Abstract
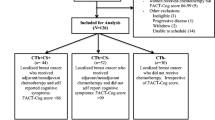
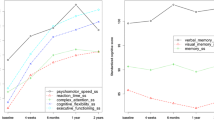
Neural dysfunction and cognitive complaints are associated with chemotherapy for breast cancer although trajectory and contributory factors remain unclear. We prospectively examined neurocognition using fMRI and self-reported cognitive, physical and psychological symptoms in women treated with adjuvant chemotherapy over one year. Patients treated with (n = 28) or without (n = 34) chemotherapy for localized breast cancer and healthy controls (n = 30) performed a Verbal Working Memory Task (VWMT) during fMRI and provided self-reports at baseline (pre-adjuvant treatment), five- (M5) and 12-months (M12). Repeated measures ANOVA and multivariable regression determined change over time and possible predictors (e.g., hemoglobin, physical symptoms, worry) of VWMT performance, fMRI activity in the frontoparietal executive network, and cognitive complaints at M12. Trajectories of change in VWMT performance for chemotherapy and healthy control groups differed significantly with the chemotherapy group performing worse at M12. Chemotherapy patients had persistently higher spatial variance (neural inefficiency) in executive network fMRI-activation than both other groups from baseline to M12. Cognitive complaints were similar among groups over time. At M12, VWMT performance and executive network spatial variance were each independently predicted by chemotherapy treatment and their respective baseline values, while cognitive complaints were predicted by baseline level, physical symptoms and worry. Executive network inefficiency and neurocognitive performance deficits pre-adjuvant treatment predict cognitive dysfunction one-year post-baseline, particularly in chemotherapy-treated patients. Persistent cognitive complaints are linked with physical symptom severity and worry regardless of treatment. Pre-chemotherapy interventions should target both neurocognitive deficits and symptom burden to improve cognitive outcomes for breast cancer survivors.




Similar content being viewed by others
References
Ahles, T. A., Saykin, A. J., McDonald, B. C., Li, Y., Furstenberg, C. T., Hanscom, B. S., et al. (2010). Longitudinal assessment of cognitive changes associated with adjuvant treatment for breast cancer: impact of age and cognitive reserve. Journal of Clinical Oncology, 28(29), 4434–4440. doi:10.1200/JCO.2009.27.0827.
Askren, M. K., Jung, M., Berman, M. G., Zhang, M., Therrien, B., Peltier, S., et al. (2014). Neuromarkers of fatigue and cognitive complaints following chemotherapy for breast cancer: a prospective fMRI investigation. Breast Cancer Research and Treatment, 147(2), 445–455. doi:10.1007/s10549-014-3092-6.
Berman, M. G., Nee, D. E., Casement, M., Kim, H. S., Deldin, P., Kross, E., et al. (2011). Neural and behavioral effects of interference resolution in depression and rumination. Cognitive, Affective, & Behavioral Neuroscience, 11(1), 85–96. doi:10.3758/s13415-010-0014-x.
Berman, M. G., Askren, M. K., Jung, M., Therrien, B., Peltier, S., Noll, D. C., et al. (2014). Pretreatment worry and neurocognitive responses in women with breast cancer. Health Psychology, 33(3), 222–231. doi:10.1037/a0033425.
Cella, D., Land, S. R., Chang, C. H., Day, R., Costantino, J. P., Wolmark, N., et al. (2008). Symptom measurement in the Breast Cancer Prevention Trial (BCPT) (P-1): psychometric properties of a new measure of symptoms for midlife women. Breast Cancer Research and Treatment, 109(3), 515–526. doi:10.1007/s10549-007-9682-9.
Churchill, N. W., Cimprich, B., Askren, M. K., Reuter-Lorenz, P. A., Jung, M. S., Peltier, S., et al. (2014). Scale-free brain dynamics under physical and psychological distress: Pre-treatment effects in women diagnosed with breast cancer. Human Brain Mapping, 36(3), 1077–1092. doi:10.1002/hbm.22687.
Cimprich, B., & Ronis, D. L. (2001). Attention and symptom distress in women with and without breast cancer. Nursing Research, 50(2), 86–94.
Cimprich, B., & Ronis, D. L. (2003). An environmental intervention to restore attention in women with newly diagnosed breast cancer. Cancer Nursing, 26(4), 284–292.
Cimprich, B., So, H., Ronis, D. L., & Trask, C. (2005). Pre-treatment factors related to cognitive functioning in women newly diagnosed with breast cancer. Psychooncology, 14(1), 70–78. doi:10.1002/pon.821.
Cimprich, B., Reuter-Lorenz, P., Nelson, J., Clark, P. M., Therrien, B., Normolle, D., et al. (2010). Prechemotherapy alterations in brain function in women with breast cancer. Journal of Clinical and Experimental Neuropsychology, 32(3), 324–331. doi:10.1080/13803390903032537.
