feasibility and efficacy of GMCs in the follow-up of breast cancer.
Methods
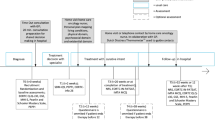
In this randomized controlled trial, 38 patients participated in a single GMC (intervention group), while the control group (n = 31) received individual outpatient visits. Feasibility is measured in terms of acceptability, demand, practicability and costs, integration and implementation, and efficacy. Between-group differences on the efficacy outcomes distress (SCL-90) and empowerment (CEQ), 1 week and 3 months after the visit, were analyzed using ANCOVAs.
Results
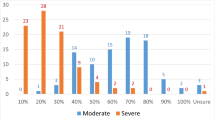
GMCs scored high on most areas of feasibility. Patients in GMCs and individual visits were equally satisfied. Patients and professionals reported more discussed themes in GMCs, despite no between-group differences on information needs prior to the visit. Sixty-nine percent of GMC patients experienced peer support. Costs for GMCs were higher compared to individual visits. However, involving a clinical nurse specialist (CNS) instead of a medical specialist reduced costs to the level of individual CNS care. Efficacy outcomes (distress and empowerment) were equal in both groups.
Conclusion
GMCs in this study were feasible. Further optimization of GMCs in future (cost-)effectiveness trials is possible by increasing the frequency of GMCs, stating criteria for the type of professionals, number of patients involved, and time limits.
Implications for Cancer Survivors
BCS may benefit from GMCs by receiving more information and additional peer support. GMCs cover all aspects of follow-up and may be a good alternative for individual follow-up.


Similar content being viewed by others
References
Bloom JR, Stewart SL, Chang S, Banks PJ. Then and now: quality of life of young breast cancer survivors. Psycho-Oncology. 2004;13(3):147–60.
Allen JD, Savadatti S, Levy AG. The transition from breast cancer ‘patient’ to ‘survivor’. Psycho-Oncology. 2009;18(1):71–8.
Garofalo JP, Choppala S, Hamann HA, Gjerde J. Uncertainty during the transition from cancer patient to survivor. Cancer Nurs. 2009;32(4):E8–14.
Cappiello M, Cunningham RS, Knobf MT, Erdos D. Breast cancer survivors: information and support after treatment. Clin Nurs Res. 2007;16(4):278–93. discussion 94–301.
Bower JE, Ganz PA, Desmond KA, Bernaards C, Rowland JH, Meyerowitz BE, et al. Fatigue in long-term breast carcinoma survivors: a longitudinal investigation. Cancer. 2006;106(4):751–8.
Ganz PA, Desmond KA, Leedham B, Rowland JH, Meyerowitz BE, Belin TR. Quality of life in long-term, disease-free survivors of breast cancer: a follow-up study. J Natl Cancer Inst. 2002;94(1):39–49.
Armes J, Crowe M, Colbourne L, Morgan H, Murrells T, Oakley C, et al. Patients’ supportive care needs beyond the end of cancer treatment: a prospective, longitudinal survey. J Clin Oncol. 2009;27(36):6172–9.
Rutten LJ, Arora NK, Bakos AD, Aziz N, Rowland J. Information needs and sources of information among cancer patients: a systematic review of research (1980–2003). Patient Educ Couns. 2005;57(3):250–61.
Thewes B, Butow P, Girgis A, Pendlebury S. The psychosocial needs of breast cancer survivors: a qualitative study of the shared and unique needs of younger versus older survivors. Psycho-Oncology. 2004;13(3):177–89.
Taylor S, Harley C, Campbell LJ, Bingham L, Podmore EJ, Newsham AC, et al. Discussion of emotional and social impact of cancer during outpatient oncology consultations. Psycho-Oncology. 2011;20(3):242–51.
Comprehensive Cancer Center the Netherlands. Oncoline. In: Breast cancer- aftercare and follow-up guidelines. Oncoline. 2012. http://richtlijnendatabase.nl/en/richtlijn/breast_cancer/aftercare_and_follow-up.html. 2014.
van Hezewijk M, van den Akker ME, van de Velde CJ, Scholten AN, Hille ET. Costs of different follow-up strategies in early breast cancer: a review of the literature. Breast. 2012;21(6):693–700.
Rojas MP, Telaro E, Russo A, Fossati R, Confalonieri C, Liberati A. Follow-up strategies for women treated for early breast cancer. Cochrane Database Syst Rev. 2000;4, CD001768.
Keesing S, McNamara B, Rosenwax L. Cancer survivors’ experiences of using survivorship care plans: a systematic review of qualitative studies. J Cancer Surviv. 2014.
Thompson J, Coleman R, Colwell B, Freeman J, Greenfield D, Holmes K, et al. Preparing breast cancer patients for survivorship (PREP)—a pilot study of a patient-centred supportive group visit intervention. Eur J Oncol Nurs. 2014;18(1):10–6.
