Abstract
Polyetheretherketone (PEEK) is regarded as one of the most potential candidates for replacing current implant applications. To obtain good bone-implant interfaces, many modification methods have been developed to enable PEEK and PEEK-based composites from bio-inert to bioactive. Among them, physical methods have aroused significant attention and been widely used to modify PEEK for orthopedic implants. This review summarizes current physical modification techniques of PEEK for orthopedic applications, which include composite strategies, surface coating methods and irradiation treatments. The positive consequences of those modification methods will encourage continuing investigations and stimulate the wide range of applications of PEEK-based implants in orthopedics.
Similar content being viewed by others
References
Stolarski T A. Tribology of polyetheretherketone. Wear, 1992, 158(1–2): 71–78
Bishop S M. The mechanical performance and impact behaviour of carbon-fibre reinforced PEEK. Composite Structures, 1985, 3(3–4): 295–318
Fujihara K, Huang Z M, Ramakrishna S, et al. Feasibility of knitted carbon/PEEK composites for orthopedic bone plates. Biomaterials, 2004, 25(17): 3877–3885
Searle O B, Pfeiffer R H. Victrex® poly (ethersulfone) (PES) and Victrex® poly (etheretherketone) (PEEK). Polymer Engineering and Science, 1985, 25(8): 474–476
Jamison R D, Maharaj G R. Intraoperative impact: characterization and laboratory simulation on composite hip prostheses. In: Jamison R D, Gilbertson L N, Composite Materials for Implant Applications in the Human Body: Characterization and Testing. ASTM International STP 1178, 1993, 98–108
Kurtz S M, Devine J N. PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials, 2007, 28(32): 4845–4869
Saito N, Aoki K, Usui Y, et al. Application of carbon fibers to biomaterials: a new era of nano-level control of carbon fibers after 30-years of development. Chemical Society Reviews, 2011, 40(7): 3824–3834
Williams D F, McNamara A, Turner R M. Potential of polyetheretherketone (PEEK) and carbon-fibre-reinforced PEEK in medical applications. Journal of Materials Science Letters, 1987, 6(2): 188–190
Wenz L M, Merritt K, Brown S A, et al. In vitro biocompatibility of polyetheretherketone and polysulfone composites. Journal of Biomedical Materials Research, 1990, 24(2): 207–215
Hunter A, Archer C W, Walker P S, et al. Attachment and proliferation of osteoblasts and fibroblasts on biomaterials for orthopaedic use. Biomaterials, 1995, 16(4): 287–295
Pioch T, Stotz S, Staehle H J, et al. Applications of confocal laser scanning microscopy to dental bonding. Advances in Dental Research, 1997, 11(4): 453–461
Scotchford C A, Garle C, Batchelor J, et al. Use of a novel carbon fibre composite material for the femoral stem component of a THR system: in vitro biological assessment. Biomaterials, 2003, 24(26): 4871–4879
Lin TW, Corvelli A A, Frondoza C G, et al. Glass peek composite promotes proliferation and osteocalcin production of human osteoblastic cells. Journal of Biomedical Materials Research, 1997, 36(2): 137–144
Katzer A, Marquardt H, Westendorf J, et al. Polyetheretherketone cytotoxicity and mutagenicity in vitro. Biomaterials, 2002, 23(8): 1749–1759
Jockisch K A, Brown S A, Bauer TW, et al. Biological response to chopped-carbon-fiber-reinforced peek. Journal of Biomedical Materials Research, 1992, 26(2): 133–146
Schwitalla A, Müller W D. PEEK dental implants: a review of the literature. The Journal of Oral Implantology, 2013, 39(6): 743–749
Rattier B D, Hoffman A S, Schoen F J, et al. Biomaterials science: an introduction to materials in medicine. Journal of Clinical Engineering, 1997, 22(1): 26
Brennan W J, Feast W J, Munro H S, et al. Investigation of the ageing of plasma oxidized PEEK. Polymer, 1991, 32(8): 1527–1530
Briem D, Strametz S, Schröoder K, et al. Response of primary fibroblasts and osteoblasts to plasma treated polyetheretherketone (PEEK) surfaces. Journal of Materials Science: Materials in Medicine, 2005, 16(7): 671–677