Cimprich, B., Visovatti, M., & Ronis, D. L. (2011). The attentional function index–a self-report cognitive measure. Psychooncology, 20(2), 194–202. doi:10.1002/pon.1729.
Covin, R., Ouimet, A. J., Seeds, P. M., & Dozois, D. J. (2008). A meta-analysis of CBT for pathological worry among clients with GAD. Journal of Anxiety Disorders, 22(1), 108–116. doi:10.1016/j.janxdis.2007.01.002.
Deprez, S., Amant, F., Smeets, A., Peeters, R., Leemans, A., Van Hecke, W., et al. (2012). Longitudinal assessment of chemotherapy-induced structural changes in cerebral white matter and its correlation with impaired cognitive functioning. Journal of Clinical Oncology, 30(3), 274–281. doi:10.1200/JCO.2011.36.8571.
Early Breast Cancer Trialists’ Collaborative Group, Peto, R., Davies, C., Godwin, J., Gray, R., Pan, H. C., et al. (2012). Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100,000 women in 123 randomised trials. Lancet, 379(9814), 432–444. doi:10.1016/S0140-6736(11)61625-5.
Fan, H. G., Houédé-Tchen, N., Yi, Q. L., Chemerynsky, I., Downie, F. P., Sabate, K., et al. (2005). Fatigue, menopausal symptoms, and cognitive function in women after adjuvant chemotherapy for breast cancer: 1- and 2-year follow-up of a prospective controlled study. Journal of Clinical Oncology, 23(31), 8025–8032. doi:10.1200/JCO.2005.01.6550.
Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189–198.
Ganz, P. A., Kwan, L., Stanton, A. L., Bower, J. E., & Belin, T. R. (2011). Physical and psychosocial recovery in the year after primary treatment of breast cancer. Journal of Clinical Oncology, 29(9), 1101–1109. doi:10.1200/JCO.2010.28.8043.
Given, C. W., Sikorskii, A., Tamkus, D., Given, B., You, M., McCorkle, R., et al. (2008). Managing symptoms among patients with breast cancer during chemotherapy: results of a two-arm behavioral trial. Journal of Clinical Oncology, 26(36), 5855–5862. doi:10.1200/JCO.2008.16.8872.
Hermelink, K., Küchenhoff, H., Untch, M., Bauerfeind, I., Lux, M. P., Bühner, M., et al. (2010). Two different sides of ‘chemobrain’: determinants and nondeterminants of self-perceived cognitive dysfunction in a prospective, randomized, multicenter study. Psychooncology, 19(12), 1321–1328. doi:10.1002/pon.1695.
Janelsins, M. C., Kesler, S. R., Ahles, T. A., & Morrow, G. R. (2014). Prevalence, mechanisms, and management of cancer-related cognitive impairment. International Review of Psychiatry, 26(1), 102–113. doi:10.3109/09540261.2013.864260.
Jansen, C. E., Miaskowski, C., Dodd, M., Dowling, G., & Kramer, J. (2005). A metaanalysis of studies of the effects of cancer chemotherapy on various domains of cognitive function. Cancer, 104(10), 2222–2233. doi:10.1002/cncr.21469.
Jenkins, V., Shilling, V., Deutsch, G., Bloomfield, D., Morris, R., Allan, S., et al. (2006). A 3-year prospective study of the effects of adjuvant treatments on cognition in women with early stage breast cancer. British Journal of Cancer, 94(6), 828–834. doi:10.1038/sj.bjc.6603029.
Jenkinson, M., Bannister, P., Brady, M., & Smith, S. (2002). Improved optimization for the robust and accurate linear registration and motion correction of brain images. Neuroimage, 17(2), 825–841.
Kelly, W. E. (2004). A brief measure of general worry: the three item worry index. North American Journal of Psychology, 6(2), 219–226.
Kroenke, K., Strine, T. W., Spitzer, R. L., Williams, J. B., Berry, J. T., & Mokdad, A. H. (2009). The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders, 114(1–3), 163–173. doi:10.1016/j.jad.2008.06.026.
Lazar, N. A., Eddy, W. F., Genovese, C. R., & Welling, J. (2001). Statistical issues in fMRI for brain imaging. International Statistical Review, 69, 105–127.
Lehto, R. H., & Cimprich, B. (2009). Worry and the formation of cognitive representations of illness in individuals undergoing surgery for suspected lung cancer. Cancer Nursing, 32(1), 2–10. doi:10.1097/01.NCC.0000343363.75752.f1.
Lund, T. E., Nørgaard, M. D., Rostrup, E., Rowe, J. B., & Paulson, O. B. (2005). Motion or activity: their role in intra- and inter-subject variation in fMRI. Neuroimage, 26(3), 960–964. doi:10.1016/j.neuroimage.2005.02.021.