Jones JM, Cheng T, Jackman M, Walton T, Haines S, Rodin G, et al. Getting back on track: evaluation of a brief group psychoeducation intervention for women completing primary treatment for breast cancer. Psycho-Oncology. 2013;22(1):117–24.
Goodwin PJ, Leszcz M, Ennis M, Koopmans J, Vincent L, Guther H, et al. The effect of group psychosocial support on survival in metastatic breast cancer. N Engl J Med. 2001;345(24):1719–26.
Helgeson VS, Cohen S, Schulz R, Yasko J. Long-term effects of educational and peer discussion group interventions on adjustment to breast cancer. Health Psychol. 2001;20(5):387–92.
Bjorneklett HG, Lindemalm C, Ojutkangas ML, Berglund A, Letocha H, Strang P, et al. A randomized controlled trial of a support group intervention on the quality of life and fatigue in women after primary treatment for early breast cancer. Support Care Cancer. 2012;20(12):3325–34.
Seesing FM, Gezamenlijk RI, Consult M. Een praktische handleiding. Houten: Bohn Stafleu; 2009.
Foster C, Fenlon D. Recovery and self-management support following primary cancer treatment. Br J Cancer. 2011;105 Suppl 1:S21–8.
Meehan KR, Hill JM, Root L, Kimtis E, Patchett L, Noffsinger EB. Group medical appointments: organization and implementation in the bone marrow transplantation clinic. Support Cancer Ther. 2006;3(2):84–90.
Noffsinger EB. Will drop-in group medical appointments (DIGMAs) work in practice? Permanente J. 1999;3:58–67.
Visser A, Prins JB, Hoogerbrugge N, van Laarhoven HW. Group medical visits in the follow-up of women with a BRCA mutation: design of a randomized controlled trial. BMC Women’s Health. 2011;11:39.
Rhee H, Ciurzynski SM, Yoos HL. Pearls and pitfalls of community-based group interventions for adolescents: lessons learned from an adolescent asthma cAMP study. Issues Compr Pediatr Nurs. 2008;31(3):122–35.
de Vries B, Darling-Fisher C, Thomas AC, Belanger-Shugart EB. Implementation and outcomes of group medical appointments in an outpatient specialty care clinic. J Am Acad Nurse Pract. 2008;20(3):163–9.
Mackay FD. Well woman’s group medical appointment: for screening and preventive care. Can Fam Physician. 2011;57(4):e125–7.
Lorentz PA, Swain JM, Gall MM, Collazo-Clavell ML. Combined group and individual model for postbariatric surgery follow-up care. Surg Obes Relat Dis : Off J Am Soc Bariatric Surg. 2012;8(2):220–4.
Cole RE, Boyer KM, Spanbauer SM, Sprague D, Bingham M. Effectiveness of prediabetes nutrition shared medical appointments: prevention of diabetes. Diabetes Educ. 2013;39(3):344–53.
Edelman D, McDuffie JR, Oddone E, Gierisch JM, Nagi A, Williams JW. Shared medical appointments for chronic medical conditions: a systematic review. Washington (DC): VA Evidence-based Synthesis Program Reports; 2012.
Slyer JT, Ferrara LR. The effectiveness of group visits for patients with heart failure on knowledge, quality of life, self-care, and readmissions: a systematic review. JBI Database Syst Rev Implement Rep. 2013;11(7):58–81.
Egger G, Binns A, Cole MA, Ewald D, Davies L, Meldrum H, et al. Shared medical appointments—an adjunct for chronic disease management in Australia? Aust Fam Physician. 2014;43(3):151–4.
Beck A, Scott J, Williams P, Robertson B, Jackson D, Gade G, et al. A randomized trial of group outpatient visits for chronically ill older HMO members: the Cooperative Health Care Clinic. J Am Geriatr Soc. 1997;45(5):543–9.
Bronson DL, Maxwell RA. Shared medical appointments: increasing patient access without increasing physician hours. Cleve Clin J Med. 2004;71(5):369–70. 72, 74 passim.
Trotter K, Schneider SM, Turner BS. Group appointments in a breast cancer survivorship clinic. J Adv Pract Oncol. 2013;4(6):423–31.
Keyzer-Dekker CM, Van Esch L, Schreurs WH, van Berlo CL, Roukema JA, De Vries J, et al. Health care utilization one year following the diagnosis benign breast disease or breast cancer. Breast. 2012;21(6):746–50.
de Bock GH, Bonnema J, Zwaan RE, van de Velde CJ, Kievit J, Stiggelbout AM. Patient’s needs and preferences in routine follow-up after treatment for breast cancer. Br J Cancer. 2004;90(6):1144–50.
Trotter K, Frazier A, Hendricks CK, Scarsella H. Innovation in survivor care: group visits. Clin J Oncol Nurs. 2011;15(2):E24–33.
Jaber R, Braksmajer A, Trilling JS. Group visits: a qualitative review of current research. J Am Board Fam Med. 2006;19(3):276–90.