Charest J L, Eliason M T, García A J, et al. Combined microscale mechanical topography and chemical patterns on polymer cell culture substrates. Biomaterials, 2006, 27(11): 2487–2494
Anselme K, Linez P, Bigerelle M, et al. The relative influence of the topography and chemistry of TiAl6V4 surfaces on osteoblastic cell behaviour. Biomaterials, 2000, 21(15): 1567–1577
Roeder R K, Converse G L, Kane R J, et al. Hydroxyapatitereinforced polymer biocomposites for synthetic bone substitutes. JOM, 2008, 60(3): 38–45
Wang Q Q, Wu J J, Unsworth A, et al. Biotribological study of large diameter ceramic-on-CFR-PEEK hip joint including fluid uptake, wear and frictional heating. Journal of Materials Science: Materials in Medicine, 2012, 23(6): 1533–1542
Scholes S C, Unsworth A. The wear performance of PEEKOPTIMA based self-mating couples. Wear, 2010, 268(3–4): 380–387
Doorn P F, Campbell P A, Amstutz H C. Metal versus polyethylene wear particles in total hip replacements. A review. Clinical Orthopaedics and Related Research, 1996, 329(Suppl): S206–S216
Catelas I, Huk O L, Petit A, et al. Flow cytometric analysis of macrophage response to ceramic and polyethylene particles: effects of size, concentration, and composition. Journal of Biomedical Materials Research, 1998, 41(4): 600–607
Ingham E, Fisher J. Biological reactions to wear debris in total joint replacement. Proceedings of the Institution of Mechanical Engineers Part H: Journal of Engineering in Medicine, 2000, 214(1): 21–37
Ingram J H, Stone M, Fisher J, et al. The influence of molecular weight, crosslinking and counterface roughness on TNF-α production by macrophages in response to ultra high molecular weight polyethylene particles. Biomaterials, 2004, 25(17): 3511–3522
Xiong D, Xiong L, Liu L. Preparation and tribological properties of polyetheretherketone composites. Journal of Biomedical Materials Research Part B: Applied Biomaterials, 2010, 93B(2): 492–496
Rousseau M A, Lazennec J Y, Saillant G. Circumferential arthrodesis using PEEK cages at the lumbar spine. Journal of Spinal Disorders & Techniques, 2007, 20(4): 278–281
Pape D, Adam F, Fritsch E, et al. Primary lumbosacral stability after open posterior and endoscopic anterior fusion with interbody implants: a roentgen stereophotogrammetric analysis. Spine, 2000, 25(19): 2514–2518
McMillin C R. Evaluation of PEKEKK composites for spine implants. In: 38th International SAMPE Symposium, Anaheim, CA, USA. 1993, 591–598
Dickinson A S, Taylor A C, Browne M. The influence of acetabular cup material on pelvis cortex surface strains, measured using digital image correlation. Journal of Biomechanics, 2012, 45(4): 719–723
Kim I Y, Sugino A, Kikuta K, et al. Bioactive composites consisting of PEEK and calcium silicate powders. Journal of Biomaterials Applications, 2009, 24(2): 105–118
Scotchford C A, Garle M J, Batchelor J, et al. Use of a novel carbon fibre composite material for the femoral stem component of a THR system: in vitro biological assessment. Biomaterials, 2003, 24(26): 4871–4879
Sagomonyants K B, Jarman-Smith M L, Devine J N, et al. The in vitro response of human osteoblasts to polyetheretherketone (PEEK) substrates compared to commercially pure titanium. Biomaterials, 2008, 29(11): 1563–1572
Bonfield W, Grynpas M D, Tully A E, et al. Hydroxyapatite reinforced polyethylene — a mechanically compatible implant material for bone replacement. Biomaterials, 1981, 2(3): 185–186
Abu Bakar M S, Cheng M H W, Tang S M, et al. Tensile properties, tension-tension fatigue and biological response of polyetheretherketone-hydroxyapatite composites for load-bearing orthopedic implants. Biomaterials, 2003, 24(13): 2245–2250
Yu S, Hariram K P, Kumar R, et al. In vitro apatite formation and its growth kinetics on hydroxyapatite/polyetheretherketone biocomposites. Biomaterials, 2005, 26(15): 2343–2352
