Abstract
Background
Few prospective studies have compared changes of nutrient intake while assessing effectiveness of thiamin, vitamin B12, and folate supplementation to prevent B vitamin deficiencies immediately following Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG). Therefore, we determined the response to 3 months supplementation on maintaining blood B vitamin concentrations.
Methods
Women undergoing RYGB (n = 11) and SG (n = 11) consumed bariatric vitamin supplements (12 mg thiamin, 350 μg vitamin B12, 800 μg folic acid) daily for 3 months. Height, weight, body mass index, and blood vitamin concentrations were measured preoperatively and at 3 months. Wilcoxon signed-rank analyses compared body weight parameters, laboratory indices, and nutrient intake at baseline and 3 months.
Results
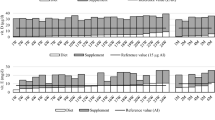
Supplementation for 3 months maintained blood thiamin, increased serum folate from 13.1 ± 5.4 to 16.3 ± 6.0 nmol/L (P = 0.049), and increased serum vitamin B12 concentrations from 498 ± 150 to 736 ± 340 pg/mL (P = 0.005). Dietary intake of thiamin and folate decreased in the combined surgical groups, while dietary intake of B12 was maintained. Bariatric B vitamin supplements provided multiple intakes of the Recommended Dietary Allowances (1090 % thiamin, 14,583 % vitamin B12, 200 % folate).
Conclusions
Although energy intake decreased 64 %, B vitamin supplementation for 3 months resulted in a 48 % increase of serum vitamin B12, a modest increase of serum folate, and no reduction of blood thiamin concentrations. Long-term effects of the rapid rise of serum B12 levels attributed to the high content of supplements warrant further investigation.

Similar content being viewed by others
References
Bal BS, Finelli FC, Shope TR, et al. Nutritional deficiencies after bariatric surgery. Nat Rev Endocrinol. 2012;8:544–56.
Alexandrou A, Armeni E, Kouskouni E, et al. Cross-sectional long-term micronutrient deficiencies after sleeve gastrectomy versus Roux-en-Y gastric bypass: a pilot study. Surg Obes Relat Dis. 2014;10:262–8.
Moize V, Andreu A, Flores L, et al. Long-term dietary intake and nutritional deficiencies following sleeve gastrectomy or Roux-en-Y gastric bypass in a Mediterranean population. J Acad Nutr Diet. 2013;113(3):400–10.
Saab R, El Khoury M, Farhat S. Wernicke’s encephalopathy three weeks after sleeve gastrectomy. Surg Obes Relat Dis. 2013. doi:10.1016/j.soard.2013.11.016.
Moore CE, Sherman V. Vitamin D supplementation efficacy: sleeve gastrectomy versus gastric bypass surgery. Obes Surg 2014; 21 April.
Green R. Indicators for assessing folate and vitamin B12 status and for monitoring the efficacy of intervention strategies. Am J Clin Nutr. 2011;94:666S–72S.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patients—2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity. 2013;21:S1–S27.
Lakhani SV, Shah HN, Alexander K, et al. Small intestinal bacterial overgrowth and thiamine deficiency after Roux-en-Y gastric bypass surgery in obese patients. Nutr Res. 2008;28:293–8.
Damms-Machado A, Friedrich A, Kramer KM, et al. Pre- and postoperative nutritional deficiencies in obese patients undergoing laparoscopic sleeve gastrectomy. Obes Surg. 2012;22:881–9.
Ledoux S, Coupaye M, Bogard C, et al. Determinants of hyperhomocysteinemia after gastric bypass surgery in obese subjects. Obes Surg. 2011;21:78–86.
Institute of Medicine. Dietary Reference Intakes for thiamin, riboflavin, niacin, vitamin B6, vitamin B12, pantothenic acid, biotin and choline. Washington, D.C.: National Academy Press; 1998.
Benaa KH, Njolstad I, Ueland PM, et al. Homocysteine lowering and cardiovascular events after acute myocardial infarction. New Eng J Med. 2006;354:1578–88.
The Heart Outcomes Prevention Evaluation (HOPE) 2 Investigators. Homocysteine lowering with folic acid and B vitamins in vascular disease. New Engl J Med. 2006;354:1567–77.
Flanchbaum L, Belsley S, Drake V, et al. Preoperative nutritional status of patients undergoing Roux-en-Y gastric bypass for morbid obesity. J Gastrointest Surg. 2006;10:1033–7.
Acknowledgments
Statistical analysis of data performed by Dr. Rene Paulson was appreciated.
Support
This project was funded in part by a Chancellor’s Research Fellowship from Texas Woman’s University. Multivitamin supplements were donated by Celebrate®.
Conflict of Interest
Carolyn E. Moore and Vadim Sherman declare they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moore, C.E., Sherman, V. Effectiveness of B Vitamin Supplementation Following Bariatric Surgery: Rapid Increases of Serum Vitamin B12 . OBES SURG 25, 694–699 (2015). https://doi.org/10.1007/s11695-014-1441-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1441-5