Bowen DJ, Kreuter M, Spring B, Cofta-Woerpel L, Linnan L, Weiner D, et al. How we design feasibility studies. Am J Prev Med. 2009;36(5):452–7.
van Campen C, Sixma HJ, Kerssens JJ, Peters L, Rasker JJ. Assessing patients’ priorities and perceptions of the quality of health care: the development of the QUOTE-Rheumatic-Patients instrument. Br J Rheumatol. 1998;37(4):362–8.
de Kok M, Scholte RW, Sixma HJ, van der Weijden T, Spijkers KF, van de Velde CJ, et al. The patient’s perspective of the quality of breast cancer care. The development of an instrument to measure quality of care through focus groups and concept mapping with breast cancer patients. Eur J Cancer. 2007;43(8):1257–64.
Bouwmans C, de Jong K, Timman R, Zijlstra-Vlasveld M, van der Feltz-Cornelis C, Tan Swan S, et al. Feasibility, reliability and validity of a questionnaire on healthcare consumption and productivity loss in patients with a psychiatric disorder (TiC-P). BMC Health Serv Res. 2013;13:217.
Hakkaart-van Roijen L, Tan S, Bouwmans C. Handleiding voor kostenonderzoek, methoden en standaard kostprijzen voor economische evaluaties in de gezondheidszorg [Guideline for cost analyses, methods and standardized cost prizes for economic evaluations in health care]. 2011.
Arrindell WA, Ettema JHM. Symptom Checklist-90; Handleiding bij een multidimensionele psychopathologie-indicator. Lisse: Swets & Zeitlinger B.V.; 2003.
Zimmerman MA. Psychological empowerment: issues and illustrations. American Journal of Community Psychology. 1995;23(5).
van den Berg SW, van Amstel FK, Ottevanger PB, Gielissen MF, Prins JB. The cancer empowerment questionnaire: psychological empowerment in breast cancer survivors. J Psychosoc Oncol. 2013;31(5):565–83.
Custers JA, van den Berg SW, van Laarhoven HW, Bleiker EM, Gielissen MF, Prins JB. The cancer worry scale: detecting fear of recurrence in breast cancer survivors. Cancer Nurs. 2014;37(1):E44–50.
Bottomley A, Aaronson NK. International perspective on health-related quality-of-life research in cancer clinical trials: the European organisation for research and treatment of cancer experience. J Clin Oncol. 2007;25(32):5082–6.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365–76.
Sprangers MA, Groenvold M, Arraras JI, Franklin J, te Velde A, Muller M, et al. The European organization for research and treatment of cancer breast cancer-specific quality-of-life questionnaire module: first results from a three-country field study. J Clin Oncol. 1996;14(10):2756–68.
Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47(6):555–67.
Drummond MF. Methods for the economic evaluation of health care programmes. 3rd ed. Oxford: Oxford University Press; 2005.
Seesing FM, Drost G, Groenewoud J, van der Wilt GJ, van Engelen BG. Shared medical appointments improve QOL in neuromuscular patients: a randomized controlled trial. Neurology. 2014;83(3):240–6.
Mewes JC, Steuten LM, Ijzerman MJ, van Harten WH. Effectiveness of multidimensional cancer survivor rehabilitation and cost-effectiveness of cancer rehabilitation in general: a systematic review. The oncologist. 2012.
Fagerlind H, Kettis A, Bergstrom I, Glimelius B, Ring L. Different perspectives on communication quality and emotional functioning during routine oncology consultations. Patient Educ Couns. 2012;88(1):16–22.
Husson O, Thong MS, Mols F, Oerlemans S, Kaptein AA, van de Poll-Franse LV. Illness perceptions in cancer survivors: what is the role of information provision? Psycho-Oncology. 2013;22(3):490–8.
Boinon D, Sultan S, Charles C, Stulz A, Guillemeau C, Delaloge S, et al. Changes in psychological adjustment over the course of treatment for breast cancer: the predictive role of social sharing and social support. Psycho-Oncology. 2014;23(3):291–8.
Taylor CLC, Kulik J, Badr H, Smith M, Basen-Engquist K, Penedo F, et al. A social comparison theory analysis of group composition and efficacy of cancer support group programs. Soc Sci Med. 2007;65(2):262–73.
Nielsen BK, Mehlsen M, Jensen AB, Zachariae R. Cancer-related self-efficacy following a consultation with an oncologist. Psycho-Oncology. 2013;22(9):2095–101.
Acknowledgments
We thank Renate Besselink, clinical nurse specialist, and Linde Bögemann, social worker, for their contribution in many GMCs. We also thank Marianne Deelen, research coordinator, for her efforts in the preparation and logistics of the GMCs.
Conflict of interest
None declared.
Ethical considerations
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Visser, A., van Laarhoven, H.W.M., Govaert, P.H.M. et al. Group medical consultations in the follow-up of breast cancer: a randomized feasibility study. J Cancer Surviv 9, 450–461 (2015). https://doi.org/10.1007/s11764-014-0421-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-014-0421-z