Abstract
Objectives
Our study aim was to evaluate oncological outcomes after compromised sublobar resection for high-risk clinical-stage IA radiologically solid non-small cell lung cancer (NSCLC), and to investigate potential clinical predictors of improved survival.
Methods
Among 1109 resected clinical-stage IA NSCLC from 2008 to 2013, 115 (10 %) patients who presented radiologically solid, i.e., invasive appearances on thin-section computed tomography (CT) and were poor candidates for lobectomy underwent compromised sublobar resection. Radiologically solid lung cancer was defined as 0.5 ≤ consolidation/tumor ratio based on thin-section CT scan.
Results
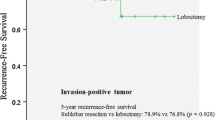
The high-risk cohorts consisted of 65 men and 50 women, with an average age of 71.2 years. The 3-year overall survival (OS) and relapse-free survival were 82.2 and 72.2 % with 34 months of mean follow-up period. A multivariate analysis identified tumor size and carcinoembryonic antigen as significant, consolidation status as marginally significant clinical predictors of survival (p = 0.0141, 0.0426, 0.0623). When the patients were divided based on the number of negative predictors, the 3-year OS of the patients who met neither or one of these negative predictors (n = 64) was 98.4 % despite their anticipated risks, while that of the patients with 2 negative predictors was 71.5 % (n = 38), and the patients who met all of the poor conditions (n = 13) was 37.1 % even in clinical-stage IA disease (p < 0.0001).
Conclusions
Among clinical-stage IA radiologically solid NSCLC patients who are not lobectomy candidates due to the anticipated risk, sublobar resection could provide acceptable oncological outcomes if patients show positive clinical predictors to improve their survival.

Similar content being viewed by others
References
Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395–409.
Travis WD, Brambilla E, Noguchi M, Nicholson AG, Geisinger KR, Yatabe Y, et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol. 2011;6:244–85.
Suzuki K, Kusumoto M, Watanabe S, Tsuchiya R, Asamura H. Radiologic classification of small adenocarcinoma of the lung: radiologic–pathologic correlation and its prognostic impact. Ann Thorac Surg. 2006;81:413–9.
Suzuki K, Asamura H, Kusumoto M, Kondo H, Tsuchiya R. “Early” peripheral lung cancer: prognostic significance of ground glass opacity on thin-section computed tomographic scan. Ann Thorac Surg. 2002;74:1635–9.
Suzuki K, Koike T, Asakawa T, Kusumoto M, Asamura H, Nagai K, et al. A prospective radiological study of thin-section computed tomography to predict pathological noninvasiveness in peripheral clinical IA lung cancer (Japan Clinical Oncology Group 0201). J Thorac Oncol. 2011;6:751–6.
Asamura H, Hishida T, Suzuki K, Koike T, Nakamura K, Kusumoto M, et al. Radiographically determined noninvasive adenocarcinoma of the lung: survival outcomes of Japan Clinical Oncology Group 0201. J Thorac Cardiovasc Surg. 2013;146:24–30.
Hattori A, Suzuki K, Matsunaga T, Miyasaka Y, Takamochi K, Oh S. What is the appropriate operative strategy for radiologically solid tumours in subcentimetre lung cancer patients? Eur J Cardiothorac Surg. 2015;47:244–9.
Hattori A, Suzuki K, Matsunaga T, Fukui M, Kitamura Y, Miyasaka Y, et al. Is limited resection appropriate for radiologically “solid” tumors in small lung cancers? Ann Thorac Surg. 2012;94:212–5.
Hattori A, Suzuki K, Maeyashiki T, Fukui M, Kitamura Y, Matsunaga T, et al. The presence of air bronchogram is a novel predictor of negative nodal involvement in radiologically pure-solid lung cancer. Eur J Cardiothorac Surg. 2014;45:699–702.