Wang L, Weng L, Song S, et al. Mechanical properties and microstructure of polyetheretherketone-hydroxyapatite nano composite materials. Materials Letters, 2010, 64(20): 2201–2204
Ma R, Weng L, Bao X, et al. Characterization of in situ synthesized hydroxyapatite/polyetheretherketone composite materials. Materials Letters, 2012, 71: 117–119
Ma R, Weng L, Bao X, et al. In vivo biocompatibility and bioactivity of in situ synthesized hydroxyapatite/polyetheretherketone composite materials. Journal of Applied Polymer Science, 2013, 127(4): 2581–2587
Ma R, Fang L, Luo Z, et al. Mechanical performance and in vivo bioactivity of functionally graded PEEK-HA biocomposite materials. Journal of Sol-Gel Science and Technology, 2014, 1: 1–7
Wang M, Joseph R, Bonfield W. Hydroxyapatite-polyethylene composites for bone substitution: effects of ceramic particle size and morphology. Biomaterials, 1998, 19(24): 2357–2366
Santos C, Luklinska Z B, Clarke R L, et al. Hydroxyapatite as a filler for dental composite materials: mechanical properties and in vitro bioactivity of composites. Journal of Materials Science: Materials in Medicine, 2001, 12(7): 565–573
Wong K L, Wong C T, Liu W C, et al. Mechanical properties and in vitro response of strontium-containing hydroxyapatite/polyetheretherketone composites. Biomaterials, 2009, 30(23–24): 3810–3817
Li Y W, Leong J C Y, Lu W W, et al. A novel injectable bioactive bone cement for spinal surgery: a developmental and preclinical study. Journal of Biomedical Materials Research, 2000, 52(1): 164–170
Shorr E, Carter A C. The usefulness of strontium as an adjuvant to calcium in the remineralization of the skeleton in man. Bulletin of the Hospital for Joint Diseases, 1952, 13(1): 59–66
Cox S C, Jamshidi P, Grover L M, et al. Preparation and characterisation of nanophase Sr, Mg, and Zn substituted hydroxyapatite by aqueous precipitation. Materials Science and Engineering C, 2014, 35: 106–114
Okayama S, Akao M, Nakamura S, et al. The mechanical properties and solubility of strontium-substituted hydroxyapatite. Bio-Medical Materials and Engineering, 1991, 1(1): 11–17
Boanini E, Torricelli P, Fini M, et al. Osteopenic bone cell response to strontium-substituted hydroxyapatite. Journal of Materials Science: Materials in Medicine, 2011, 22(9): 2079–2088
Qi Z, Zhang Q, Dai H, et al. Effects of β-TCP ceramics on intracellular Ca2+ concentration, mineralization of osteoblast and protein structure. Journal of Wuhan University of Technology (Materials Science Edition), 2011, 26(6): 1064–1067
Petrovic L, Pohle D, Münstedt H, et al. Effect of β-TCP filled polyetheretherketone on osteoblast cell proliferation in vitro. Journal of Biomedical Science, 2006, 13(1): 41–46
von Wilmowsky C, Vairaktaris E, Pohle D, et al. Effects of bioactive glass and β-TCP containing three-dimensional laser sintered polyetheretherketone composites on osteoblasts in vitro. Journal of Biomedical Materials Research Part A, 2008, 87A(4): 896–902
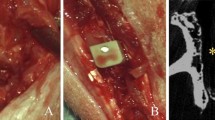
VonWilmonsky C, Lutz R, Meisel U, et al. In vivo evaluation of β-TCP containing 3D laser sintered poly (ether ether ketone) composites in pigs. Journal of Bioactive and Compatible Polymers, 2009, 24(2): 169–184
Suska F, Omar O, Emanuelsson L, et al. Enhancement of CRFPEEK osseointegration by plasma-sprayed hydroxyapatite: A rabbit model. Journal of Biomaterials Applications, 2014, 29(2): 234–242
Lee J H, Jang H L, Lee KM, et al. In vitro and in vivo evaluation of the bioactivity of hydroxyapatite-coated polyetheretherketone biocomposites created by cold spray technology. Acta Biomaterialia, 2013, 9(4): 6177–6187
Gardon M, Latorre A, Torrell M, et al. Cold gas spray titanium coatings onto a biocompatible polymer. Materials Letters, 2013, 106: 97–99
Fauchais P, Vardelle A, Dussoubs B. Quo vadis thermal spraying? Journal of Thermal Spray Technology, 2001, 10(1): 44–66
