Abstract
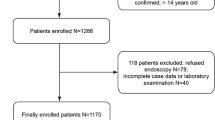
Not all patients with upper gastrointestinal bleeding (UGIB) require emergency endoscopy. Lactate clearance has been suggested as a parameter for predicting patient outcomes in various critical care settings. This study investigates whether lactate clearance can predict active bleeding in critically ill patients with UGIB. This single-center, retrospective, observational study included critically ill patients with UGIB who met all of the following criteria: admission to the emergency department (ED) from April 2011 to August 2014; had blood samples for lactate evaluation at least twice during the ED stay; and had emergency endoscopy within 6 h of ED presentation. The main outcome was active bleeding detected with emergency endoscopy. Classification and regression tree (CART) analyses were performed using variables associated with active bleeding to derive a prediction rule for active bleeding in critically ill UGIB patients. A total of 154 patients with UGIB were analyzed, and 31.2 % (48/154) had active bleeding. In the univariate analysis, lactate clearance was significantly lower in patients with active bleeding than in those without active bleeding (13 vs. 29 %, P < 0.001). Using the CART analysis, a prediction rule for active bleeding is derived, and includes three variables: lactate clearance; platelet count; and systolic blood pressure at ED presentation. The rule has 97.9 % (95 % CI 90.2–99.6 %) sensitivity with 32.1 % (28.6–32.9 %) specificity. Lactate clearance may be associated with active bleeding in critically ill patients with UGIB, and may be clinically useful as a component of a prediction rule for active bleeding.


Similar content being viewed by others
References
Barkun AN, Bardou M, Kuipers EJ et al (2010) International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med 152:101–113. doi:10.7326/0003-4819-152-2-201001190-00009
Laursen SB, Hansen JM, Schaffalitzky de Muckadell OB (2012) The Glasgow Blatchford score is the most accurate assessment of patients with upper gastrointestinal hemorrhage. Clin Gastroenterol Hepatol 10(1130–1135):e1. doi:10.1016/j.cgh.2012.06.022
Stanley AJ, Dalton HR, Blatchford O et al (2011) Multicentre comparison of the Glasgow Blatchford and Rockall Scores in the prediction of clinical end-points after upper gastrointestinal haemorrhage. Aliment Pharmacol Ther 34:470–475. doi:10.1111/j.1365-2036.2011.04747.x
Blatchford O, Murray WR, Blatchford M (2000) A risk score to predict need for treatment for upper-gastrointestinal haemorrhage. Lancet 356:1318–1321. doi:10.1016/S0140-6736(00)02816-6
Stanley AJ, Ashley D, Dalton HR et al (2009) Outpatient management of patients with low-risk upper-gastrointestinal haemorrhage: multicentre validation and prospective evaluation. Lancet 373:42–47. doi:10.1016/S0140-6736(08)61769-9
Attar A, Sebbagh V, Vicaut E et al (2012) Urgent endoscopy in severe non-variceal upper gastrointestinal hemorrhage: does the Glasgow-Blatchford score help endoscopists? Scand J Gastroenterol 47:1086–1093. doi:10.3109/00365521.2012.703237
Zhang Z, Xu X (2014) Lactate clearance is a useful biomarker for the prediction of all-cause mortality in critically Ill patients. Crit Care Med 42:2118–2125. doi:10.1097/CCM.0000000000000405
El-Kersh K, Chaddha U, Sinha RS et al (2015) Predictive role of admission lactate level in critically Ill patients with acute upper gastrointestinal bleeding. J Emerg Med. doi:10.1016/j.jemermed.2015.04.008
Sacks HS, Chalmers TC, Blum AL et al (1990) Endoscopic hemostasis. An effective therapy for bleeding peptic ulcers. JAMA 264:494–499
Jairath V, Kahan BC, Logan RFA et al (2012) Outcomes following acute nonvariceal upper gastrointestinal bleeding in relation to time to endoscopy: results from a nationwide study. Endoscopy 44:723–730. doi:10.1055/s-0032-1309736
Lin HJ, Wang K, Perng CL et al (1996) Early or delayed endoscopy for patients with peptic ulcer bleeding. A prospective randomized study. J Clin Gastroenterol 22:267–271
Bjorkman DJ, Zaman A, Fennerty MB et al (2004) Urgent vs. elective endoscopy for acute non-variceal upper-GI bleeding: an effectiveness study. Gastrointest Endosc 60:1–8
Forrest J, Finlayson ND, Shearman DJ (1974) Endoscopy in gastrointestinal bleeding. Lancet 304:394–397. doi:10.1016/S0140-6736(74)91770-X
Almenoff PL, Leavy J, Weil MH et al (1989) Prolongation of the half-life of lactate after maximal exercise in patients with hepatic dysfunction. Crit Care Med 17:870–873
Grobman WA, Stamilio DM (2006) Methods of clinical prediction. Am J Obstet Gynecol 194:888–894. doi:10.1016/j.ajog.2005.09.002
Stiell I, Wells G (1999) Methodologic standards for the development of clinical decision rules in emergency medicine. Ann Emerg Med 33:437–447. doi:10.1016/S0196-0644(99)70309-4
Kreisberg RA (1980) Lactate homeostasis and lactic acidosis. Ann Intern Med 92:227–237
Jones AE, Shapiro NI, Trzeciak S et al (2010) Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA 303:739–746. doi:10.1001/jama.2010.158
Adamopoulos AB, Baibas NM, Efstathiou SP et al (2003) Differentiation between patients with acute upper gastrointestinal bleeding who need early urgent upper gastrointestinal endoscopy and those who do not. A prospective study. Eur J Gastroenterol Hepatol 15:381–387. doi:10.1097/01.meg.0000050005.68425.22
Iwasaki H, Shimura T, Yamada T et al (2013) Novel nasogastric tube-related criteria for urgent endoscopy in nonvariceal upper gastrointestinal bleeding. Dig Dis Sci 58:2564–2571. doi:10.1007/s10620-013-2706-x
Bloom BM, Grundlingh J, Bestwick JP, Harris T (2014) The role of venous blood gas in the emergency department: a systematic review and meta-analysis. Eur J Emerg Med 21:81–88. doi:10.1097/MEJ.0b013e32836437cf
Acknowledgments
The authors wish to thank all the Emergency Department residents and attending staff at Center Hospital of the National Center for Global Health and Medicine for their kind help in this study. The authors acknowledge the contribution of the medical staff in the Department of Gastroenterology at Center Hospital of the National Center for Global Health and Medicine in the implementation of emergency endoscopy for each patient in the present study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare.
Statement of human and animal rights
The present study was conducted in accordance with the amended Declaration of Helsinki. The Ethics Committee of Center Hospital of the National Center for Global Health and Medicine approved this study.
Informed consent
The requirement for written informed consent from patients was waived because the study design formed part of the current standard of care in the ED, and patient data were anonymous.
Rights and permissions
About this article
Cite this article
Wada, T., Hagiwara, A., Uemura, T. et al. Early lactate clearance for predicting active bleeding in critically ill patients with acute upper gastrointestinal bleeding: a retrospective study. Intern Emerg Med 11, 737–743 (2016). https://doi.org/10.1007/s11739-016-1392-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-016-1392-z