Nakamura K, Saji H, Nakajima R, Okada M, Asamura H, Shibata T, et al. A phase III randomized trial of lobectomy versus limited resection for small-sized peripheral non-small cell lung cancer (JCOG0802/WJOG4607L). Jpn J Clin Oncol. 2011;40:271–4.
ClinicalTrials.gov. Comparison of different types of surgery in treating patients with stage IA non-small cell lung cancer. Bethesda: National Institutes of Health. http://clinicaltrials.gov/ct/show/NCT00499330. Accessed 9 Jan 2012.
Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg. 1995;60:615–22 (discussion 622–3).
Kent M, Landreneau R, Mandrekar S, Hillman S, Nichols F, Jones D, et al. Segmentectomy versus wedge resection for non-small cell lung cancer in high-risk operable patients. Ann Thorac Surg. 2013;96:1747–54 (discussion 1754–5).
Kilic A, Schuchert MJ, Pettiford BL, Pennathur A, Landreneau JR, Landreneau JP, et al. Anatomic segmentectomy for stage I non-small cell lung cancer in the elderly. Ann Thorac Surg. 2009;87:1662–6 (discussion 1667–8).
Timmerman R, Paulus R, Galvin J, Michalski J, Straube W, Bradley J, et al. Stereotactic body radiation therapy for inoperable early stage lung cancer. JAMA. 2010;303:1070–6.
Fernando HC, Landreneau RJ, Mandrekar SJ, Hillman SL, Nichols FC, Meyers B, et al. Thirty- and ninety-day outcomes after sublobar resection with and without brachytherapy for non-small cell lung cancer: results from a multicenter phase III study. J Thorac Cardiovasc Surg. 2011;142:1143–51.
Nagata YHM, Shibata T, Onishi H, Kokubo M, Karasawa K, Shioyama Y, et al. Stereotactic body radiation therapy for T1N0M0 non-small cell lung cancer: first report for inoperable population of a phase II trial by Japan Clinical Oncology Group (JCOG 0403). Int J Radiat Oncol Biol Phys. 2012;84:S46.
Schuchert MJ, Kilic A, Pennathur A, Nason KS, Wilson DO, Luketich JD, et al. Oncologic outcomes after surgical resection of subcentimeter non-small cell lung cancer. Ann Thorac Surg. 2011;91:1681–7 (discussion 1687–8).
Onishi H, Araki T, Shirato H, Nagata Y, Hiraoka M, Gomi K, et al. Stereotactic hypofractionated high-dose irradiation for stage I nonsmall cell lung carcinoma: clinical outcomes in 245 subjects in a Japanese multiinstitutional study. Cancer. 2004;101:1623–31.
Robinson CG, DeWees TA, El Naqa IM, Creach KM, Olsen JR, Crabtree TD, et al. Patterns of failure after stereotactic body radiation therapy or lobar resection for clinical stage I non-small-cell lung cancer. J Thorac Oncol. 2013;8:192–201.
Lau KK, Martin-Ucar AE, Nakas A, Waller DA. Lung cancer surgery in the breathless patient–the benefits of avoiding the gold standard. Eur J Cardiothorac Surg. 2010;38:6–13.
Linden PA, Bueno R, Colson YL, Jaklitsch MT, Lukanich J, Mentzer S, et al. Lung resection in patients with preoperative FEV1 < 35% predicted. Chest. 2005;127:1984–90.
Acknowledgments
This work was supported in part by a Grant-in-Aid for Cancer Research from the Ministry of Health, Labour and Welfare, Japan, the Smoking Research Foundation, and the National Cancer Center Research and Development Fund (26-A-4).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Aritoshi Hattori and his co-authors have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Hattori, A., Takamochi, K., Matsunaga, T. et al. Oncological outcomes of sublobar resection for clinical-stage IA high-risk non-small cell lung cancer patients with a radiologically solid appearance on computed tomography. Gen Thorac Cardiovasc Surg 64, 18–24 (2016). https://doi.org/10.1007/s11748-015-0598-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-015-0598-8