Fauchais P. Understanding plasma spraying. Journal of Physics D: Applied Physics, 2004, 37(9): R86–R108
Furlong R J, Osborn J F. Fixation of hip prostheses by hydroxyapatite ceramic coatings. The Journal of Bone and Joint Surgery (British Volume), 1991, 73(5): 741–745
Montanaro L, Arciola C R, Campoccia D, et al. In vitro effects on MG63 osteoblast-like cells following contact with two roughnessdiffering fluorohydroxyapatite-coated titanium alloys. Biomaterials, 2002, 23(17): 3651–3659
Kurtz S M. PEEK Biomaterials Handbook. Oxford, UK: William Andrew, 2011, 145–161
Tsui Y C, Doyle C, Clyne T W. Plasma sprayed hydroxyapatite coatings on titanium substrates. Part 1: Mechanical properties and residual stress levels. Biomaterials, 1998, 19(22): 2015–2029
Marrocco T, McCartney D G, Shipway P H, et al. Production of titanium deposits by cold-gas dynamic spray: Numerical modeling and experimental characterization. Journal of Thermal Spray Technology, 2006, 15(2): 263–272
Lupoi R, O’Neill W. Deposition of metallic coatings on polymer surfaces using cold spray. Surface and Coatings Technology, 2010, 205(7): 2167–2173
Hahn B D, Park D S, Choi J J, et al. Osteoconductive hydroxyapatite coated PEEK for spinal fusion surgery. Applied Surface Science, 2013, 283: 6–11
Yao C, Storey D, Webster T J. Nanostructured metal coatings on polymers increase osteoblast attachment. International Journal of Nanomedicine, 2007, 2(3): 487–492
Han CM, Lee E J, Kim H E, et al. The electron beam deposition of titanium on polyetheretherketone (PEEK) and the resulting enhanced biological properties. Biomaterials, 2010, 31(13): 3465–3470
Barkarmo S, Wennerberg A, Hoffman M, et al. Nano-hydroxyapatite-coated PEEK implants: a pilot study in rabbit bone. Journal of Biomedical Materials Research Part A, 2013, 101A(2): 465–471
Jung H D, Sun Park H, Kang M H, et al. Polyetheretherketone/magnesium composite selectively coated with hydroxyapatite for enhanced in vitro bio-corrosion resistance and biocompatibility. Materials Letters, 2014, 116: 20–22
Ha S W, Hauert R, Ernst K H, et al. Surface analysis of chemically-etched and plasma-treated polyetheretherketone (PEEK) for biomedical applications. Surface and Coatings Technology, 1997, 96(2–3): 293–299
Rochford E T J, Poulsson A H C, Salavarrieta Varela J, et al. Bacterial adhesion to orthopaedic implant materials and a novel oxygen plasma modified PEEK surface. Colloids and Surfaces B: Biointerfaces, 2014, 113: 213–222
Garbassi F, Morra M, Occhiello E. Polymer Surfaces: from Physics to Technology. Chichester, UK: John Wiley and Sons, 1994, 221–454
Mathieson I, Bradley R H. Effects of ultraviolet/ozone on the surface chemistry of polymer films. Advanced Engineering Materials, 1994, 99(100): 185–191
Riveiro A, Soto R, Comesana R, et al. Laser surface modification of PEEK. Applied Surface Science, 2012, 258(23): 9437–9442
Akkan C K, Hammadeh M, Brück S, et al. Plasma and short pulse laser treatment of medical grade PEEK surfaces for controlled wetting. Materials Letters, 2013, 109: 261–264
Mangipudi V, Tirrell M, Pocius A V. Direct measurement of the surface energy of corona-treated polyethylene using the surface forces apparatus. Langmuir, 1995, 11(1): 19–23
Strobel M, Walzak M J, Hill J M, et al. A comparison of gas-phase methods of modifying polymer surfaces. Journal of Adhesion Science and Technology, 1995, 9(3): 365–383
Sasuga T, Hagiwara M. Mechanical relaxation of crystalline poly (aryl-ether-ether-ketone) (PEEK) and influence of electron beam irradiation. Polymer, 1986, 27(6): 821–826
Iwanaga S, Akiyama Y, Kikuchi A, et al. Fabrication of a cell array on ultrathin hydrophilic polymer gels utilising electron beam irradiation and UV excimer laser ablation. Biomaterials, 2005, 26(26): 5395–5404
Kim K H, Cho J S, Choi D J, et al. Hydrophilic group formation and cell culturing on polystyrene Petri-dish modified by ionassisted reaction. Nuclear Instruments & Methods in Physics Research Section B: Beam Interactions with Materials and Atoms, 2001, 175–177: 542–547
