Abstract
Summary
Access to dual-energy X-ray absorptiometry (DXA) scanning varies significantly throughout New Zealand with the majority of scans funded privately or through the health industry. Barriers to access need to be addressed if osteoporosis guidelines are to be implemented across the country equitably, to reduce the incidence and cost of fragility fractures in New Zealand.
Purpose
This study aims (1) to estimate the number of dual-energy X-ray absorptiometry scans performed in New Zealand, (2) to determine funding sources of DXA scans and (3) to determine the level of regional variation in access.
Methods
DXA scan providers in New Zealand were accessed through a nationwide database and asked to provide data on DXA scans performed in 2007. The numbers of DXA scans performed in each District Health Board (DHB) region were calculated by using a funding source and compared with DHB population estimates provided by Statistics New Zealand for 2007.
Results
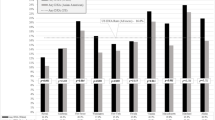
In New Zealand in 2007, 33,104 DXA scans were performed, with a population rate of 78.1 DXA scans per annum per 10,000 general population, significantly less than international guidelines. There were important regional differences in access to DXA scanning. Funding for scans was predominately by private and pharmaceutical industry funders. DHBs funded only 31 % of DXA scans during this time period.
Conclusions
Access to DXA scan technology varies significantly throughout New Zealand, with the majority of DXA scans funded by the private sector or health industry. Barriers to access need to be addressed if osteoporosis guidelines are to be implemented across the country in an equitable fashion and so reduce the incidence and cost of fragility fractures to New Zealand.

Similar content being viewed by others
References
Brown PM, O’Neill R, Leung W, Radwan E, Willingdale J (2011) Current and future economic burden of osteoporosis in New Zealand. Applied Health Economics and Health Policy 9(2):111–23
No author (2003) Prevention and management of osteoporosis. World Health Organ Tech Rep Ser 921:1–164, back cover
Osteoporosis New Zealand. www.bones.org.nz/. [serial on the Internet]
Statistics NZ population projections. Available at: http://www.moh.govt.nz/moh.nsf/indexmh/dhb-faq [database on the Internet]. 2007
Mithal A, Dhingra V, Lau E (2009) The Asian Audit Epidemiology, costs and burden of osteoporosis in Asia 2009, In: International Osteoporosis Foundation. http://www.iofbonehealth.org/download/osteofound/filemanager/publications/pdf/Asian-audit-09/2009-Asian_Audit.pdf
Ewald DP, Eisman JA, Ewald BD, Winzenberg TM, Seibel MJ, Ebeling PR et al (2009) Population rates of bone densitometry use in Australia, 2001–2005, by sex and rural versus urban location. Med J Aust 190(3):126–8
Breakable bones. Osteoporosis Australia Tracking Study 50upcomau/article/2011/09/breakable-bones/ [serial on the Internet]. 2011; Available from: 50up.com.au/article/2011/09/breakable-bones/
Fraser WD (2004) The burden of osteoporosis and the case for disease management. Disease Manag and Health Outcomes 12(6):409–18
Eisman J, Clapham S, Kehoe L (2004) Osteoporosis prevalence and levels of treatment in primary care: the Australian Bone Care Study. J Bone Miner Res 19(12):1969–75
Horne G (2007) Hip fracture management in New Zealand—we need to do better. N Z Med J 120(1254):U2531
(2007) British Orthopaedic Association, British Geriatrics Society. The care of patients with fragility fracture
Marsh D, Akesson K, Beaton DE, Bogoch ER, Boonen S, Brandi ML et al (2011) Coordinator-based systems for secondary prevention in fragility fracture patients. Osteoporos Int 22(7):2051–65
Eisman JA, Bogoch ER, Dell R, Harrington JT, McKinney RE Jr, McLellan A et al (2012) Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res 27(10):2039–46
Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P et al (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35(2):375–82
Port L, Center J, Britta NK, Nguyen T, Cumming R, Eisman J (2003) Osteoporotic fracture: missed opportunity for intervention. Osteoporos Int 14(9):780–4
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15(4):721–39
Pharmaceutical schedule, Wellington: Pharmaceutical Management Agency (2012)
Conflicts of interest
Paul James Mitchell has conflicts of interest. Consultancies are as follows: pharmaceutical manufactures (Amgen, GSK, MSD-NZ, Novartis), charities (National Osteoporosis Society (UK), Osteoporosis Australia, International Osteoporosis Foundation), public bodies (Department of Health in England, National Hip Fracture Database (UK), ANZ Hip Fracture Registry, Health Quality Safety Commission New Zealand) and others (Board Member of Osteoporosis New Zealand (pro-bono). All other authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Milsom, S., Leung, W., Twigden, V. et al. Does insufficient access to dual-energy X-ray absorptiometry (DXA) stifle the provision of quality osteoporosis care in New Zealand?. Arch Osteoporos 8, 120 (2013). https://doi.org/10.1007/s11657-013-0120-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-013-0120-9