McDonald, B. C., Conroy, S. K., Ahles, T. A., West, J. D., & Saykin, A. J. (2012). Alterations in brain activation during working memory processing associated with breast cancer and treatment: a prospective functional magnetic resonance imaging study. Journal of Clinical Oncology, 30(20), 2500–2508. doi:10.1200/JCO.2011.38.5674.
Menning, S., de Ruiter, M. B., Veltman, D. J., Koppelmans, V., Kirschbaum, C., Boogerd, W., et al. (2015). Multimodal MRI and cognitive function in patients with breast cancer prior to adjuvant treatment–the role of fatigue. Neuroimage: Clinical, 7, 547–554. doi:10.1016/j.nicl.2015.02.005.
Mišić, B., Fatima, Z., Askren, M. K., Buschkuehl, M., Churchill, N., Cimprich, B., et al. (2014). The functional connectivity landscape of the human brain. PloS One, 9(10), e111007. doi:10.1371/journal.pone.0111007.
Myers, J. S. (2012). Chemotherapy-related cognitive impairment: the breast cancer experience. Oncology Nursing Forum, 39(1), E31–E40. doi:10.1188/12.ONF.E31-E40.
Nelson, J. K., Reuter-Lorenz, P. A., Sylvester, C. Y., Jonides, J., & Smith, E. E. (2003). Dissociable neural mechanisms underlying response-based and familiarity-based conflict in working memory. Proceedings of the National Academy of Sciences, 100(19), 11171–11175. doi:10.1073/pnas.1334125100.
Pullens, M. J., De Vries, J., & Roukema, J. A. (2010). Subjective cognitive dysfunction in breast cancer patients: a systematic review. Psychooncology, 19(11), 1127–1138. doi:10.1002/pon.1673.
Reuter-Lorenz, P. A., & Cimprich, B. (2013). Cognitive function and breast cancer: promise and potential insights from functional brain imaging. Breast Cancer Research and Treatment, 137(1), 33–43. doi:10.1007/s10549-012-2266-3.
Shilling, V., Jenkins, V., Morris, R., Deutsch, G., & Bloomfield, D. (2005). The effects of adjuvant chemotherapy on cognition in women with breast cancer–preliminary results of an observational longitudinal study. Breast, 14(2), 142–150. doi:10.1016/j.breast.2004.10.004.
Smith, S. M. (2002). Fast robust automated brain extraction. Human Brain Mapping, 17(3), 143–155. doi:10.1002/hbm.10062.
Smith, S. M., Jenkinson, M., Woolrich, M. W., Beckmann, C. F., Behrens, T. E., Johansen-Berg, H., et al. (2004). Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage, 23(Suppl 1), S208–S219. doi:10.1016/j.neuroimage.2004.07.051.
Stewart, A., Collins, B., Mackenzie, J., Tomiak, E., Verma, S., & Bielajew, C. (2008). The cognitive effects of adjuvant chemotherapy in early stage breast cancer: a prospective study. Psychooncology, 17(2), 122–130. doi:10.1002/pon.1210.
Von Ah, D., Jansen, C. E., & Allen, D. H. (2014). Evidence-based interventions for cancer- and treatment-related cognitive impairment. Clinical Journal of Oncology Nursing, 18 Suppl, 17–25, doi:10.1188/14.CJON.S3.17-25.
Wefel, J. S., Saleeba, A. K., Buzdar, A. U., & Meyers, C. A. (2010). Acute and late onset cognitive dysfunction associated with chemotherapy in women with breast cancer. Cancer, 116(14), 3348–3356. doi:10.1002/cncr.25098.
Wefel, J. S., Vardy, J., Ahles, T., & Schagen, S. B. (2011). International cognition and cancer task force recommendations to harmonise studies of cognitive function in patients with cancer. The Lancet Oncology, 12(7), 703–708. doi:10.1016/S1470-2045(10)70294-1.
Wood, L. J., & Weymann, K. (2013). Inflammation and neural signaling: etiologic mechanisms of the cancer treatment-related symptom cluster. Current Opinion in Supportive and Palliative Care, 7(1), 54–59. doi:10.1097/SPC.0b013e32835dabe3.
Acknowledgments
This work was supported by the National Institutes of Health R01 NR01039 (BC).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Mi Sook Jung, Min Zhang, Mary K. Askren, Marc G. Berman, Scott Peltier, Daniel F. Hayes, Barbara Therrien, Patricia A. Reuter-Lorenz, and Bernadine Cimprich declare that they have no conflicts of interest.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, and the applicable revisions at the time of the investigation. Informed consent was obtained from all participants included in the study.
Rights and permissions
About this article
Cite this article
Jung, M.S., Zhang, M., Askren, M.K. et al. Cognitive dysfunction and symptom burden in women treated for breast cancer: a prospective behavioral and fMRI analysis. Brain Imaging and Behavior 11, 86–97 (2017). https://doi.org/10.1007/s11682-016-9507-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-016-9507-8