Khoury J, Kirkpatrick S R, Maxwell M, et al. Neutral atom beam technique enhances bioactivity of PEEK. Nuclear Instruments & Methods in Physics Research Section B: Beam Interactions with Materials and Atoms, 2013, 307: 630–634
Matrab T, Chehimi M M, Boudou J P, et al. Surface functionalization of ultrananocrystalline diamond using atom transfer radical polymerization (ATRP) initiated by electro-grafted aryldiazonium salts. Diamond and Related Materials, 2006, 15(4–8): 639–644
Kyomoto M, Moro T, Takatori Y, et al. Self-initiated surface grafting with poly(2-methacryloyloxyethyl phosphorylcholine) on poly(ether-ether-ketone). Biomaterials, 2010, 31(6): 1017–1024
Kyomoto M, Ishihara K. Self-initiated surface graft polymerization of 2-methacryloyloxyethyl phosphorylcholine on poly(ether ether ketone) by photoirradiation. ACS Applied Materials & Interfaces, 2009, 1(3): 537–542
Lego B, Skene W G, Giasson S. Unprecedented covalently attached ATRP initiator onto OH-functionalized mica surfaces. Langmuir, 2008, 24(2): 379–382
Jin Z, Feng W, Zhu S, et al. Protein-resistant polyurethane by sequential grafting of poly(2-hydroxyethyl methacrylate) and poly (oligo(ethylene glycol) methacrylate) via surface-initiated ATRP. Journal of Biomedical Materials Research Part A, 2010, 95A(4): 1223–1232
Fu K Y, Cheung T L, Mei Y F, et al. Surface modification of polymeric materials by plasma immersion ion implantation. Nuclear Instruments & Methods in Physics Research Section B: Beam Interactions with Materials and Atoms, 2005, 237(1–2): 417–421
Lu T, Qiao Y Q, Liu X Y. Surface modification of biomaterials using plasma immersion ion implantation and deposition. Interface Focus, 2012, 2(3): 325–336
Hegemann D, Brunner H, Oehr C. Plasma treatment of polymers for surface and adhesion improvement. Nuclear Instruments & Methods in Physics Research Section B: Beam Interactions with Materials and Atoms, 2003, 208: 281–286
Liu X M, Wu S L, Chu P K, et al. Effects of water plasma immersion ion implantation on surface electrochemical behavior of NiTi shape memory alloys in simulated body fluids. Applied Surface Science, 2007, 253(6): 3154–3159
Chan C M, Ko T M, Hiraoka H. Polymer surface modification by plasmas and photons. Surface Science Reports, 1996, 24(1–2): 1–54
Ahad I U, Bartnik A, Fiedorowicz H, et al. Surface modification of polymers for biocompatibility via exposure to extreme ultraviolet radiation. Journal of Biomedical Materials Research Part A, 2013 doi: 10.1002/jbm.a.34958
Poulsson A H C, Mitchell S A, Davidson MR, et al. Attachment of human primary osteoblast cells to modified polyethylene surfaces. Langmuir, 2009, 25(6): 3718–3727
Davidson M R, Mitchell S A, Bradley R H. Surface studies of low molecular weight photolysis products from UV-ozone oxidized polystyrene. Surface Science, 2005, 581(2–3): 169–177
Laurens P, Ould Bouali M, Meducin F, et al. Characterization of modifications of polymer surfaces after excimer laser treatments below the ablation threshold. Applied Surface Science, 2000, 154–155: 211–216
Laurens P, Sadras B, Decobert F, et al. Enhancement of the adhesive bonding properties of PEEK by excimer laser treatment. International Journal of Adhesion and Adhesives, 1998, 18(1): 19–27
Kirkpatrick A, Kirkpatrick S, Walsh M, et al. Investigation of accelerated neutral atom beams created from gas cluster ion beams. Nuclear Instruments & Methods in Physics Research Section B: Beam Interactions with Materials and Atoms, 2013, 307: 281–289
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Du, YW., Zhang, LN., Hou, ZT. et al. Physical modification of polyetheretherketone for orthopedic implants. Front. Mater. Sci. 8, 313–324 (2014). https://doi.org/10.1007/s11706-014-0266-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11706-014-0266-4